Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7090
Peer-review started: December 17, 2021
First decision: February 21, 2022
Revised: March 3, 2022
Accepted: May 22, 2022
Article in press: May 22, 2022
Published online: July 16, 2022
Processing time: 199 Days and 20.2 Hours
Left bundle branch pacing (LBBP) is a physiological pacing method that has emerged in recent years. It is an ideal choice for patients with complete left bundle branch block who are in need of cardiac resynchronization therapy (CRT). Moreover, LBBP is superior in maintaining physiological ventricular activation and can effectively improve heart function and quality of life in patients with pacemaker-induced cardiomyopathy. However, LBBP in pacing-dependent patients who already have cardiac dysfunction has not been well assessed.
A 69-year-old male patient presented with symptoms of chest tightness, palpitation and systolic heart failure with New York Heart Association class III for 1 mo. The 12-lead electrocardiogram showed atrial fibrillation with third-degree atrioventricular block and ventricular premature beat. Holter revealed a right bundle branch block, atrial fibrillation with third-degree atrioventricular block, frequent multifocal ventricular premature beats, Ron-T and ventricular tachycardia. The echocardiogram documented an enlarged left atrium and left ventricle and a low left ventricular ejection fraction. Coronary angiography indicated a stenosis of 30% in the middle left anterior descending artery. Apparently, a CRT-D pacemaker was the best choice for this patient according to previous findings. However, the patient was worried about the financial burden. A single-chamber pacemaker with LBBP was selected, with the plan to take amiodarone and upgrade with dual-chamber implantable cardioverter-de
LBBP might be used in patients with heart failure and a high-degree atrioventricular block as an alternative to conventional CRT.
Core Tip: Left bundle branch pacing is a new and prospective pacing technique that is a promising alternative with the potential for similar outcomes in patients with complete left bundle branch block who need cardiac resynchronization therapy or for patients with pacemaker-induced cardiomyopathy. We present herein a patient with heart failure and high-degree atrioventricular block treated with left bundle branch pacing who received improved cardiac function during follow-up. This case highlights the possibility of left bundle branch pacing used in patients who already have heart failure and high-degree atrioventricular block as an alternative to conventional cardiac resynchronization therapy.
- Citation: Song BX, Wang XX, An Y, Zhang YY. Left bundle branch pacing in a ventricular pacing dependent patient with heart failure: A case report. World J Clin Cases 2022; 10(20): 7090-7096
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7090.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7090
Left bundle branch pacing (LBBP) is a new, prospective pacing technique that is more physiological than traditional right ventricular pacing (RVP)[1]. It is appropriate for pacing-dependent patients to prevent left ventricular mechanical asynchrony and to reduce the morbidity of heart dysfunction. A previous clinical study has already shown that LBBP is superior for maintaining physiological ventricular activation[2] and can effectively improve heart function and quality of life in patients with pacemaker-induced cardiomyopathy[3-5]. However, LBBP in pacing-dependent patients who already have cardiac dysfunction has not been well evaluated. Here, we report a case of a heart failure patient with atrial fibrillation and third-degree atrioventricular block who successfully received LBBP.
A 69-year-old male patient presented with symptoms of chest tightness, palpitation and exertional dyspnea.
The patient’s symptoms started 1 mo prior with recurrent episodes of chest tightness, palpitation and exertional dyspnea. Dyspnea worsened the previous 3 d.
The patient had a history of atrial fibrillation and diabetes.
The patient had no family history.
The rhythm of heart auscultation was irregular.
