Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7256
Peer-review started: November 9, 2021
First decision: March 3, 2022
Revised: April 7, 2022
Accepted: June 4, 2022
Article in press: June 4, 2022
Published online: July 26, 2022
Processing time: 243 Days and 19.8 Hours
Sleep disturbance on the first postoperative night commonly develops for patients after day surgeries. The choice of either total intravenous anesthesia by propofol or total inhalation anesthesia with sevoflurane has become an issue for preventing sleep disturbance.
To compare sleep quality on the first postoperative night for female patients after total intravenous anesthesia by propofol and total inhalation anesthesia with sevoflurane.
We enrolled 61 American Society of Anesthesia (ASA) class I-II outpatients who underwent minor gynecologic surgeries by either propofol or sevoflurane anesthesia. Sleep quality of the very night was assessed by the Pittsburgh Sleep Quality Index (PSQI) on the next day, and PSQI scores were compared by the Wilcoxon signed-rank test and paired t-test pre-operatively and postoperatively.
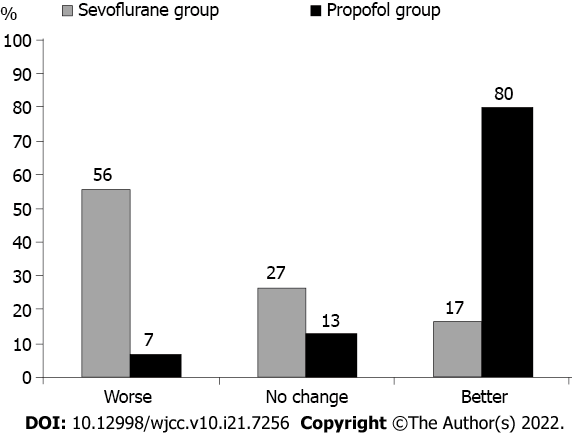
For the propofol group, the mean postoperative global PSQI score (3.3 ± 1.3) was lower than the mean preoperative global PSQI score (4.9 ± 2.3) (P < 0.001); for the sevoflurane group, the mean postoperative global PSQI score (6.5 ± 2.8) was higher than the mean preoperative global PSQI score (5.5 ± 3.2) (P = 0.02). Eighty percent of patients receiving propofol anesthesia subjectively reported improved sleep quality, but only 17% of patients receiving sevoflurane anesthesia reported improved sleep quality.
Sleep quality assessed by the PSQI is better improved in ASA class I-II female patients receiving propofol anesthesia other than sevoflurane anesthesia for undergoing minor gynecologic surgeries.
Core Tip: Total intravenous anesthesia by propofol and total inhalation anesthesia by sevoflurane both were feasible for patients undergoing minor gynecologic surgeries. Eighty percent of patients receiving propofol anesthesia subjectively reported improved sleep quality on the first night. Sleep quality assessed by the Pittsburgh Sleep Quality Index was better improved in American Society of Anesthesia class I-II female patients receiving propofol anesthesia other than sevoflurane anesthesia.
- Citation: Hu CH, Chou WY. Improved Pittsburgh Sleep Quality Index scores on first postoperative night achieved by propofol anesthesia in patients undergoing ambulatory gynecologic surgery. World J Clin Cases 2022; 10(21): 7256-7264
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7256.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7256
Previous studies reported that postoperative sleep disruptions are common regardless of the type of surgery, especially on the first night[1,2]. For most patients, the postoperative sleep pattern changed, of which the total sleep time was reduced by up to 80% and the sleep cycle was fragmented with numerous movement arousals and spontaneous awakenings[2].
Increasing evidence provides confirmation that some of minor surgical procedures or even major pathology operated by minimally invasive endoscopic procedures could safely and successfully be undertaken on a day-surgery basis[3]. Better satisfaction is crucial to the continuing success of day surgery[4,5]. Since the postoperative sleep deprivation was observed for considerable surgical patients during the early postoperative period, more attention should be paid to sleep disorders that are easy to occur due to the influence of psychological factors, surgical trauma, and postoperative pain[6]. We therefore intended to seek an effective way to avoid sleep disturbance for patients undergoing day surgeries.
