Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7130
Peer-review started: January 5, 2022
First decision: February 21, 2022
Revised: March 6, 2022
Accepted: May 27, 2022
Article in press: May 27, 2022
Published online: July 16, 2022
Processing time: 180 Days and 12 Hours
Portal vein thrombosis (PVT) is a condition caused by hemodynamic disorders. It may be noted in the portal vein system when there is an inflammatory stimulus in the abdominal cavity. However, PVT is rarely reported after hepatectomy. At present, related guidelines and major expert opinions tend to consider vitamin K antagonists or low-molecular weight heparin (LMWH) as the standard treatment. But based on research, direct oral anticoagulants may be more effective and safe for noncirrhotic PVT and are also beneficial by reducing the recurrence rate of PVT.
A 51-year-old woman without any history of disease felt discomfort in her right upper abdomen for 20 d, with worsening for 7 d. Contrast-enhanced computed tomography (CECT) of the upper abdomen showed right liver intrahepatic cholangiocarcinoma with multiple intrahepatic metastases but not to the left liver. Therefore, she underwent right hepatic and caudate lobectomy. One week after surgery, the patient underwent a CECT scan, due to nausea, vomiting, and abdominal distension. Thrombosis in the left branch and main trunk of the portal vein and near the confluence of the splenic vein was found. After using LMWH for 22 d, CECT showed no filling defect in the portal vein system.
Although PVT after hepatectomy is rare, it needs to be prevented during the perioperative period.
Core Tip: We present a case of portal vein thrombosis (PVT) after hemihepatectomy. It is most common in liver cirrhosis, postsplenectomy, and liver transplantation, but is relatively rare after hepatectomy. This case verified the safety and effectiveness of low-molecular weight heparin in this condition. In the perioperative period, attention should be given to the prevention, early diagnosis, and systemic treatment of PVT.
- Citation: Zhang SB, Hu ZX, Xing ZQ, Li A, Zhou XB, Liu JH. Portal vein thrombosis in a noncirrhotic patient after hemihepatectomy: A case report and review of literature. World J Clin Cases 2022; 10(20): 7130-7137
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7130.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7130
Portal vein thrombosis (PVT) is often detected in the extrahepatic portal vein, such as the superior mentraic vein and spleen vein. Vitamin K antagonists (VKAs) or low-molecular weight heparin (LMWH) are considered as the standard treatment[1,2]. But direct oral anticoagulants (DOACs) may be more effective and safe for noncirrhotic PVT (ncPVT) and are also beneficial by reducing the recurrence rate of PVT[3,4]. Portal vein tumor thrombosis is significantly different from PVT[5,6]. Studies show that 2.1%-9.1%[7,8] of patients have PVT after hepatectomy, with a rate of 10%-40%[9-11] among patients with hepatocellular carcinoma. Anticoagulation is widely accepted as the standard treatment option for ncPVT[12-14]. According to the Child–Pugh classification principle, thrombectomy and interventional therapy may have great disadvantages.
A 51-year-old woman without any history of disease felt discomfort in the right upper abdomen for 20 d with worsening for 7 d.
The symptoms were unrelated to feeding behavior, and the patient had not undergone any treatment.
The patient was in good health.
The patient had no medical history or family history of malignant tumors.
The physical examinations were toughly normal.
CA-199 was over 1000 U/mL on admission.
Contrast-enhanced computed tomography (CECT) of the upper abdomen showed right liver intrahepatic cholangiocarcinoma (ICC) with multiple intrahepatic metastases, which were confined to the right liver and caudate lobe.
ICC with multiple intrahepatic metastases in the right liver and caudate lobe.