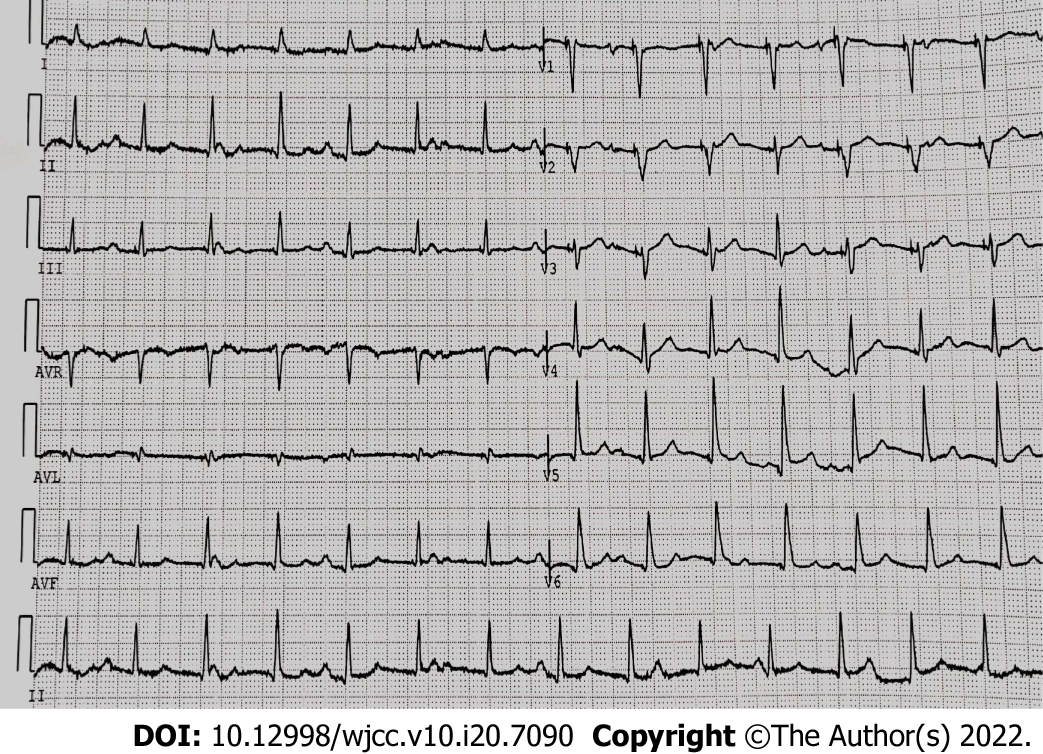
The 12-lead electrocardiogram showed atrial fibrillation with third-degree atrioventricular block and ventricular premature beat (Figure 1A). Holter revealed a right bundle branch block, atrial fibrillation with third-degree atrioventricular block, frequent multifocal ventricular premature beats (Figure 1B), Ron-T and ventricular tachycardia. The echocardiogram documented a large left atrium diameter (48 mm), large left ventricular end-diastolic diameter (62 mm), large left ventricular end-systolic diameter (54 mm), low left ventricular ejection fraction (38%), severe mitral regurgitation and moderate pulmonary hypertension (Table 1) The brain natriuretic peptide level was 451 pg/mL.
| LVEDD in mm | LVESD in mm | LVEF, % | MR | TR | PAP in mmHg | NYHA | |
| Before procedure | 62 | 54 | 38 | Severe | Mild-moderate | 57 | III |
| Follow-up | 56 | 45 | 41 | Moderate | Mild-moderate | 46 | I |
Coronary angiography indicated a stenosis of 30% in the middle left anterior descending artery.
Arrhythmia, atrial fibrillation with third-degree atrioventricular block, frequent multifocal ventricular premature beats, Ron-T, ventricular tachycardia, right bundle branch block, cardiomyopathy, coronary atherosclerosis, cardiac insufficiency (New York Heart Association class III) and diabetes.
An optimal medical therapy with rivaroxaban, diuretic, sacubitril valsartan and dapagliflozin was chosen. Meanwhile, permanent pacemaker implantation was decided after optimal medical therapy for heart failure, and the patient signed informed consent.
Considering the low heart function and high risk of sudden cardiac death, a cardiac resynchronization therapy (CRT)-D pacemaker was the best choice for this patient according to previous findings[6]. However, due to the local insurance policy, the reimbursement ratio of pacemaker implantation is very low, and the cost of a CRT pacemaker is much more expensive than that of a single-chamber pacemaker. The patient was worried about the financial burden. A single-chamber pacemaker with LBBP was selected, with the plan to take amiodarone and upgrade to dual-chamber implantable cardioverter-defibrillator (ICD) or CRT-D at an appropriate time. We will still use the left bundle branch electrode as the RVP electrode and place the defibrillation electrode on the right ventricular apex with only the defibrillation function applied as the dual-chamber ICD. Similarly, we will use the LBB electrode combined with the right ventricular defibrillation electrode and the traditional left ventricular electrode as CRT-D, which comprises the left bundle branch optimized CRT-D that we are currently performing frequently.