Propofol is an ultra-short-acting intravenous anaesthesia drug for anaesthesia induction and maintenance that was commonly administered in total intravenous anesthesia (TIVA) with the advantages of rapid onset, easy control, and reasonable safety[7,8]. In addition, a previous study[9] observed that the propofol-based TIVA has limited effect on early postoperative sleep disorders assessed by the Pittsburgh Sleep Quality Index (PSQI)[10]. However, the utilization of propofol in treating insomnia or sleep disturbance remains controversial on account of previously reported accidental mortalities[11,12]. Sevoflurane is a popular anesthetic agent for ambulatory surgery that provides a safe intraoperative anesthesia with a smooth recovery to meet the need of early discharge from hospital. Nonetheless, no consensus has been achieved regarding its effect on sleep quality yet[13,14].
Considering Enhanced Recovery After Surgery (ERAS) guideline dedicated to standardizing and optimizing perioperative care for women undergoing minimally invasive gynecologic surgery[15], the guideline focuses on workflows important for high-value care in minimally invasive surgery, such as same-day discharge, to elevate the quality and safety of healthcare in clinical practice. Consequently, we initiated this study on female patients of middle age who underwent minor gynecological day-surgery because of benign gynecological disease to compare the impact of between TIVA by propofol and total inhalation anesthesia (TIA) by sevoflurane in preventing sleep disturbance.
Ethical approval for this study (B-ER-108-012-T) was provided by Institutional Review Board of National Cheng Kung University Hospital, Tainan, Taiwan (Chairperson Prof Lin. Thy-Sheng) on January 29, 2019. This study was conducted in accordance with the Declaration of Helsinki.
With the approval from Institutional Review Board of National Cheng Kung University Hospital (B-ER-108-012-T), we conducted this retrospective case-control study by reviewing the pre-operative and postoperative records of each study subject that was operated from March 2019 to December 2019. Eighty patients who underwent a minor gynecological surgery, including hysteroscopy for endometrial biopsy, polypectomy, or cervical conization, were involved in this study. Except patients who had extra sleep before usual bedtime after returning home, we also excluded patients with a history of opioid use or postoperative nausea/vomiting. We therefore enrolled 61 American Society of Anesthesia (ASA) class I-II patients with a mean age of 42.3 years (range: 30-54 years). As a routine postoperative follow-up for patients after discharge from day surgery on the next day, verbal consent instead of written consent was obtained from each patient before inquiry of questionnaire by telephone that was allowed by the Institutional Review Board of National Cheng Kung University Hospital.
As a standard protocol, we used propofol or sevoflurane for general anesthesia. For the propofol group, the general anesthesia was induced by Target Controlled Infusion (Orchestra Base Primea) with an effect-site concentration of propofol 4-5 mcg/mL and adjusted according to the autonomic response to surgical stimulation. For the sevoflurane group, anesthesia was induced with inhaled sevoflurane 3.5%-5%, followed by laryngeal mask insertion at an optimal end-tidal concentration of sevoflurane ventilation with 60% oxygen (oxygen:air = 1:1). The depth of inhaled anesthesia was adjusted to maintain a spontaneous respiration with an end-tidal carbon dioxide partial pressure ranging from 35 to 45 mmHg and adapt to surgical stimulus. The end-tidal CO2 concentration and pulse oximeter were monitored for apnea.
The maintenance of stable vital signs aimed at controlling heart rate and blood pressure within 20% upper or lower of baseline measurement throughout the whole surgical course. Furthermore, mean arterial pressure was kept no less than 60 mmHg by adjusting hydration with Lactate ringer’s solution or intermittent boluses of ephedrine 5-25 mg to treat intraoperative hypotension. At the end of the surgery, the infusion pump was discontinued for the propofol group. As for the sevoflurane group, the supply of inhaled anesthetic was suspended, and fresh gas flows were increased to 10 L/min (air:oxygen = 1:1) for wash-out. The laryngeal mask was removed at 0.4-0.5 MAC (minimal alveolar concentration) and the patient was sent to the recovery room. Acetaminophen 500 mg was given for postoperative pain if the patient requested for analgesia. The patients usually were discharged with recovery of clear consciousness and restoration of independent movements once the patients were well-oriented to request a discharge.
Our anesthetist evaluated each patient’s sleep quality with the PSQI after obtaining oral consent from each patient on the following day. The PSQI evaluates the quality and patterns of sleep[11] with seven sleep components: Sleep duration, sleep disturbance, sleep latency, daytime disturbance, habitual sleep efficiency, sleep quality, and the use of sleep medications. A global score of PSQI is obtained by summing seven PSQI subscales totally.
We used independent t-test for analyzing numerical parameters, including propofol dose (mg), anesthesia time (min), operation time (min), and interval from discharge to sleep at night (min) except the paired t-test for comparing the time of sleep latency and sleep duration. Mann-Whitney U test was adopted for comparing non-parametric data between these two groups. For related samples, the Wilcoxon signed-rank test was used to compare the pre-operative and postoperative PSQI scores. Data analyses were conducted by using SPSS 22 with P < 0.05 considered significant.
Among 61 patients who underwent minor gynecologic surgery, 31 and 30 patients received propofol anesthesia (propofol group) and sevoflurane anesthesia (sevoflurane group), respectively. No statistically significant difference was disclosed regarding the average age, average height, and average weight between two groups (Table 1). With respect to the operative parameters, no statistically significant differences were noticed regarding the average anesthesia duration, average operation time, and average interval from discharge to sleep at night (Table 1).
| Propofol group (n = 31) | Sevoflurane group (n = 30) | P | |
| Height (cm) | 158.6 (± 5.8) | 159.3 (± 5.2) | 0.62 |
| Weight (kg) | 59.6 (± 8.7) | 65.1 (± 14.6) | 0.08 |
| Age (yr) | 43.2 (± 5.9) | 41.3 (± 6.9) | 0.25 |
| Operation time (min) | 50.4 (± 12.6) | 46.3 (± 9.7) | 0.11 |
| Anesthesia time (min) | 65.9 (± 15.1) | 62.5 (± 10.4) | 0.16 |
| Recovery time (min) | 55.0 (± 3.7) | 54.5 (± 4.0) | 0.32 |
| Adverse effect | |||
| Dizziness (patient) | 1 | 2 | |
| Interval from discharge to sleep (min) | 572.2 (± 151.4) | 553.1 (± 138.6) | 0.45 |
Regarding global PSQI scores, no significant difference was found between the propofol group (4.9 ± 2.3) and the sevoflurane group (5.5 ± 3.2) pre-operatively. However, intra-group comparison showed that the postoperative global PSQI score (3.3 ± 1.3) was significantly lower than the preoperatively global PSQI score (4.9 ± 2.3) (P < 0.001) in the propofol group, while the postoperative global PSQI score (6.5 ± 2.8) was significantly higher than the preoperative global PSQI score (5.5 ± 3.2; P = 0.02) in the sevoflurane group.
As for each component of PSQI scores, the postoperative PSQI components of subjective sleep quality, sleep latency, and sleep duration scored significantly lower than preoperative ones (P < 0.001, P = 0.005, and P = 0.001, respectively) in the propofol group. For the sevoflurane group, the postoperative PSQI components of habitual sleep efficiency, step disturbances, and daytime dysfunction scored significantly higher than preoperative ones (P = 0.01, P = 0.01, and P = 0.01, respectively), but the postoperative PSQI component of sleep latency scored significantly lower than preoperative one (P = 0.03) (Table 2).