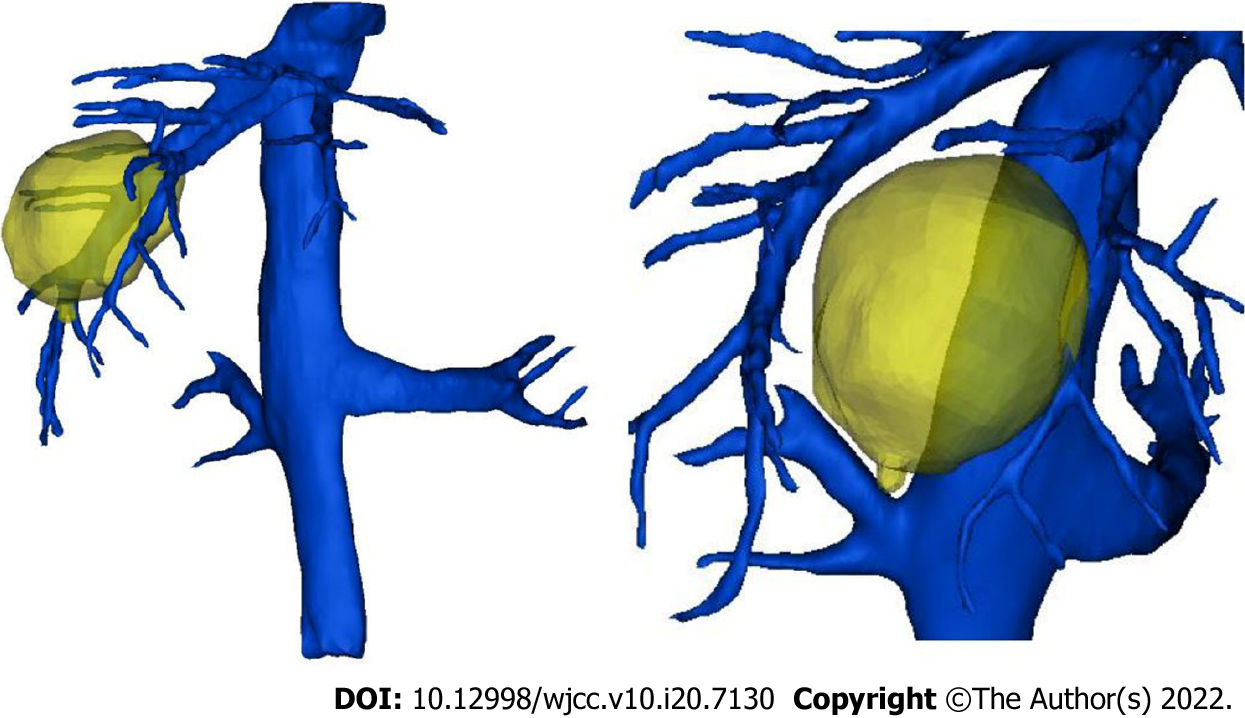
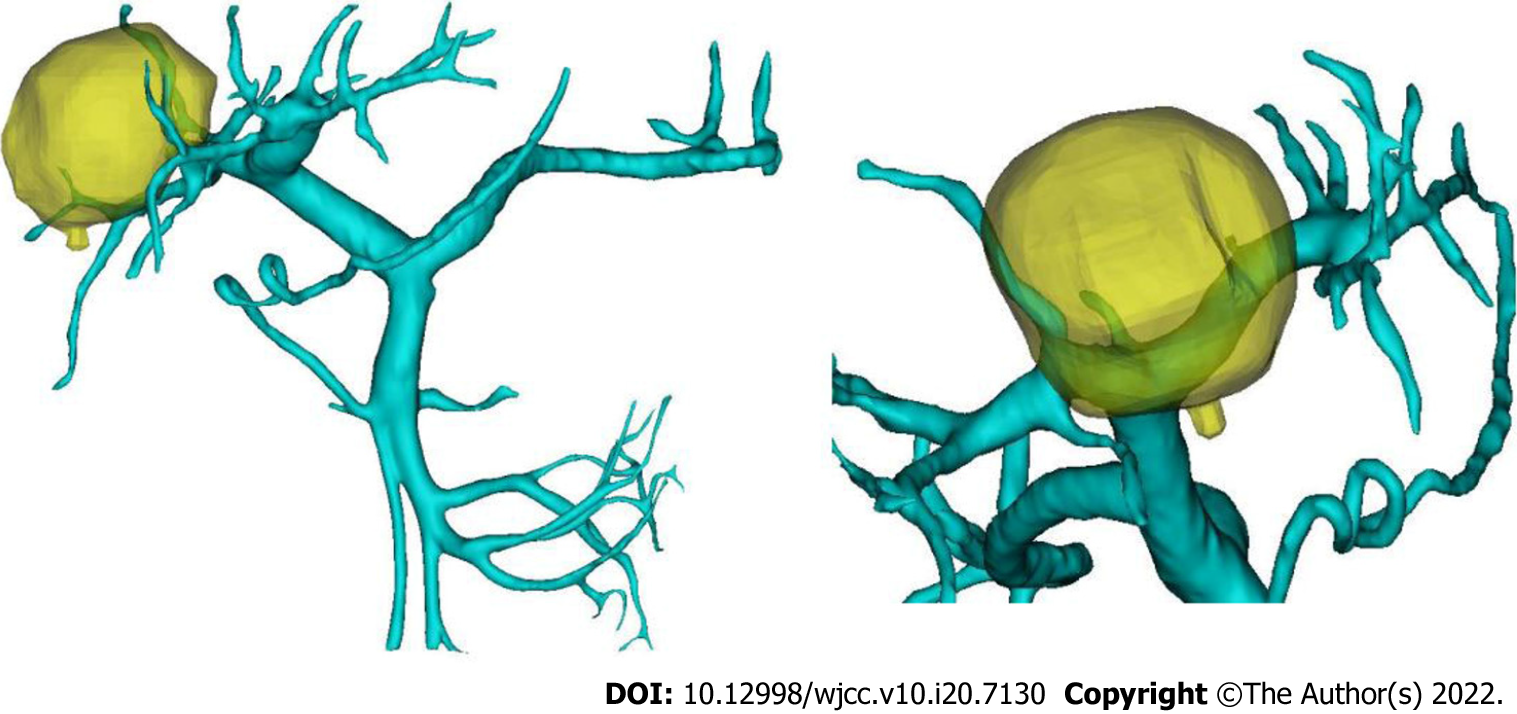
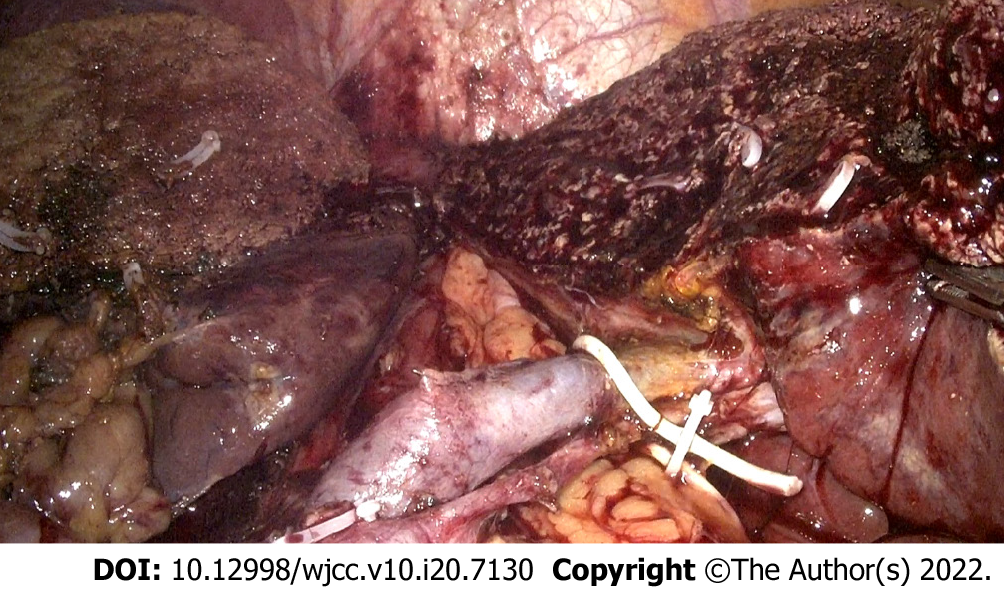
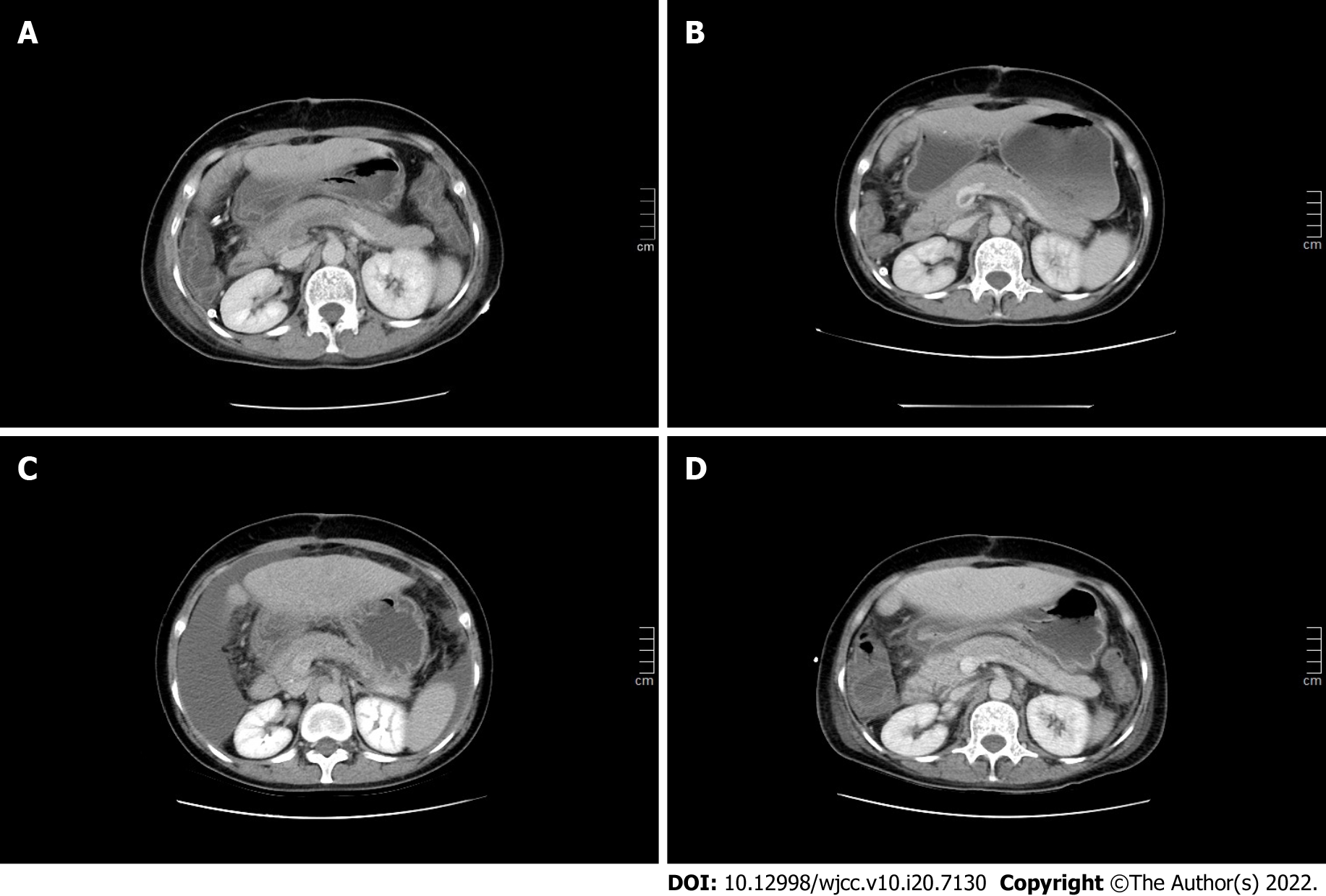
After three-dimensional reconstruction of the liver, we found that the middle hepatic vein (Figure 1) and the right branch of the portal vein (Figure 2) were located close to the tumor. Therefore, we decided to perform laparoscopic left-liver-first anterior radical modular orthotopic right hemihepatectomy (Lap-larmorh) (Figure 3). The right liver and caudate lobe, which accounted for 62% of the liver volume, were resected. After the operation, in addition to antibiotics, hepatic protectants, and proton pump inhibitors, we also intermittently administered fibrinogen, human prothrombin complex concentrates, and ordinary frozen plasma to avoid hemorrhage from the liver wounds. However, one week after surgery, nausea, vomiting, and abdominal distension occurred, and she underwent a CECT scan. Thrombosis was distributed in the left branch and main trunk of the portal vein and near the confluence of the splenic vein. Moreover, the main trunk was almost occluded (Figure 4A). To prevent further progression, we began to inject 6400 IU LMWH twice a day until the PVT disappeared and stopped procoagulant therapy. After the above treatments, the patient’s discomfort was significantly relieved. In addition, CECT and color Doppler ultrasound indicated that the thrombosis was smaller than before (Figure 4B and C). On day 22, CECT showed that there was no filling defect in the portal vein (Figure 4D).
This patient was discharged uneventfully 1 mo after the operation. Nine months of follow-up by telephone showed that there were no recurrent thromboembolic events without anticoagulation therapy. Moreover, there were no symptoms of digestive system discomfort.