The patient underwent implantation of a single-chamber pacemaker (RESR 1, Medtronic Inc., Minneapolis, MN, United States). A ventricular pacing lead (3830-69 cm, Medtronic Inc.) was implanted into the left bundle branch area using the transventricular septal method. In brief, the delivery sheath (C315HIS, Medtronic Inc.) and the 3830 lead were inserted through the left axillary vein and moved to the ventricular side inferior to the septal leaflet of tricuspid valves under right anterior oblique fluoroscopy. The pacing lead was then screwed toward the left side of the interventricular septum. The pacing lead was successfully placed in the left bundle branch area (Figure 2). The pacing threshold was 0.7 V at 0.4 ms, and the electrocardiography mode had a right bundle branch conduction delay (Figure 3). The R wave amplitude was 12 mV.
During the follow-up at 3 mo after LBBP, the patient showed an improvement in cardiac function: left ventricular end-diastolic diameter decreased from 62 mm to 56 mm, left ventricular end-systolic diameter decreased from 54 mm to 45 mm, left ventricular ejection fraction increased from 38% to 41%, pulmonary artery pressure decreased from moderate to mild, and New York Heart Association functional class was maintained at I. The brain natriuretic peptide level was downregulated to 81 pg/mL. Moreover, the patient was free from chest tightness and palpitations. Holter showed decreased ventricular arrhythmia of less than 5%.
As a conventional pacing strategy, RVP is easy to access, well tolerated and stable. However, studies have indicated that chronic RVP may result in intraventricular and interventricular desynchrony, which is harmful to left ventricular function and is associated with heart failure and increased mortality[7]. Recognizing the deleterious effect of RVP, Deshmukh et al[8] first described the pioneering research of permanent His bundle pacing (HBP) in 2000. Since then, multiple studies have demonstrated the safety and feasibility of HBP. Compared with RVP, HBP is associated with a reduction in the combined endpoint of death and heart failure hospitalization[9]. Although HBP could be a physiological alternative to RVP, due to technical challenges and unstable and higher pacing thresholds, especially in patients with pathological disease in the conduction system, HBP has not become mainstream. Moreover, HBP has a lower R wave amplitude and a higher lead dislocation rate.
Huang et al[10] described a case of a patient with dilated cardiomyopathy and complete left bundle branch block (LBBB) who was treated with LBBP in 2017 and found improved cardiac function. The safety and feasibility of LBBP have been subsequently tested by multiple studies. Since then, LBBP has become a new pacing site because of its low threshold and narrow paced QRS duration[11]. During LBBP, the lead is fixed in the left bundle branch area, and the left ventricular His-Purkinje system is paced directly, which leads to a shorter paced QRS duration and better electrical synchrony compared to RVP.
Recently, several studies have shown that left ventricular synchronization in the LBBP group is superior to that of right ventricular apical pacing, right ventricular outflow tract pacing and right ventricular septal pacing[12-14]. Compared with RVP, LBBP is associated with a reduced incidence of pacing-induced left ventricular dysfunction and hospitalization for heart failure[1,12-14]. In 2020, Wu et al[15] revealed that LBBP produced significantly greater reductions in QRS duration and resulted in significant improvements in the function of the left ventricle and clinical response compared to biventricular pacing in heart failure patients with typical LBBB.
Subsequently, a number of studies have shown that in heart failure with LBBB, LBBP-related complications and adverse clinical outcomes, including heart failure hospitalization and mortality, were not significantly different compared to CRT[16]. Therefore, LBBP could be a superior alternative to CRT in patients with typical LBBB. In the 2021 European Society of Cardiology Guidelines on cardiac pacing and cardiac resynchronization therapy, CRT-P is highly recommended for patients with heart failure and high-degree atrioventricular block to reduce morbidity, including patients with atrial fibrillation[6]. However, whether LBBP is an ideal choice for heart failure patients with high-degree atrioventricular block lacks evidence. Moreover, in patients who are candidates for an ICD and who have CRT indications, implantation of CRT-D is highly recommended[6].
As a traditional pacemaker implantation method, right ventricular apical pacing has been widely used to date, but this method can lead to electrical and mechanical asynchrony, which increase the risk of atrial fibrillation, heart failure and even death[17]. Subsequently, right ventricular outflow tract and right ventricular septal pacing have been developed to reduce these potential adverse consequences, but their long-term results have not proved to be better than right ventricular apical pacing. Cardiac resynchronization therapy through biventricular pacing is another pacing method for the treatment of heart failure.
Clinical studies have shown that CRT can promote left ventricular reverse remodeling and exercise tolerance and reduce the incidence rate and mortality of heart failure patients[6]. Although the benefits of CRT have been fully demonstrated, the nonresponse rate of this therapy is very high (30%-40%). In addition, biventricular pacing is a nonphysiological method that requires two leads to activate the ventricular myocardium rather than a specialized conduction system. Therefore, the physiological pacing technology of directly activating the conduction system has become the focus of attention.
LBBP is achieved through the transventricular septal approach, which can directly excite the left bundle branch area, and the QRS duration is narrowed due to the rapid activation of the left ventricle. At present, this method has been extended to treat some patients with heart failure and ventricular dyssynchrony caused by LBBB. According to the current research, with the increase in clinical application, the clinical development of LBBP is in an early but encouraging stage. However, there is a need to develop standardized procedures with improved delivery tools and pacing leads as well as long-term efficacy and safety studies[18].
In our case, the patient had an indication for CRT-D implantation. However, due to economic factors, LBBP was the best choice. It remains unclear whether LBBP was the best choice to avoid further deterioration of cardiac function or whether the patient should receive an ICD to prevent sudden cardiac death. Recent studies have shown that upgrading to LBBP can effectively improve heart function and quality of life in patients with pacing-induced cardiomyopathy[3-5]. However, LBBP in patients with cardiac dysfunction and high-degree AVB lacks evidence. In our case, there was an increased left ventricular ejection fraction and decreased left ventricular end-diastolic diameter and left ventricular end-systolic diameter 3 mo after LBBP implantation. In addition, with drug therapy and cardiac function recovery, ventricular arrhythmia was significantly decreased. Therefore, future work should focus on exploring the advantage of LBBP in patients with heart failure and high-degree atrioventricular block, as it may obtain more benefit than CRT with less cost.
We present the case of a heart failure patient with atrial fibrillation and third-degree atrioventricular block who successfully received LBBP. After LBBP for 3 mo, there was an improvement in left ventricle function and a reduction in left ventricular size. This case shows the possibility of using LBBP in patients with heart failure and high-degree atrioventricular block as an alternative to conventional CRT.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lakusic N, Croatia; Patel L, United States; Pradhan A, India A-Editor: Yao QG, China S-Editor: Chang KL L-Editor: Filipodia P-Editor: Chang KL
| 1. | Chen X, Jin Q, Bai J, Wang W, Qin S, Wang J, Liang Y, Su Y, Ge J. The feasibility and safety of left bundle branch pacing vs. right ventricular pacing after mid-long-term follow-up: a single-centre experience. Europace. 2020;22:ii36-ii44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 2. | Abdin A, Aktaa S, Vukadinović D, Arbelo E, Burri H, Glikson M, Meyer C, Munyombwe T, Nielsen JC, Ukena C, Vernooy K, Gale CP. Outcomes of conduction system pacing compared to right ventricular pacing as a primary strategy for treating bradyarrhythmia: systematic review and meta-analysis. Clin Res Cardiol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Li H, Wang L, Peng X, Wu J. The quality of life of patients with pacemaker-induced cardiomyopathy after they upgrade to left bundle branch pacing. Am J Transl Res. 2021;13:3044-3053. [PubMed] |
| 4. | Yang YH, Wang KX, Ma PP, Zhang RF, Waleed KB, Yin X, Gao LJ, Xia YL, Dong YX. His-purkinje system pacing upgrade improve the heart performances in patients suffering from pacing-induced cardiomyopathy with or without permanent atrial fibrillation. Int J Cardiol. 2021;335:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Ye Y, Wu S, Su L, Sheng X, Zhang J, Wang B, Sharma PS, Ellenbogen KA, Su Y, Chen X, Fu G, Huang W. Feasibility and Outcomes of Upgrading to Left Bundle Branch Pacing in Patients With Pacing-Induced Cardiomyopathy and Infranodal Atrioventricular Block. Front Cardiovasc Med. 2021;8:674452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Glikson M, Nielsen JC, Kronborg MB, Michowitz Y, Auricchio A, Barbash IM, Barrabés JA, Boriani G, Braunschweig F, Brignole M, Burri H, Coats AJS, Deharo JC, Delgado V, Diller GP, Israel CW, Keren A, Knops RE, Kotecha D, Leclercq C, Merkely B, Starck C, Thylén I, Tolosana JM; ESC Scientific Document Group. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur Heart J. 2021;42:3427-3520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 287] [Cited by in RCA: 1109] [Article Influence: 277.3] [Reference Citation Analysis (1)] |
| 7. | Tops LF, Schalij MJ, Bax JJ. The effects of right ventricular apical pacing on ventricular function and dyssynchrony implications for therapy. J Am Coll Cardiol. 2009;54:764-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 297] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 8. | Deshmukh P, Casavant DA, Romanyshyn M, Anderson K. Permanent, direct His-bundle pacing: a novel approach to cardiac pacing in patients with normal His-Purkinje activation. Circulation. 2000;101:869-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 491] [Cited by in RCA: 539] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 9. | Abdelrahman M, Subzposh FA, Beer D, Durr B, Naperkowski A, Sun H, Oren JW, Dandamudi G, Vijayaraman P. Clinical Outcomes of His Bundle Pacing Compared to Right Ventricular Pacing. J Am Coll Cardiol. 2018;71:2319-2330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 424] [Article Influence: 60.6] [Reference Citation Analysis (0)] |
| 10. | Huang W, Su L, Wu S, Xu L, Xiao F, Zhou X, Ellenbogen KA. A Novel Pacing Strategy With Low and Stable Output: Pacing the Left Bundle Branch Immediately Beyond the Conduction Block. Can J Cardiol. 2017;33:1736.e1-1736.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 523] [Article Influence: 65.4] [Reference Citation Analysis (0)] |
| 11. | Chen K, Li Y, Dai Y, Sun Q, Luo B, Li C, Zhang S. Comparison of electrocardiogram characteristics and pacing parameters between left bundle branch pacing and right ventricular pacing in patients receiving pacemaker therapy. Europace. 2019;21:673-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 12. | Zhang S, Guo J, Tao A, Zhang B, Bao Z, Zhang G. Clinical outcomes of left bundle branch pacing compared to right ventricular apical pacing in patients with atrioventricular block. Clin Cardiol. 2021;44:481-487. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Liu Q, Yang J, Bolun Z, Pei M, Ma B, Tong Q, Yin H, Zhang Y, You L, Xie R. Comparison of cardiac function between left bundle branch pacing and right ventricular outflow tract septal pacing in the short-term: A registered controlled clinical trial. Int J Cardiol. 2021;322:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Heckman LIB, Luermans JGLM, Curila K, Van Stipdonk AMW, Westra S, Smisek R, Prinzen FW, Vernooy K. Comparing Ventricular Synchrony in Left Bundle Branch and Left Ventricular Septal Pacing in Pacemaker Patients. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 15. | Wu S, Su L, Vijayaraman P, Zheng R, Cai M, Xu L, Shi R, Huang Z, Whinnett ZI, Huang W. Left Bundle Branch Pacing for Cardiac Resynchronization Therapy: Nonrandomized On-Treatment Comparison With His Bundle Pacing and Biventricular Pacing. Can J Cardiol. 2021;37:319-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 191] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 16. | Chen X, Ye Y, Wang Z, Jin Q, Qiu Z, Wang J, Qin S, Bai J, Wang W, Liang Y, Chen H, Sheng X, Gao F, Zhao X, Fu G, Ellenbogen KA, Su Y, Ge J. Cardiac resynchronization therapy via left bundle branch pacing vs. optimized biventricular pacing with adaptive algorithm in heart failure with left bundle branch block: a prospective, multi-centre, observational study. Europace. 2022;24:807-816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 95] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 17. | Lamas GA, Lee KL, Sweeney MO, Silverman R, Leon A, Yee R, Marinchak RA, Flaker G, Schron E, Orav EJ, Hellkamp AS, Greer S, McAnulty J, Ellenbogen K, Ehlert F, Freedman RA, Estes NA 3rd, Greenspon A, Goldman L; Mode Selection Trial in Sinus-Node Dysfunction. Ventricular pacing or dual-chamber pacing for sinus-node dysfunction. N Engl J Med. 2002;346:1854-1862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 692] [Cited by in RCA: 652] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 18. | Liu P, Wang Q, Sun H, Qin X, Zheng Q. Left Bundle Branch Pacing: Current Knowledge and Future Prospects. Front Cardiovasc Med. 2021;8:630399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |