Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7037
Peer-review started: November 22, 2021
First decision: December 10, 2021
Revised: December 24, 2021
Accepted: May 22, 2022
Article in press: May 22, 2021
Published online: July 16, 2022
Processing time: 224 Days and 22.7 Hours
Solitary plasmacytoma in the left rib is rare and can cause chest discomfort such as chest pain and tightness, and its clinical manifestations are not typical, so it is often misdiagnosed. We report a case of left costal plasmacytoma misdiagnosed as angina pectoris. We also review the literature and provide suggestions as to how to avoid misdiagnosis.
A 77-year-old man with a history of intermittent chest tightness for 3 years presented with pain in the left chest for 1 wk and was admitted to hospital. The cardiologists initially diagnosed angina pectoris but the findings of coronary angiography were not consistent with the symptoms. Computed tomography showed that the left eighth rib mass was accompanied by bone destruction. The patient was transferred to our department for further treatment. Preoperative biopsy indicated that the lesion was possibly malignant, and elective surgery was performed to remove the lesion. The size of the tumor was about 4 cm. The tumor was spindle-shaped and protruded into the pleural cavity, without invading the lungs. Postoperative pathology confirmed that the left rib lesion was plasma
Left rib solitary plasmacytoma is a rare disease confined to a specific rib and can cause local pain. Attention should be paid to the differential diagnosis of angina pectoris to avoid misdiagnosis.
Core Tip: In the diagnosis of rib solitary plasmacytoma (SP), attention should be paid to the following aspects: the patient has an unknown cause of rib fracture or there is a long-term chest pain; and the computed tomography of the rib shows that osteolysis of ribs coexists with soft tissue mass around the rib. Local surgical resection is the first choice for the treatment of rib SP. Postoperative radiotherapy should be performed to obtain a better curative effect, prolong patient survival and prevent tumor progression and recurrence. Attention should be paid to the differential diagnosis from angina pectoris to avoid misdiagnosis.
- Citation: Yao J, He X, Wang CY, Hao L, Tan LL, Shen CJ, Hou MX. Solitary plasmacytoma of the left rib misdiagnosed as angina pectoris: A case report . World J Clin Cases 2022; 10(20): 7037-7044
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7037.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7037
A 77-year-old man with a history of intermittent chest tightness for 3 years, presented with pain in the left chest for 1 wk, and was admitted to hospital.
The patient’s chest pain was dull and had not dissipated. The pain increased on rising and lying in bed. No awakening or sweating occurred at night. After oral administration of nitroglycerin tablets, chest tightness was significantly reduced, but chest pain was not obviously alleviated.
The patient had a history of angina pectoris for 3 years.
The patient was conscious, with normal temperature, blood pressure, heart rate and rhythm, and slightly increased respiration (22 breaths/min). Electrocardiography at admission showed a sinus heart rate with ST segment depression of 0.05 mV in leads V4–V6. There was no chest pain on palpation. The primary diagnosis by the cardiologist was recurrent angina pectoris.
Both the patient and his family denied that they had a family history of cancer.
The patient was conscious, with normal temperature, blood pressure, heart rate and rhythm, and slightly increased respiration (22 breaths/min). Electrocardiography at admission showed a sinus heart rate with ST segment depression of 0.05 mV in leads V4–V6. There was no chest pain on palpation. The primary diagnosis by the cardiologist was recurrent angina pectoris.
Routine blood tests, renal function, ion levels and myocardial enzymes were normal.
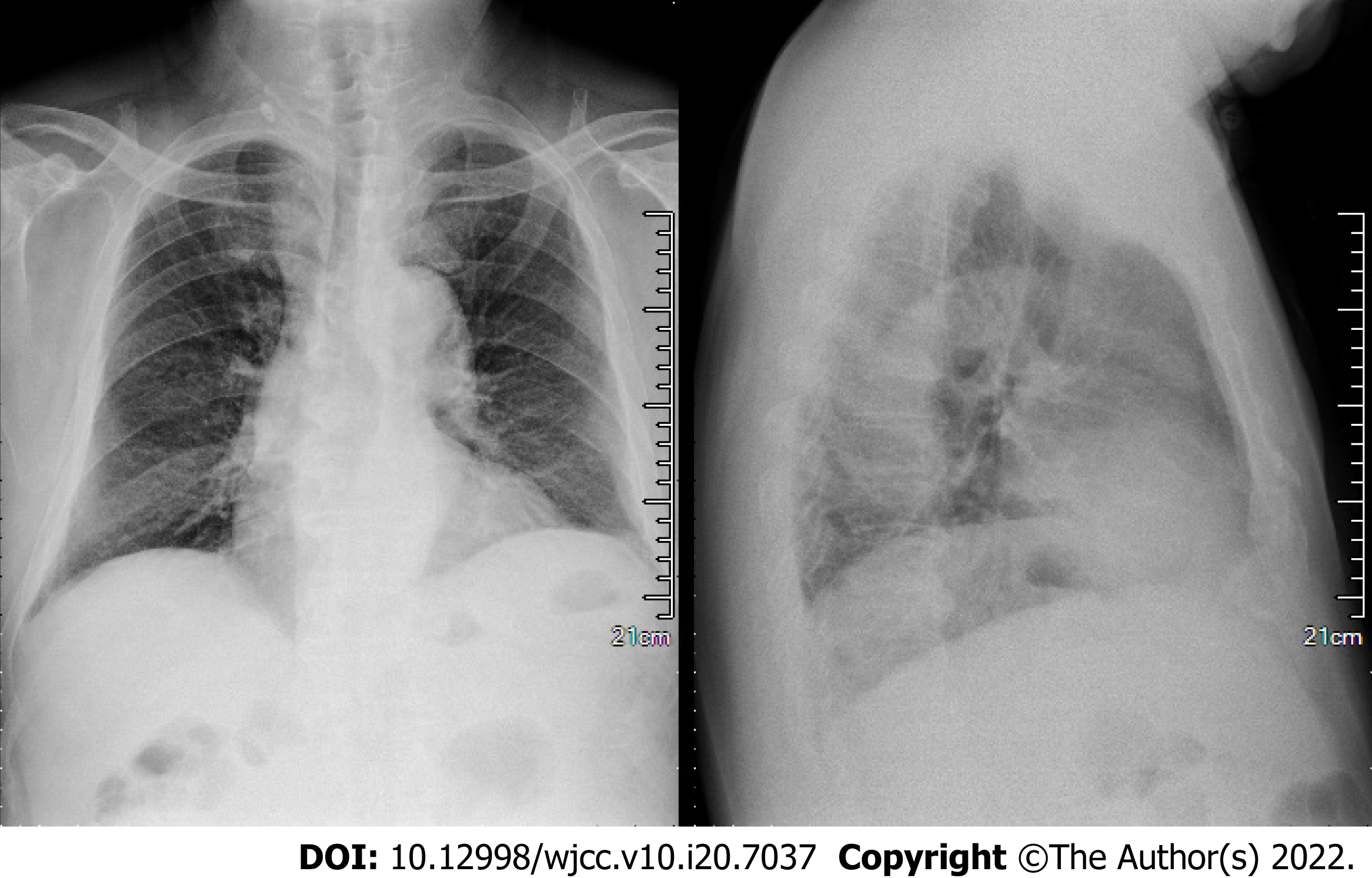
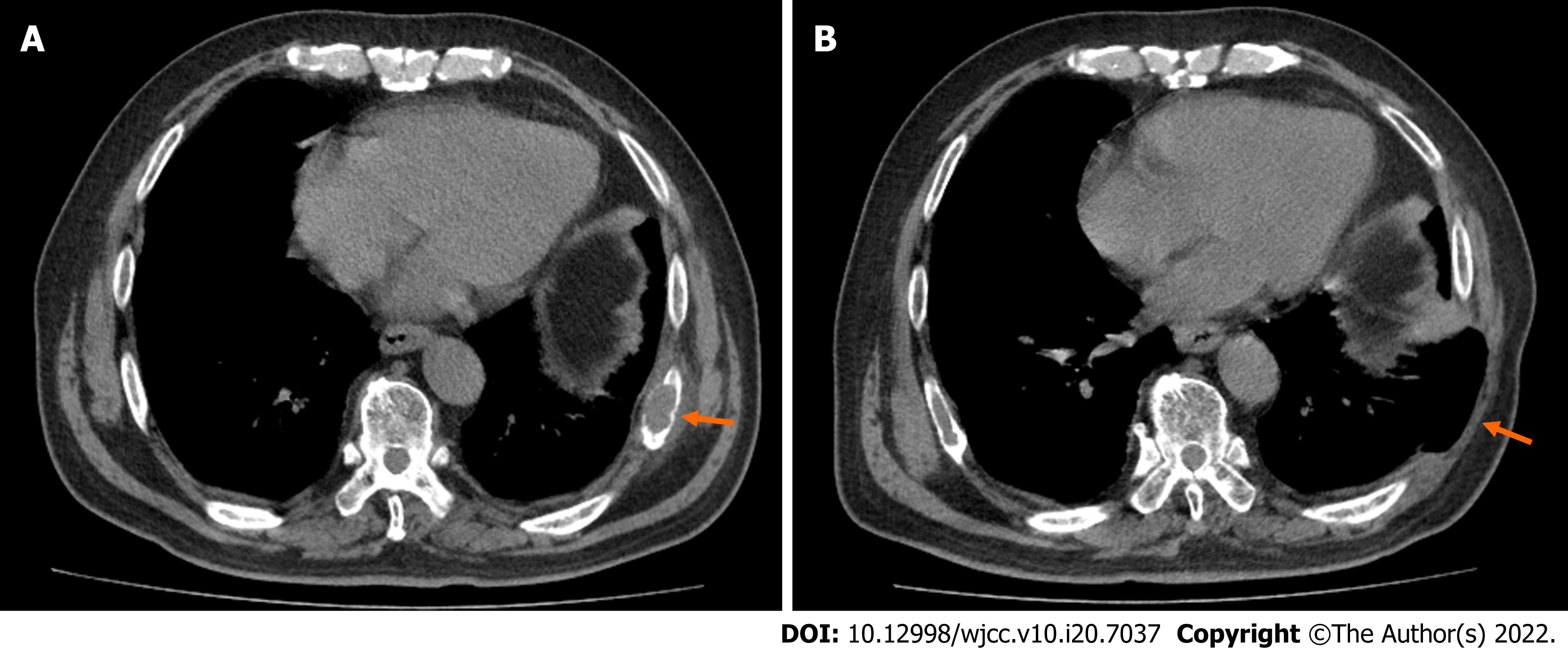
Chest X-ray showed no significant abnormalities (Figure 1). Coronary angiography performed by cardiologists showed that the intima of the coronary arteries was not smooth, and the proximal segment of the left anterior descending branch (LAD) was narrowed by 40%, the middle segment of the LAD by 50%, the middle segment of the right coronary artery (RCA) by 40%–50%, and the distal segment of the RCA by 30%–40%. Compared with 3 years ago, the degree of stenosis had not changed significantly. Chest computed tomography (CT) (Figure 2A) showed that left eighth rib mass was accompanied by bone destruction.
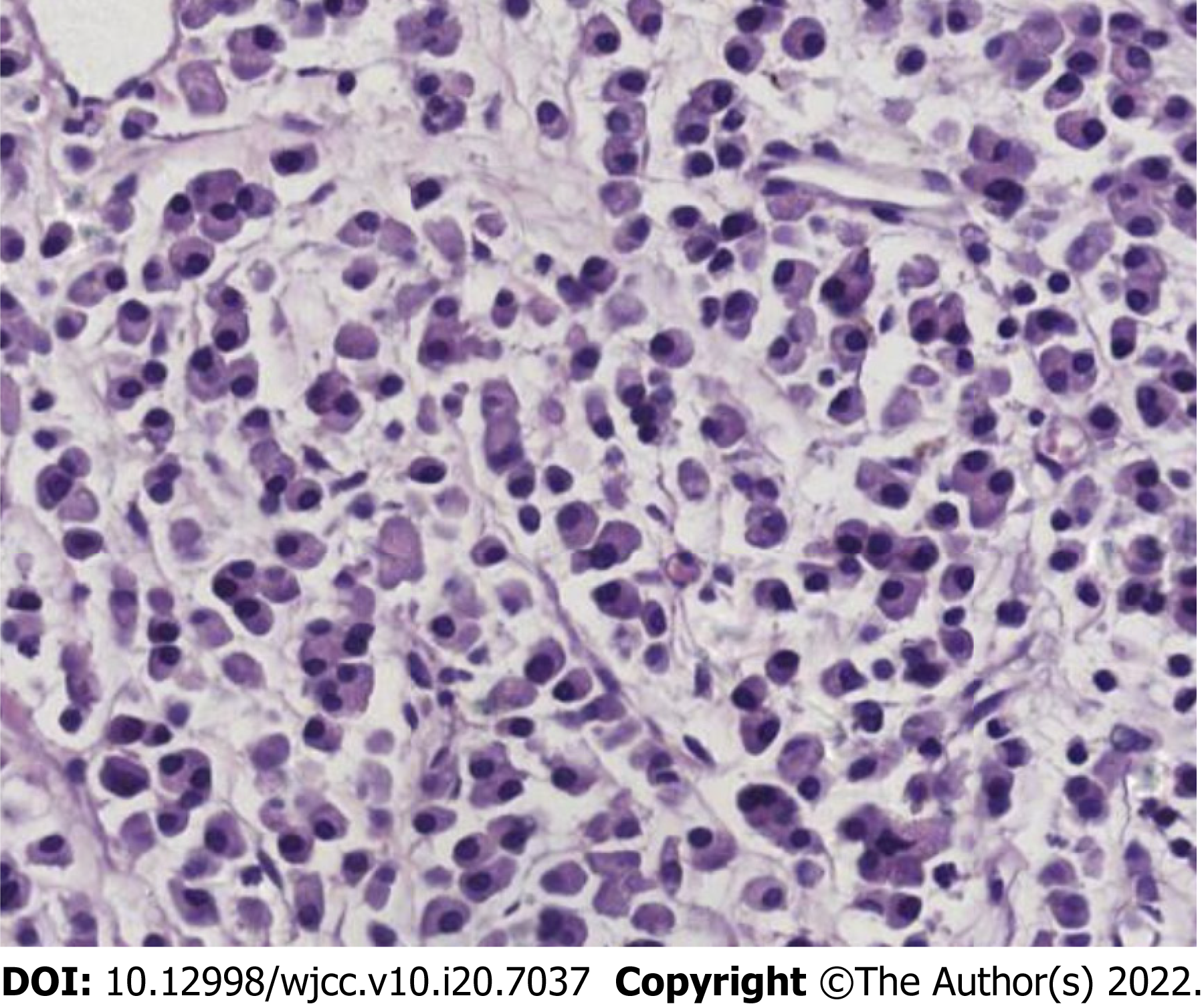
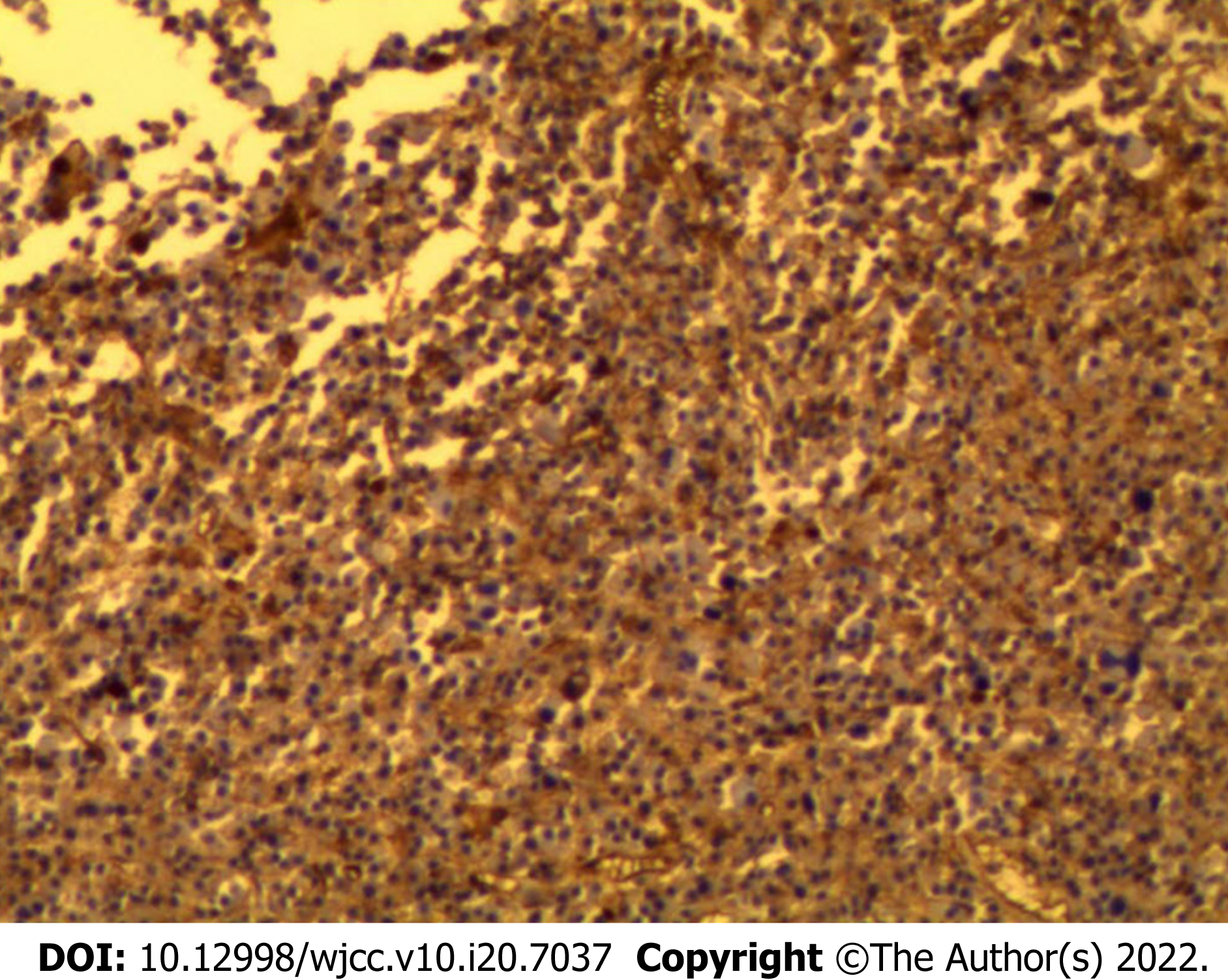
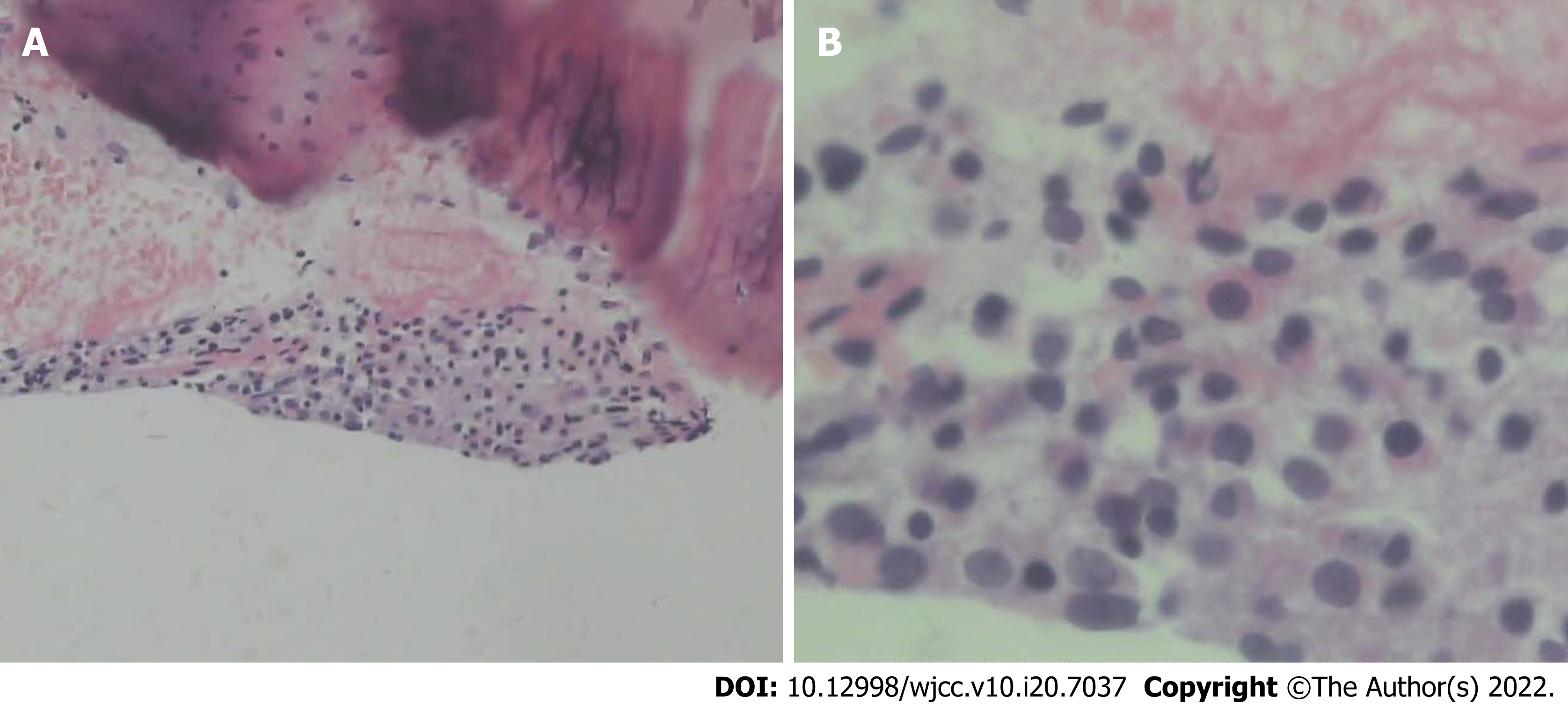
Postoperative pathology (Figures 3 and 4) showed that many immature plasma cells proliferated diffusely, with CD 138(+) and ki-67 (20%+). Therefore, the left rib tumor was finally diagnosed as a plasmacytoma.
After coronary angiography, the cardiology department invited the cardiothoracic surgery department for consultation, and the left rib lesion was found after careful reading of the CT. The patient was transferred to our department for further treatment. A puncture biopsy was performed on the rib masses. Postoperative pathology showed a high degree of suspicion of malignant tumor (Figure 5A and B). Whole body CT scan showed no other bone damage. Ribectomy was performed under general anesthesia. The rib lesions showed fusiform growth, protruding to the pleural cavity, and did not invade the lungs. The tumor was about 4 cm and 2 cm in size, and another small lump was about 1.5 cm and 0.8 cm away from the larger one, and the rib surface was damaged. At 5 cm from the medial and lateral ends of the mass, the ribs were cut off and the rib mass was completely removed (Figure 2B).
Chest pain was significantly relieved after the operation. Patients were unaware of the fact that they had a malignant tumor. The patient’s family unanimously disagreed with the patient’s radiotherapy and chemotherapy. Therefore, after discharge, the patient took thalidomide and dexamethasone tablets orally. Due to serious gastrointestinal reactions, the patient voluntarily gave up taking the above-mentioned drugs. Unfortunately, after 14 mo follow-up, the patient died of systemic metastasis.
Plasmacytoma is a malignant tumor mainly caused by abnormal proliferation of plasmacytoma clones. Clinically, multiple myxomas are common, and isolated plasmacytoma is rare. Solitary plasmacytoma (SP) is characterized by a single clonal plasma cell mass; no or only a small amount of bone marrow plasma cell degeneration; and no symptoms except those of the primary lesion. SP can present as extramedullary (extraosseous) plasmacytoma, that is, in soft tissues, or as solitary bone plasmacytoma (SBP)[1]. SP is a rare disease with a cumulative incidence of 0.15/100000[1,2]. SBP comprises 70% of all SP cases [1].
SP is difficult to diagnose preoperatively, with a high misdiagnosis rate and limited sites of occurrence. It can occur in any bone tissue but most commonly in the spine and skull, followed by ribs, clavicle and scapula, and rarely in the long tubular bones of the lower limbs, and generally without bone marrow abnormality. Rib SP is a rarer disease with no definite criteria for diagnosis and treatment. SP is confined to a specific rib, causing local pain, and its clinical manifestations are not characteristic, so it is often misdiagnosed[3].
We conducted a literature search on PubMed using the search terms “solitary plasmacytoma and rib” and identified 23 case reports published between 1992 and 2020[4-26] (Table 1). Among these rib SP patients, 14 were male and nine were female (with a male to female ratio of 1.6:1), aged between 26 and 75 years (mean 50.5 ± 15.6 years; median 46 years). The ratio of right rib to the left rib was 1.8: 1, and most tumors occurred in the fourth to sixth rib (65.2%). In our case, the lesion was located in the left eighth rib (the overlap areas of common angina pain, i.e., precordial area), and the patient also had a history of angina pectoris. Electrocardiography at the time of admission showed a sinus heart rate with ST segment depression of 0.05 mV in leads V4–V6. However, the results of coronary angiography did not explain the cause of the patient’s left chest pain. After coronary angiography, the cardiology department invited the cardiothoracic surgery department for consultation, and the left rib lesion was found after careful reading of the CT. Because the tumor location was covered by the heart and diaphragm, it could not be observed in the chest X-ray. Undoubtedly, it is highly likely to be misdiagnosed as angina pectoris for early stage of left-sided rib tumor. In addition, nitroglycerin has a relaxing effect on bronchial smooth muscle. This may be related to the relief of chest tightness. It is the relief of the patient’s symptoms after the application of nitroglycerin that misled the initial judgment of the cardiologist. The currently recommended diagnostic criteria[27] for SPB include: (1) Absence of bone marrow plasma cells; (2) Single lesion of bone or soft tissue; (3) Negative whole body imaging for additional lesions; and (4) Absence of end organ damage: Hypercalcemia, renal dysfunction, or anemia. In our case, the patient underwent a biopsy before removing the rib mass. Pathology revealed a malignant tumor of plasma cells. Other parts of the body were scanned with CT but no similar lesions were found in other bone tissues. Therefore, rib SP was considered before the operation. At present, the diagnosis of SP is based on biopsy, histology and immunohistochemistry to confirm homogeneous infiltration of monoclonal plasma cells, which usually express CD138 and/or CD38[1]. In our case, postoperative immunohistochemical pathology showed CD138 (+), which met the above pathological diagnosis criteria.
| Ref. | Gender | Age | Location of rib | Treatment | Prognosis | |
| 1 | Ikeda et al[4], 1992 | M | 75 | Left 4th | R | NM |
| 2 | Hihara et al[5], 1993 | F | 52 | Left 4th | NM | Relapse-free for 23 months’ follow-up |
| 3 | Hanawa et al[6], 1994 | M | 58 | Right 7th and 8th | S+R | Recurrence on the left side after 7 mo |
| 4 | Hirai et al[7], 1995 | F | 72 | Right 5th | S+R | Relapse-free for 23 mo’ follow-up |
| 5 | Mankodi et al[8], 1999 | F | 26 | Left 6th | S+R | NM |
| 6 | Kadokura et al[9], 2000 | M | 44 | Left 7th | S+R | Relapse-free for 24 mo’ follow-up |
| 7 | Sato et al[10], 2001 | M | 46 | Right 5th | S | NM |
| 8 | George et al[11], 2002 | M | 29 | Right 11th | S+R | NM |
| 9 | Yan et al[12], 2003 | F | 45 | 7th rib (left or right NM) | R | Relapse-free for 24 mo’ follow-up |
| 10 | García et al[23], 2004 | F | 32 | Right 9th | S | Relapse-free for 18 mo’ follow-up |
| 11 | Bousnina et al[13], 2006 | M | 52 | Left 6th | S+R | Relapse-free for 12 mo’ follow-up |
| 12 | Xiao et al[14], 2008 | F | 30 | Right 4th | S+R | Relapse-free for 11 mo’ follow-up |
| 13 | Ketata et al[15], 2009 | M | 60 | Left 1st | S+R | Relapse-free for 8 mo’ follow-up |
| 14 | Pattanayak et al[16], 2010 | M | 60 | Right 4th | S+R | Remission for 8 mo |
| 15 | Kodate et al[17], 2010 | M | 70 | Right 4th | S+R+C | Remission for 33 mo |
| 16 | Singal et al[18], 2011 | F | 43 | Right 5th | S+R | Relapse-free for 30 mo’ follow-up |
| 17 | Lee et al[19], 2012 | M | 73 | Right 5th | S+R | NM |
| 18 | Santos et al[20], 2012 | F | 65 | Right 6th | NM | NM |
| 19 | Tajima et al[21], 2014 | F | 71 | Right 3rd | S | Relapse-free for 18 mo’ follow-up |
| 20 | Razafimanjato et al[22], 2014 | M | 42 | Left 2nd | S+C | Relapse-free for 36 mo’ follow-up |
| 21 | Caffery et al[24], 2014 | M | 33 | Right 5th | R | NM |
| 22 | Jia et al[25], 2015 | M | 44 | Right 6th | S+R | Relapse-free for 6 mo’ follow-up |
| 23 | Singh et al[26], 2020 | M | 39 | Left 4th | NM | NM |
Plasmacytomas usually do not require surgical resection, because these malignancies are sensitive to radiation. In most cases, surgical resection is reserved in the case of loss of anatomical integrity or emergency decompression, necessitating resection due to compression of the spinal cord or nerve root. If surgery is performed, it is usually before radiotherapy, and it is used to assist deterministic radiotherapy[1,27]. According to our literature review, costal plasmacytoma was treated with surgical resection combined with radiotherapy, and the tumor recurrence-free or remission-free duration was 6–30 mo (average 16.1 ± 8.9, median 12 mo)[5,7,9,13-16,23,25]. For patients who received only surgical resection without postoperative radiotherapy, the tumor relapse-free duration was 18 mo[21,23]. For those who had undergone surgical resection combined with chemotherapy[22], or surgical resection combined with radiotherapy and chemotherapy[17], the tumor recurrence-free duration after surgery appeared to be longer, and could be > 33 mo. In our case, the patient underwent surgery combined with chemotherapy, but due to serious adverse drug reactions, the patient stopped drug chemotherapy, resulting in tumor recurrence and death 14 mo after surgery. Despite good local control, most patients with SP eventually develop multiple myeloma[27]. Sustained high levels of monoclonal protein after radiotherapy are now an important factor in prognosis. Serum monoclonal protein > 0.5 g/dL and abnormal serum-free light chain could be negative prognostic factors, according to the results of a retrospective study by Dingli et al[28]. In addition, it has been suggested that early diagnosis of SP may prevent SP from developing into multiple myeloma and enable patients to obtain prolonged tumor-free survival or cure by reducing tumor burden by surgery and postoperative adjuvant radiotherapy. Therefore, the timeliness of SP diagnosis is also a factor affecting prognosis.
Rib SP is a rare disease confined to a specific rib and can cause local pain. The majority of patients are male and the location of onset is mostly in the right rib, with the majority occurring in the fourth to sixth ribs. Surgical resection combined with postoperative radiotherapy or chemotherapy appears to result in longer tumor recurrence-free survival. If the SP is in the left rib, attention should be paid to the differential diagnosis of angina pectoris to avoid misdiagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Aziz JMA, Iraq; Sung WY, South Korea; Surani S, United States; Teragawa H, Japan A-Editor: Hasan A, Egypt S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Caers J, Paiva B, Zamagni E, Leleu X, Bladé J, Kristinsson SY, Touzeau C, Abildgaard N, Terpos E, Heusschen R, Ocio E, Delforge M, Sezer O, Beksac M, Ludwig H, Merlini G, Moreau P, Zweegman S, Engelhardt M, Rosiñol L. Diagnosis, treatment, and response assessment in solitary plasmacytoma: updated recommendations from a European Expert Panel. J Hematol Oncol. 2018;11:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 180] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 2. | Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R. Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood. 2000;96:2037-2044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Burt M, Karpeh M, Ukoha O, Bains MS, Martini N, McCormack PM, Rusch VW, Ginsberg RJ. Medical tumors of the chest wall. Solitary plasmacytoma and Ewing's sarcoma. J Thorac Cardiovasc Surg. 1993;105:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Ikeda T, Minakata Y, Inui H, Yukawa S, Nomoto H, Tsujimoto M. A case of plasmacytoma of the ribs with intrathoracic tumors. Nihon Kyobu Shikkan Gakkai Zasshi. 1992;30:133-137. [PubMed] |
| 5. | Hihara J, Takeo S, Furuyama M, Saku M. A case of solitary plasmacytoma that originated in a rib. Nihon Kyobu Geka Gakkai Zasshi. 1993;41:456-460. [PubMed] |
| 6. | Hanawa T, Sawai S, Matsui T, Chiba W, Watanabe S, Matsubara Y, Hatakenaka R, Funatsu T, Ikeda S. A case of solitary plasmacytoma of the chest wall. Nihon Kyobu Shikkan Gakkai Zasshi. 1994;32:616-620. [PubMed] |
| 7. | Hirai T, Hamada Y, Kanou T, Kobayashi J, Endo K, Morishita Y. Solitary plasmacytoma of the rib--a case report and review of Japanese literatures. Nihon Kyobu Geka Gakkai Zasshi. 1995;43:205-209. [PubMed] |
| 8. | Mankodi AK, Rao CV, Katrak SM. Solitary plasmacytoma presenting as peripheral neuropathy: a case report. Neurol India. 1999;47:234-237. [PubMed] |
| 9. | Kadokura M, Tanio N, Nonaka M, Yamamoto S, Kataoka D, Kushima M, Kimura S, Nakamaki T, Sato I, Takaba T. A surgical case of solitary plasmacytoma of rib origin with biclonal gammopathy. Jpn J Clin Oncol. 2000;30:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Sato Y, Hara M, Ogino H, Kaji M, Yamakawa Y, Wakita A, Tateyama H. CT-pathologic correlation in a case of solitary plasmacytoma of the rib. Radiat Med. 2001;19:303-305. [PubMed] |
| 11. | George SM, Ratnakar KS, Shome DK, Nair R, Al Ajmi A. Plasmacytoma of the rib in young male. Asian Cardiovasc Thorac Ann. 2002;10:282-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Yan TQ, Guo W, Tang XD, Tang S. Clinical study of solitary bone plasmacytoma. Zhonghua Wai Ke Za Zhi. 2003;41:749-752. [PubMed] |
| 13. | Bousnina S, Zendah I, Marniche K, Yalaoui S, El Mezni F, Megdiche ML, Chabbou A. Solitary plasmocytoma of the rib: a rare tumor not to miss. Rev Pneumol Clin. 2006;62:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Xiao P, Lin P. A case report of solitary plasmacytoma of the rib. Ai Zheng. 2008;27:559-560. [PubMed] |
| 15. | Ketata W, Triki F, Msaad S, Ayadi L, Fouzi S, Ayadi H, Ayoub A. A rare localization of solitary plasmocytoma. Rev Pneumol Clin. 2009;65:165-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Pattanayak L, Samantaray S, Rout N. Solitary plasmacytoma of the rib: a rare cytological detection. Indian J Cancer. 2010;47:485-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Kodate M, Takagishi T, Osaki T. Plasmacytoma of chest wall. Kyobu Geka. 2010;63:879-882. [PubMed] |
| 18. | Singal R, Dalal U, Dalal AK, Attri AK, Gupta S, Raina R. Solitary plasmacytoma of the rib: A rare case. Lung India. 2011;28:309-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Lee HY, Kim JI, Kim KN. Solitary plasmacytoma of the rib. Korean J Thorac Cardiovasc Surg. 2012;45:269-271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Santos VM, Brito EF, Paz BC, Leal CT. Rib plasmacytoma and IgA multiple myeloma with hyperviscosity syndrome. Arch Iran Med. 2012;15:517-519. [PubMed] |
| 21. | Tajima K, Uchida N, Azuma Y, Okada T, Sasamoto H, Yokoo H, Kuwano H. Surgical resection of a solitary plasmacytoma originating in a rib. Ann Thorac Cardiovasc Surg. 2014;20 Suppl:609-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Razafimanjato NN, Ravoatrarilandy M, Rakotoarisoa AJ, Hasiniatsy R, Hunald AF, Rakototiana AF, Rafaramino F, Rakotovao HJ. Solitary plasmacytoma of the rib: about a case. Pan Afr Med J. 2014;18:179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | García Franco CE, Jiménez Hiscock L, Zapatero Gaviria J. Solitary plasmacytoma in a rib. Arch Bronconeumol. 2004;40:100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 24. | Caffery T, Foy M. Plasmacytoma presenting as missing rib on chest film: a case report and review of the literature. J La State Med Soc. 2014;166:63-66. [PubMed] |
| 25. | Jia R, Xue L, Liang H, Gao K, Li J, Zhang Z. Surgery combined with radiotherapy for the treatment of solitary plasmacytoma of the rib: a case report and review of the literature. J Cardiothorac Surg. 2015;10:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Singh V, Suraj AK, Mishra V, Ora M, Gambhir S. Rib Plasmacytoma With Unusual Sunburst Periosteal Reaction. Clin Nucl Med. 2020;45:461-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Pham A, Mahindra A. Solitary Plasmacytoma: a Review of Diagnosis and Management. Curr Hematol Malig Rep. 2019;14:63-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 64] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 28. | Dingli D, Kyle RA, Rajkumar SV, Nowakowski GS, Larson DR, Bida JP, Gertz MA, Therneau TM, Melton LJ 3rd, Dispenzieri A, Katzmann JA. Immunoglobulin free light chains and solitary plasmacytoma of bone. Blood. 2006;108:1979-1983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 100] [Article Influence: 5.3] [Reference Citation Analysis (0)] |