As a deep vascular complication, PVT is not common in clinical work. It usually occurs in patients with liver cirrhosis, with an incidence of 10-25%[15-17]. The incidence is closely related to surgery, ranging from 1% to 3%[18] after liver transplantation, and from 1.6 to 11%[19,20] after splenectomy. At present, our department does not provide preventive treatment for thrombosis during the perioperative period. Anticoagulation therapy has no significant effect on the incidence of thrombosis[21].
According to the location of the thrombus, the degree of obstruction, and the speed of obstruction formation, PVT can be divided into the acute phase, subacute phase, and chronic phase. At the onset of the acute phase, the patient will suddenly show symptoms such as nausea, vomiting, abdominal pain, or fever. After hepatectomy, without undergoing portal vein color Doppler ultrasound and CECT, it is difficult to associate these symptoms with acute PVT and make an early diagnosis or start treatment early. If the portal vein is not completely blocked in the acute phase, these symptoms will continue for several weeks and progress to the subacute phase, eventually entering the chronic phase after the formation of venous collateral circulation. The patient gradually developed gastrointestinal symptoms 1 wk after right hepatectomy, which proved that the PVT did not suddenly block most of the main portal vein, which created the possibility for subsequent treatment.
The three basic risk factors for the formation of PVT are vascular endothelial cell damage, blood hypercoagulability, and portal vein blood flow disorder. Reviewing the patient's perioperative treatment, there were the following risk factors that may have led to PVT: (1) Surgical factors, such as intraoperative laparoscopic equipment pulling the portal vein and damaging the vascular endothelial cells, 20 min of treatment by the first hepatic portal blood flow occlusion method causing prolonged hypoxia, and high pneumoperitoneal pressure (15 mmHg)[22,23] causing a reduction in portal blood flow velocity; and (2) After the operation, the patient's effective circulating blood volume was insufficient, and the blood hypercoagulable state was caused by an inflammatory reaction. In addition, an insufficient remaining liver volume after hepatectomy resulted in a fragile balance of the coagulation system. Frozen plasma and other procoagulant drugs infused to prevent hemorrhage from the wound may also have promoted the development of PVT.
At present, the early diagnosis of PVT is based on clinical symptoms and the detection of thrombi through imaging examination. However, approximately 67%[24] of patients have no special clinical manifestations after the formation of PVT. CECT is still the first choice for a clear diagnosis[21,25]. The diagnosis of this patient was achieved through CECT, and in the follow-up process, the combination of CECT and ultrasound also achieved good results.
The purpose of PVT treatment is to prevent the further development of the thrombus and recanalization of blood vessels. Generally, there are three treatment methods. First, thrombectomy can immediately relieve blood vessel obstruction and prevent acute intestinal necrosis or related complications. However, new portal vein injuries and other surgical trauma often lead to the recurrence of PVT. In particular, patients cannot withstand the traumatic stimulation of reoperation. Therefore, this method is only suitable for patients in whom there are signs of peritonitis or the thrombus has been confirmed to come from the portal venous system. Second, interventional therapy can accurately deliver thrombolytic drugs to the obstruction with less damage and fewer complications. In addition, it provides an option for patients in whom liver function is decompensated, the PVT lasts for a long time, and conservative treatment was not effective. Although nonsurgical treatment is minimally invasive, effective, and reproducible, its risks still require our attention. For example, percutaneous portal vein thrombolysis can induce bleeding in the puncture tract. During the process of thrombolysis, it is necessary to monitor coagulation function and blood cell count over time. Therefore, it is contraindicated in patients with Child–Pugh class C who have large amounts of ascites and poor coagulation. Finally, anticoagulation and thrombolysis are the basic principles of noninvasive treatment[26]. Patients with primary blood hypercoagulability and early thrombosis will benefit more from anticoagulation therapy. Eighty percent of acute PVT cases can be completely or partially recanalized after anticoagulation therapy[27]. Compared with heparin, LMWH is the best anticoagulant. Because there is no obvious difference between the two anticoagulant drugs in terms of causing bleeding, LMWH can better improve the survival rate[25,28]. Studies have shown that LMWH is safe and effective in the treatment of PVT caused by liver cirrhosis[29], and changes in thrombus volume can be seen on imaging after 2 wk of anticoagulation therapy[28]. This is also consistent with the therapeutic effect of this patient after hepatectomy. If anticoagulation is not continued after recanalization, approximately 38%[30] of patients will develop PVT again. Some experts suggest that after 20 d of intravenous infusion of anticoagulant, it is best for patients to continue oral anticoagulant for 3 to 6 mo instead of subcutaneous LMWH[19,21]. Because long-term subcutaneous injection of LMWH after discharge can lead to decreased patient compliance, and standard treatment represented by VKAs and LMWH requires continuous monitoring of renal function and INR to adjust the dosage[31]. However, related foundational trials included no patients with PVT[32-35]. DOACs for the treatment of PVT are still not widely accepted, and further research is needed[36].
In addition to the treatment of PVT and prevention of recurrence mentioned above, prevention during the perioperative period is crucial. First, adequate portal blood flow should be ensured. Ultrasound can be used to measure portal vein blood flow, and less than 15 cm/s is an important risk factor[37]. Second, damage to the vascular intima should be avoided, for example, preventing violent pulling of the portal vein system during surgery, and reducing the time and frequency of portal occlusion. Finally, if symptoms such as nausea and vomiting occur after surgery, it is necessary to promptly confirm whether PVT occurred[21].
PVT is common in patients with liver cirrhosis or after liver transplantation and splenectomy. Surgeons should improve their understanding of this complication and use color Doppler ultrasound and CECT to confirm the appearance of PVT in a timely manner.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Singh N, United States; Tadros M, United States A-Editor: Lin FY, China S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Ageno W, Beyer-Westendorf J, Garcia DA, Lazo-Langner A, McBane RD, Paciaroni M. Guidance for the management of venous thrombosis in unusual sites. J Thromb Thrombolysis. 2016;41:129-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 84] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ, Nelson ME, Wells PS, Gould MK, Dentali F, Crowther M, Kahn SR. Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e419S-e496S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2565] [Cited by in RCA: 2562] [Article Influence: 197.1] [Reference Citation Analysis (0)] |
| 3. | Naymagon L, Tremblay D, Zubizarreta N, Moshier E, Troy K, Schiano T, Mascarenhas J. The efficacy and safety of direct oral anticoagulants in noncirrhotic portal vein thrombosis. Blood Adv. 2020;4:655-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 4. | De Gottardi A, Trebicka J, Klinger C, Plessier A, Seijo S, Terziroli B, Magenta L, Semela D, Buscarini E, Langlet P, Görtzen J, Puente A, Müllhaupt B, Navascuès C, Nery F, Deltenre P, Turon F, Engelmann C, Arya R, Caca K, Peck-Radosavljevic M, Leebeek FWG, Valla D, Garcia-Pagan JC; VALDIG Investigators. Antithrombotic treatment with direct-acting oral anticoagulants in patients with splanchnic vein thrombosis and cirrhosis. Liver Int. 2017;37:694-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 172] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 5. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 5998] [Article Influence: 856.9] [Reference Citation Analysis (3)] |
| 6. | Cheng S, Chen M, Cai J, Sun J, Guo R, Bi X, Lau WY, Wu M. Chinese Expert Consensus on Multidisciplinary Diagnosis and Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombus (2018 Edition). Liver Cancer. 2020;9:28-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 7. | Yoshiya S, Shirabe K, Nakagawara H, Soejima Y, Yoshizumi T, Ikegami T, Yamashita Y, Harimoto N, Nishie A, Yamanaka T, Maehara Y. Portal vein thrombosis after hepatectomy. World J Surg. 2014;38:1491-1497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 8. | Kuboki S, Shimizu H, Ohtsuka M, Kato A, Yoshitomi H, Furukawa K, Takayashiki T, Takano S, Okamura D, Suzuki D, Sakai N, Kagawa S, Miyazaki M. Incidence, risk factors, and management options for portal vein thrombosis after hepatectomy: a 14-year, single-center experience. Am J Surg. 2015;210:878-85.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Minagawa M, Makuuchi M. Treatment of hepatocellular carcinoma accompanied by portal vein tumor thrombus. World J Gastroenterol. 2006;12:7561-7567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 209] [Cited by in RCA: 229] [Article Influence: 12.1] [Reference Citation Analysis (1)] |
| 10. | Llovet JM, Bustamante J, Castells A, Vilana R, Ayuso Mdel C, Sala M, Brú C, Rodés J, Bruix J. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology. 1999;29:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 839] [Cited by in RCA: 904] [Article Influence: 34.8] [Reference Citation Analysis (1)] |
| 11. | Cheung TK, Lai CL, Wong BC, Fung J, Yuen MF. Clinical features, biochemical parameters, and virological profiles of patients with hepatocellular carcinoma in Hong Kong. Aliment Pharmacol Ther. 2006;24:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 74] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Ponziani FR, Zocco MA, Campanale C, Rinninella E, Tortora A, Di Maurizio L, Bombardieri G, De Cristofaro R, De Gaetano AM, Landolfi R, Gasbarrini A. Portal vein thrombosis: insight into physiopathology, diagnosis, and treatment. World J Gastroenterol. 2010;16:143-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 227] [Cited by in RCA: 194] [Article Influence: 12.9] [Reference Citation Analysis (2)] |
| 13. | Parikh S, Shah R, Kapoor P. Portal vein thrombosis. Am J Med. 2010;123:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 133] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 14. | Intagliata NM, Caldwell SH, Tripodi A. Diagnosis, Development, and Treatment of Portal Vein Thrombosis in Patients With and Without Cirrhosis. Gastroenterology. 2019;156:1582-1599.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 244] [Article Influence: 40.7] [Reference Citation Analysis (0)] |
| 15. | Tsochatzis EA, Senzolo M, Germani G, Gatt A, Burroughs AK. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther. 2010;31:366-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 223] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Nery F, Chevret S, Condat B, de Raucourt E, Boudaoud L, Rautou PE, Plessier A, Roulot D, Chaffaut C, Bourcier V, Trinchet JC, Valla DC; Groupe d'Etude et de Traitement du Carcinome Hépatocellulaire. Causes and consequences of portal vein thrombosis in 1,243 patients with cirrhosis: results of a longitudinal study. Hepatology. 2015;61:660-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 348] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 17. | Grando-Lemaire V, Guettier C, Chevret S, Beaugrand M, Trinchet JC. Hepatocellular carcinoma without cirrhosis in the West: epidemiological factors and histopathology of the non-tumorous liver. Groupe d'Etude et de Traitement du Carcinome Hépatocellulaire. J Hepatol. 1999;31:508-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Sainz-Barriga M, Baccarani U, Risaliti A, Gasparini D, Sponza M, Adani GL, Toniutto PL, Avellini C, Ramacciato G, Bresadola F. Successful minimally invasive management of late portal vein thrombosis after splenectomy due to splenic artery steal syndrome following liver transplantation: a case report. Transplant Proc. 2004;36:558-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Chaffanjon PC, Brichon PY, Ranchoup Y, Gressin R, Sotto JJ. Portal vein thrombosis following splenectomy for hematologic disease: prospective study with Doppler color flow imaging. World J Surg. 1998;22:1082-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 105] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Péré G, Basselerie H, Maulat C, Pitocco A, Leblanc P, Philis A, Julio CH, Tuyeras G, Buscail E, Carrere N. Splenic volume and splenic vein diameter are independent pre-operative risk factors of portal vein thrombosis after splenectomy: a retrospective cohort study. BMC Surg. 2021;21:366. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Skarsgard E, Doski J, Jaksic T, Wesson D, Shandling B, Ein S, Babyn P, Heiss K, Hu X. Thrombosis of the portal venous system after splenectomy for pediatric hematologic disease. J Pediatr Surg. 1993;28:1109-1112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 59] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Ikeda M, Sekimoto M, Takiguchi S, Kubota M, Ikenaga M, Yamamoto H, Fujiwara Y, Ohue M, Yasuda T, Imamura H, Tatsuta M, Yano M, Furukawa H, Monden M. High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg. 2005;241:208-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 186] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 23. | Klopfenstein CE, Morel DR, Clergue F, Pastor CM. Effects of abdominal CO2 insufflation and changes of position on hepatic blood flow in anesthetized pigs. Am J Physiol. 1998;275:H900-H905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Ruiz-Tovar J, Priego P. Portal Vein Thrombosis After Splenic and Pancreatic Surgery. Adv Exp Med Biol. 2017;906:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Hanafy AS, Abd-Elsalam S, Dawoud MM. Randomized controlled trial of rivaroxaban versus warfarin in the management of acute non-neoplastic portal vein thrombosis. Vascul Pharmacol. 2019;113:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 123] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 26. | Sogaard KK, Astrup LB, Vilstrup H, Gronbaek H. Portal vein thrombosis; risk factors, clinical presentation and treatment. BMC Gastroenterol. 2007;7:34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 145] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 27. | Valla DC, Condat B. Portal vein thrombosis in adults: pathophysiology, pathogenesis and management. J Hepatol. 2000;32:865-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 233] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 28. | Nagaoki Y, Aikata H, Daijyo K, Teraoka Y, Shinohara F, Nakamura Y, Hatooka M, Morio K, Nakahara T, Kawaoka T, Tsuge M, Hiramatsu A, Imamura M, Kawakami Y, Ochi H, Chayama K. Efficacy and safety of edoxaban for treatment of portal vein thrombosis following danaparoid sodium in patients with liver cirrhosis. Hepatol Res. 2018;48:51-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 113] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 29. | Loffredo L, Pastori D, Farcomeni A, Violi F. Effects of Anticoagulants in Patients With Cirrhosis and Portal Vein Thrombosis: A Systematic Review and Meta-analysis. Gastroenterology. 2017;153:480-487.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 296] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 30. | Delgado MG, Seijo S, Yepes I, Achécar L, Catalina MV, García-Criado A, Abraldes JG, de la Peña J, Bañares R, Albillos A, Bosch J, García-Pagán JC. Efficacy and safety of anticoagulation on patients with cirrhosis and portal vein thrombosis. Clin Gastroenterol Hepatol. 2012;10:776-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 289] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 31. | Rugivarodom M, Charatcharoenwitthaya P. Nontumoral Portal Vein Thrombosis: A Challenging Consequence of Liver Cirrhosis. J Clin Transl Hepatol. 2020;8:432-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 32. | EINSTEIN–PE Investigators, Büller HR, Prins MH, Lensin AW, Decousus H, Jacobson BF, Minar E, Chlumsky J, Verhamme P, Wells P, Agnelli G, Cohen A, Berkowitz SD, Bounameaux H, Davidson BL, Misselwitz F, Gallus AS, Raskob GE, Schellong S, Segers A. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med. 2012;366:1287-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1646] [Cited by in RCA: 1686] [Article Influence: 129.7] [Reference Citation Analysis (0)] |
| 33. | EINSTEIN Investigators, Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H, Gallus AS, Lensing AW, Misselwitz F, Prins MH, Raskob GE, Segers A, Verhamme P, Wells P, Agnelli G, Bounameaux H, Cohen A, Davidson BL, Piovella F, Schellong S. Oral rivaroxaban for symptomatic venous thromboembolism. N Engl J Med. 2010;363:2499-2510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2218] [Cited by in RCA: 2259] [Article Influence: 150.6] [Reference Citation Analysis (0)] |
| 34. | Agnelli G, Buller HR, Cohen A, Curto M, Gallus AS, Johnson M, Masiukiewicz U, Pak R, Thompson J, Raskob GE, Weitz JI; AMPLIFY Investigators. Oral apixaban for the treatment of acute venous thromboembolism. N Engl J Med. 2013;369:799-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1533] [Cited by in RCA: 1634] [Article Influence: 136.2] [Reference Citation Analysis (0)] |
| 35. | Schulman S, Kearon C, Kakkar AK, Mismetti P, Schellong S, Eriksson H, Baanstra D, Schnee J, Goldhaber SZ; RE-COVER Study Group. Dabigatran versus warfarin in the treatment of acute venous thromboembolism. N Engl J Med. 2009;361:2342-2352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1838] [Cited by in RCA: 1801] [Article Influence: 112.6] [Reference Citation Analysis (0)] |
| 36. | Priyanka P, Kupec JT, Krafft M, Shah NA, Reynolds GJ. Newer Oral Anticoagulants in the Treatment of Acute Portal Vein Thrombosis in Patients with and without Cirrhosis. Int J Hepatol. 2018;2018:8432781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 37. | Zocco MA, Di Stasio E, De Cristofaro R, Novi M, Ainora ME, Ponziani F, Riccardi L, Lancellotti S, Santoliquido A, Flore R, Pompili M, Rapaccini GL, Tondi P, Gasbarrini GB, Landolfi R, Gasbarrini A. Thrombotic risk factors in patients with liver cirrhosis: correlation with MELD scoring system and portal vein thrombosis development. J Hepatol. 2009;51:682-689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 364] [Cited by in RCA: 355] [Article Influence: 22.2] [Reference Citation Analysis (0)] |