| Propofol anesthesia (n = 31) | Sevoflurane anesthesia (n = 30) | P | |
| Global PSQI score (before surgery) | 4.9 ± 2.3 | 5.5 ± 3.2 | 0.38 |
| Global PSQI score (after srugery) | 3.3 ± 1.3 | 6.5 ± 2.8 | < 0.001 |
| P < 0.001 | P = 0.02 | ||
| Component 1 | |||
| Subjective sleep quality (before) | 2.3 ± 0.7 | 1.3 ± 0.7 | |
| Subjective sleep quality (after) | 1.7 ± 0.4 | 1.5 ± 0.8 | |
| P < 0.001 | P = 0.13 | ||
| Component 2 | |||
| Sleep latency (before) | 0.5 ± 0.8 | 1.0 ± 1.1 | |
| Sleep latency (after) | 0.2 ± 0.6 | 0.6 ± 0.9 | |
| P = 0.005 | P = 0.03 | ||
| Component 3 | |||
| Sleep duration (before) | 0.6 ± 0.6 | 1.1 ± 1.0 | |
| Sleep duration (after) | 0.2 ± 0.4 | 1.2 ± 1.0 | |
| P = 0.001 | P = 0.77 | ||
| Component 4 | |||
| Habitual sleep efficiency (before) | 0.0 ± 0.2 | 0.4 ± 0.8 | |
| Habitual sleep efficiency (after) | 0.0 ± 0.2 | 1.1 ± 1.2 | |
| P = 1.00 | P = 0.01 | ||
| Component 5 | |||
| Sleep disturbances (before) | 1.0 ± 0.0 | 0.8 ± 0.4 | |
| Sleep disturbances (after) | 1.0 ± 0.0 | 1.0 ± 0.3 | |
| P = 1.00 | P = 0.01 | ||
| Component 6 | |||
| Use of sleeping medication (before) | 0.3 ± 0.8 | 0.1 ± 0.5 | |
| Use of sleeping medication (after) | 0.0 ± 0.2 | 0.0 ± 0.0 | |
| P = 0.06 | P = 0.32 | ||
| Component 7 | |||
| Daytime dysfunction (before) | 1.0 ± 0.0 | 0.8 ± 0.4 | |
| Daytime dysfunction (after) | 1.0 ± 0.0 | 1.1 ± 0.5 | |
| P = 1.00 | P = 0.01 |
For the group of propofol anesthesia, we observed that the time of postoperative sleep latency (7.6 ± 27.6 min) was significantly shorter than the preoperative sleep latency (15.6 ± 24.1 min). The time of postoperative sleep duration (8.1 ± 1.2 h) was significantly longer than the preoperative sleep duration (7.2 ± 0.9 h) (Table 3).
| Preoperative | Postoperative | 95% confidence interval | P | |
| Sleep latency (min) | 15.6 ± 24.1 | 7.6 ± 27.6 | 2.5 to 13.7 | 0.006 |
| Sleep duration (h) | 7.2 ± 0.9 | 8.1 ± 1.2 | -1.4 to -0.5 | < 0.001 |
For the group of sevoflurane anesthesia, the mean scores of postoperative habitual sleep efficiency and sleep disturbance were significantly more than the preoperative ones despite having a shorter average sleep latency (18.8 ± 16.1 vs 25.4 ± 20.9 min) (Table 4). Most patients complained that their sleep was fragmented with movement arousals and long periods of spontaneous awakenings. As for the mean score of having trouble staying awake, the postoperative score (0.5 ± 0.6) was significantly higher than the preoperative score (0.1 ± 0.3; P = 0.001); the mean score of keeping up enough enthusiasm to get things done postoperatively (1.4 ± 0.6) was significantly higher than the preoperative score (0.7 ± 0.4; P < 0.001) (Table 4).
| Preoperative | Postoperative | 95% confidence interval | P | |
| Sleep latency (min) | 25.4 ± 20.9 | 18.8 ± 16.1 | -7.4 to 13.8 | 0.08 |
| Trouble staying awake (sum of question scores) | 0.1 ± 0.3 | 0.5 ± 0.6 | -0.6 to -0.2 | 0.001 |
| Enough enthusiasm (sum of question scores) | 0.7 ± 0.4 | 1.4 ± 0.6 | -0.9 to -0.4 | < 0.001 |
In this study, 80% of patients after propofol anesthesia for day surgery reported improved sleep quality and only 7% reported a worse sleep quality. While being compared with the baseline sleep data before anesthesia, only 17% of the patients reported improved sleep quality and 56% reported a worse sleep quality in the sevoflurane group (Figure 1).
By comparing PSQI scores on the first night among 61 female patients undergoing day surgeries for minor gynecological pathology, 80% of the patients after propofol anesthesia reported improved sleep quality, while 57% of the patients after sevoflurane anesthesia reported a worse sleep quality. In this study, we found that the postoperative global PSQI score was significantly lower than the preoperative global PSQI score after propofol anesthesia (P < 0.001). Multiple components of PSQI including subjective sleep quality, sleep latency, and sleep duration improved postoperatively as well (P < 0.003) (Table 2). On the other hand, the postoperative score of global PSQI was significantly worse than the global PSQI score preoperatively in the sevoflurane group, especially in the PSQI components of habitual sleep efficiency, sleep disturbances, and daytime dysfunction.
The unfavorable factors of sleep disturbances include pain, psychological stresses, age, magnitude of surgery, operation procedure, inflammation reaction, increased sympathetic activity, endocrine response to surgery, and environmental accommodation[2]. A multicenter cross-sectional study containing 434 patients after excluding 9 patients without complete follow-up also disclosed that two most common factors causing poor postoperative sleep quality were depression and young age between 25-54 years old[16]. Another study investigated patients undergoing hip replacement reported the PSQI scores significantly correlated with pre-operative sleep quality and the postoperative consumption of analgesics[17]. The major surgery implied bigger operative trauma that caused worse quality of sleep by greater suppression of rapid eye movement (REM) sleep[18]. Through fast-track arrangement of joint replacement operations, the patients reported more waking-up times because of pain[19]. Different types of surgeries have varied effects on patients' sleep quality. We therefore recruited female patients of middle age undergoing minor gynecological surgeries for this study in order to prevent possible confounding factors such as hormone shifting, aging, and extreme pain that would inadvertently affect the sleep quality[20,21].
Among currently used scales for assessing sleep quality, like the PSQI questionnaire, Insomnia Severity Index, Athens Insomnia Scale, Epworth Sleepiness Scale, and General Sleep Disturbance Scale, the most commonly used assessment is PSQI on account of high reliability and validity[22]. The PSQI contains 19 self-rated questions and 5 questions rated by the bed partner or roommate. The scoring contained only self-rated questions. Although the PSQI was not designed for assessing a single night sleep, we adopted it in consideration of its simplicity to be easily communicated between the investigators and the patients.
The intravenous anesthesia with propofol was adjusted according to the change in vital sign or surgical stimuli[23]. The patient usually recovers soon after the infusion pauses. It has therefore become a popular method of anesthesia for middle-aged female patients of ASAI-II status who received a minor gynecologic surgery. For the sevoflurane group, the dose was adjusted in a similar way as the propofol use. Patients also recover rapidly after the pauses of inhalation in a few minutes. However, the disproportionate recovery of homeostasis caused by sevoflurane inhalation on either non-REM (NREM) or REM could be fairly obvious. Sevoflurane exposure may increase NREM sleep and produce a significant decrease in the NREM sleep during the post-anesthetic period, but did not satisfy the homeostatic need for REM sleep[24]. Consequently, it accounted for fragmented sleep and spontaneous awakenings except having trouble staying awake in activity postoperatively causing daytime dysfunction, and subsequently being unable to keep up enough enthusiasm to get things done postoperatively[13].
Recently, a study by Ding et al[9] also indicated that propofol-based TIVA may effectively reduce the incidence of sleep disorders by inhibiting the release of cortisol and other inflammatory factors in addition to activating the secretion of melatonin. Although propofol anesthesia is not a real sleep state, some components of postoperative PSQI score might be affected by the residual effect of propofol after several half-lives of elimination that was supposed to be a very low plasma concentration. Regarding the mechanism of propofol in improving sleep quality, Boveroux et al[25] performed the blood oxygen level-dependent functional magnetic resonance imaging (fMRI-BOLD) in healthy human in states of wakefulness and sedation induced by propofol. Their study disclosed that higher dose of propofol negatively correlates with the functional connectivity within certain thalamocortical and higher association corticocortical networks. Propofol is a commonly used ultra-short-acting intravenous anaesthesia drug that integrates several advantages of intravenous anaesthetics, including rapid onset, quick analgesia, short recovery time, quick recovery of physiological function, good controllability, and high safety. Moreover, Murphy et al[26] used high-density electroencephalography (hd-EEG) to investigate the cortical reactions with propofol anesthesia. They found that slow waves in propofol anesthesia are associated with diminished consciousness. Namely, propofol anesthesia seemed to be a sleep-like state[27]. Except electrophyiological finding of EEG and image evidence of functional MRI of the brain, better sleep quality after propofol anesthesia was also supported by biochemical examination. A study collecting sleep quality parameters on the first night after selective laparoscopic surgery for 74 patients by wireless portable sleep monitor disclosed that patients who underwent sevoflurane anesthesia reported dreaming more frequently than patients anesthetized by TIVA with propofol. As a consequence, postoperative REM sleep was also higher in the sevoflurane anesthesia group than in the propofol group. The potential mechanism was supposed to be that volatile anesthetic could not regulate sleep homeostasis between NREM and REM sleep[28].
We did notice several limitations of this study during handling the study data and preparing the manuscript. We collected the PSQI questionnaire by telephone inquiry instead of interview in person. Some ambiguity in answering by the patient could cause trivial bias in deciding the score by the investigator due to a lack of on-site re-confirmation by the patient. Consequently, we had tried to attenuate the influence by second questioning before completion of the questionnaire. Even though we chose female patients undergoing minor gynecological procedures in consideration of less effect on sleep quality by postoperative pain, a lack of pain assessment could not eliminate the readers’ doubt regarding the negative effect on sleep quality that might result in an unfair comparison between the propofol group and sevoflurane group. We therefore routinely prescribed acetaminophen for pain relief. Although the PSQI is commonly adopted for evaluation of sleep quality, its reliability fits better for mid-term or long-term assessment instead of single night sleep. However, its simplicity still deserves a recommendation on account of less difficulty in communication between investigators and study subjects.
In comparison with sevoflurane anesthesia, propofol anesthesia significantly improves the sleep quality on the first postoperative night assessed by the PSQI in ASA I-II female patients who underwent minor gynecologic surgery.
For most patients, postoperative sleep disruptions are common regardless of the type of surgery, especially on the first night.
Since the postoperative sleep deprivation was observed for considerable surgical patients during the early postoperative period, we therefore intended to seek an effective way to avoid sleep disturbance for patients undergoing day surgeries.
We initiated this study on female patients of middle age who underwent minor gynecological day-surgery because of benign gynecological disease to compare the impact of total intravenous anesthesia by propofol and total inhalation anesthesia by sevoflurane in preventing sleep disturbance.
We enrolled 61 American Society of Anesthesia (ASA) class I-II outpatients who underwent minor gynecologic surgeries by either propofol or sevoflurane anesthesia. Sleep quality evaluated by the Pittsburgh Sleep Quality Index (PSQI) on the first night of the ambulatory surgery was compared.
For the propofol group, the mean postoperative global PSQI score (3.3 ± 1.3) was lower than the mean preoperative global PSQI score (4.9 ± 2.3; P < 0.001); for the sevoflurane group, the mean postoperative global PSQI score (6.5 ± 2.8) was higher than the mean preoperative global PSQI score (5.5 ± 3.2; P = 0.02).
Sleep quality assessed by the PSQI is better improved in ASA class I-II female patients receiving propofol anesthesia other than sevoflurane anesthesia for undergoing minor gynecologic surgeries.
Total intra-venous anesthesia by propofol is recommended to be applied for same day ambulatory surgery for different surgical procedures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Song J, China S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Wu YXJ
| 1. | Rosenberg-Adamsen S, Kehlet H, Dodds C, Rosenberg J. Postoperative sleep disturbances: mechanisms and clinical implications. Br J Anaesth. 1996;76:552-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 150] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Dolan R, Huh J, Tiwari N, Sproat T, Camilleri-Brennan J. A prospective analysis of sleep deprivation and disturbance in surgical patients. Ann Med Surg (Lond). 2016;6:1-5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 3. | Gupta A. Evidence-based medicine in day surgery. Curr Opin Anaesthesiol. 2007;20:520-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Majholm B, Engbæk J, Bartholdy J, Oerding H, Ahlburg P, Ulrik AM, Bill L, Langfrits CS, Møller AM. Is day surgery safe? Acta Anaesthesiol Scand. 2012;56:323-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Mitchell M. Home recovery following day surgery: a patient perspective. J Clin Nurs. 2015;24:415-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Yu J, Rawtaer I, Fam J, Jiang MJ, Feng L, Kua EH, Mahendran R. Sleep correlates of depression and anxiety in an elderly Asian population. Psychogeriatrics. 2016;16:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 125] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 7. | White PF. Propofol: its role in changing the practice of anesthesia. Anesthesiology. 2008;109:1132-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Chaudhri S, White M, Kenny GN. Induction of anaesthesia with propofol using a target-controlled infusion system. Anaesthesia. 1992;47:551-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Ding F, Wang X, Zhang L, Li J, Liu F, Wang L. Effect of propofol-based total intravenous anaesthesia on postoperative cognitive function and sleep quality in elderly patients. Int J Clin Pract. 2021;75:e14266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 21998] [Article Influence: 611.1] [Reference Citation Analysis (0)] |
| 11. | Garcia-Guasch R, Roigé J, Padrós J. Substance abuse in anaesthetists. Curr Opin Anaesthesiol. 2012;25:204-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Wischmeyer PE, Johnson BR, Wilson JE, Dingmann C, Bachman HM, Roller E, Tran ZV, Henthorn TK. A survey of propofol abuse in academic anesthesia programs. Anesth Analg. 2007;105:1066-1071, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Brioni JD, Varughese S, Ahmed R, Bein B. A clinical review of inhalation anesthesia with sevoflurane: from early research to emerging topics. J Anesth. 2017;31:764-778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 127] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 14. | Chen WS, Chiang MH, Hung KC, Lin KL, Wang CH, Poon YY, Luo SD, Wu SC. Adverse respiratory events with sevoflurane compared with desflurane in ambulatory surgery: A systematic review and meta-analysis. Eur J Anaesthesiol. 2020;37:1093-1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Stone R, Carey E, Fader AN, Fitzgerald J, Hammons L, Nensi A, Park AJ, Ricci S, Rosenfield R, Scheib S, Weston E. Enhanced Recovery and Surgical Optimization Protocol for Minimally Invasive Gynecologic Surgery: An AAGL White Paper. J Minim Invasive Gynecol. 2021;28:179-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 16. | Seid Tegegne S, Fenta Alemnew E. Postoperative poor sleep quality and its associated factors among adult patients: A multicenter cross-sectional study. Ann Med Surg (Lond). 2022;74:103273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Luo ZY, Li LL, Wang D, Wang HY, Pei FX, Zhou ZK. Preoperative sleep quality affects postoperative pain and function after total joint arthroplasty: a prospective cohort study. J Orthop Surg Res. 2019;14:378. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 71] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 18. | Wu XH, Cui F, Zhang C, Meng ZT, Wang DX, Ma J, Wang GF, Zhu SN, Ma D. Low-dose Dexmedetomidine Improves Sleep Quality Pattern in Elderly Patients after Noncardiac Surgery in the Intensive Care Unit: A Pilot Randomized Controlled Trial. Anesthesiology. 2016;125:979-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 19. | Krenk L, Jennum P, Kehlet H. Sleep disturbances after fast-track hip and knee arthroplasty. Br J Anaesth. 2012;109:769-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 20. | Eichling PS, Sahni J. Menopause related sleep disorders. J Clin Sleep Med. 2005;1:291-300. [PubMed] |
| 21. | Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255-1273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1891] [Cited by in RCA: 2143] [Article Influence: 107.2] [Reference Citation Analysis (0)] |
| 22. | Lin D, Huang X, Sun Y, Wei C, Wu A. Perioperative Sleep Disorder: A Review. Front Med (Lausanne). 2021;8:640416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 23. | Schüttler J, Ihmsen H. Population pharmacokinetics of propofol: a multicenter study. Anesthesiology. 2000;92:727-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 246] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 24. | Pal D, Lipinski WJ, Walker AJ, Turner AM, Mashour GA. State-specific effects of sevoflurane anesthesia on sleep homeostasis: selective recovery of slow wave but not rapid eye movement sleep. Anesthesiology. 2011;114:302-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Boveroux P, Vanhaudenhuyse A, Bruno MA, Noirhomme Q, Lauwick S, Luxen A, Degueldre C, Plenevaux A, Schnakers C, Phillips C, Brichant JF, Bonhomme V, Maquet P, Greicius MD, Laureys S, Boly M. Breakdown of within- and between-network resting state functional magnetic resonance imaging connectivity during propofol-induced loss of consciousness. Anesthesiology. 2010;113:1038-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 443] [Cited by in RCA: 475] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 26. | Murphy M, Bruno MA, Riedner BA, Boveroux P, Noirhomme Q, Landsness EC, Brichant JF, Phillips C, Massimini M, Laureys S, Tononi G, Boly M. Propofol anesthesia and sleep: a high-density EEG study. Sleep. 2011;34:283-91A. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 284] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 27. | Chamberlin NL, Eikermann M. This is no humbug: anesthetic agent-induced unconsciousness and sleep are visibly different. Anesthesiology. 2010;113:1007-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Li S, Song B, Li Y, Zhu J. Effects of Intravenous Anesthetics vs Inhaled Anesthetics on Early Postoperative Sleep Quality and Complications of Patients After Laparoscopic Surgery Under General Anesthesia. Nat Sci Sleep. 2021;13:375-382. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |