Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7013
Peer-review started: November 17, 2021
First decision: April 13, 2022
Revised: April 20, 2022
Accepted: May 27, 2022
Article in press: May 27, 2022
Published online: July 16, 2022
Processing time: 229 Days and 9.3 Hours
Asymmetric multifocal intraocular lenses (IOLs) are now widely used in the modern cataract surgery, providing a good level of visual performance over a range of distances and high postoperative patient satisfaction. We report a case of improved visual quality after shifting the near segment of an asymmetrical multifocal IOL to the superotemporal placement in the dominant eye of a glau
A 72-year-old woman with bilateral glaucoma underwent phacoemulsification in the dominant eye (left eye) with implantation of an asymmetrical multifocal IOL. Postoperative uncorrected distance visual acuity (UDVA) was 0.0 logMAR (20/20 Snellen) and uncorrected near visual acuity (UNVA) was 0.1 logMAR (20/25 Snellen). Two weeks later, the patient presented to our clinic with decreased vision due to migration of lens epithelial cells to IOL anterior surface and edema of corneal endothelial cells. Anterior capsule polishing and superotemporal placement of near segment [+3.00 diopter (D) addition (add)] of IOL were performed. As a result, UDVA at the first week and first year after reposition was 0.0 logMAR (20/20 Snellen), and compared with 0.3 logMAR (20/40 Snellen) in the first week, the UNVA was improved to 0.0 logMAR (20/20 Snellen) one year after surgery.
The postoperative inflammatory reaction and lens epithelial cells proliferation were obvious in this glaucoma patient. Capsule polishing and rotation of the lens were beneficial to the patient, which not only enhanced the patient's vision, but also improved the patient's satisfaction. Therefore, glaucoma patients need to be cautious of implanting multifocal IOLs. Placement of a near segment of an asymmetrical multifocal IOL in the dominant eye should be performed on an individual basis.
Core Tip: Based on the design concept of asymmetric region refraction, the placement of asymmetric multifocal intraocular lenses (IOLs) is particularly important. Here, we report the case of a glaucoma patient undergoing cataract surgery with an asymmetric multifocal IOL implanted in the dominant eye. After 2 wk, the lens epithelial cells proliferated rapidly and visual acuity decreased significantly, which was recovered after capsular polishing combined with IOL rotation. By reporting this case, we hope to provide new insights into the implantation of asymmetric multifocal IOLs in patients with glaucoma.
- Citation: Fan C, Zhou Y, Jiang J. Secondary positioning of rotationally asymmetric refractive multifocal intraocular lens in a patient with glaucoma: A case report. World J Clin Cases 2022; 10(20): 7013-7019
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7013.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7013
Cataract is the leading cause of blindness in the world. The development of the intraocular lens (IOL) and phacoemulsification as a technique for cataract removal could be considered as the two most significant strides that have been made in this surgical field[1]. With the development of science and technology, the choice of IOL is becoming more and more diversified and personalized. Asymmetric multifocal IOLs are now widely used in the modern cataract surgery, which provide excellent levels of visual performance at a range of distances as well as high postoperative patient satisfaction[2-4]. Asymmetrical multifocal IOLs, such as the SBL-3 (Lenstec, Inc.) as we mentioned in this case, provide their multifocality through a refractive design by incorporating a near vision section in the IOL[5]. Therefore, the SBL-3 is an asymmetric multifocal IOL with a +3.0 D near portion and a seamless transition zone between distance section and near section, and the asymmetric nature means that the position of the near segment must be considered.
A 72-year-old woman was referred to our clinic with a complaint of decreased visual acuity for 1 wk following cataract surgery performed in the left eye 2 wk ago.
The patient underwent an uneventful phacoemulsification cataract surgery for the left eye at our department 2 wk ago, and a rotationally asymmetric refractive multifocal IOL (SBL-3, Lenstec, Inc.) was chosen and implanted with the near segments placed inferonasally. The first day post-surgery, uncorrected distance visual acuity (UDVA) was 0.0 logMAR (20/20 Snellen) and uncorrected near visual acuity (UNVA) was 0.1 logMAR (20/25 Snellen). Preoperative biometric data are given in Table 1.
| Parameter | Left eye |
| Axial length (mm) | 22.46 |
| K1 (D) | 44.94 @ 55° |
| K2 (D) | 45.18 @ 145° |
| ACD (mm) | 2.23 |
| Angle kappa (mm) | 0.06 @ 56° |
| Angle alpha (mm) | 0.32 @ 28° |
| Total corneal astigmatism (D) | 1.0 |
The patient had bilateral primary angle closure glaucoma treated by laser peripheral iridectomy before at a local hospital, bilateral intraocular pressure was normal with no glaucoma medication before cataract surgery, and she had no history of allergies, trauma, surgery, or systemic disease.
The patient was married and had two sons. She had no family history of ocular disease.
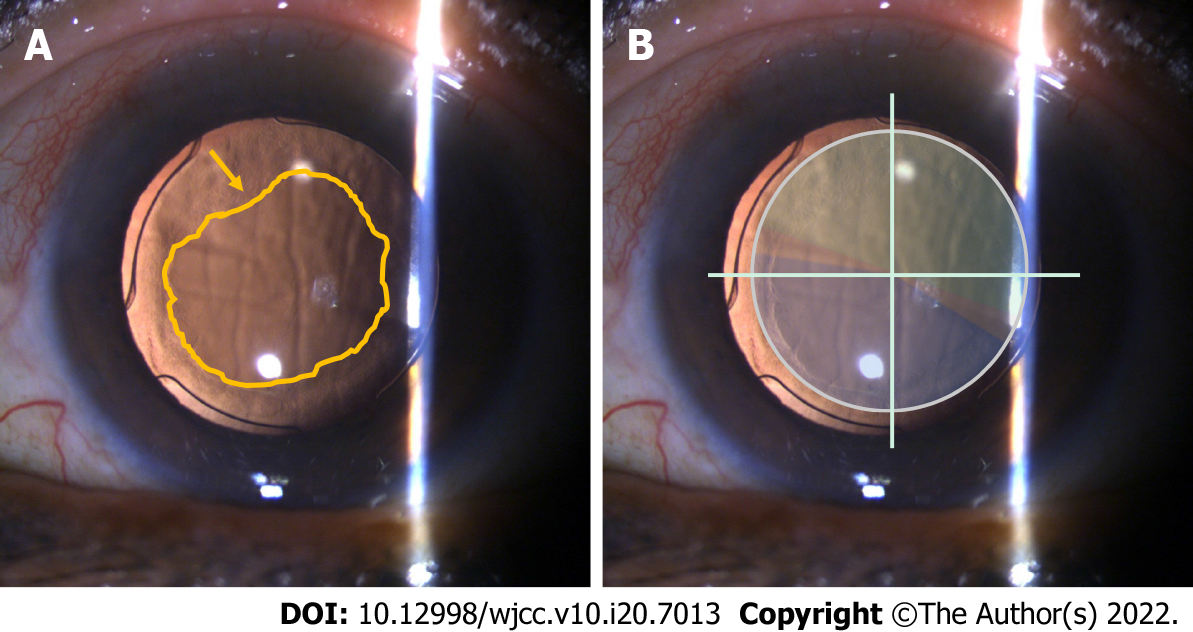
The patient presented to our clinic for reexamination with deterioration in the UDVA to 1.0 logMAR (20/200 Snellen) and in the corrected distant visual acuity of 1.0 logMAR (20/200 Snellen). Using a slit lamp, the swelling of the corneal endothelium and proliferation of lens epithelial cells crawling over the surface of the IOL could be clearly seen. Meanwhile, the IOL was in positive position, without any tilt or decentration, and the near segment was located in inferonasal orientation (Figure 1).
IOL (left), complicated cataract (right), primary angle closure glaucoma (both), and status after laser peripheral iridectomy (both).
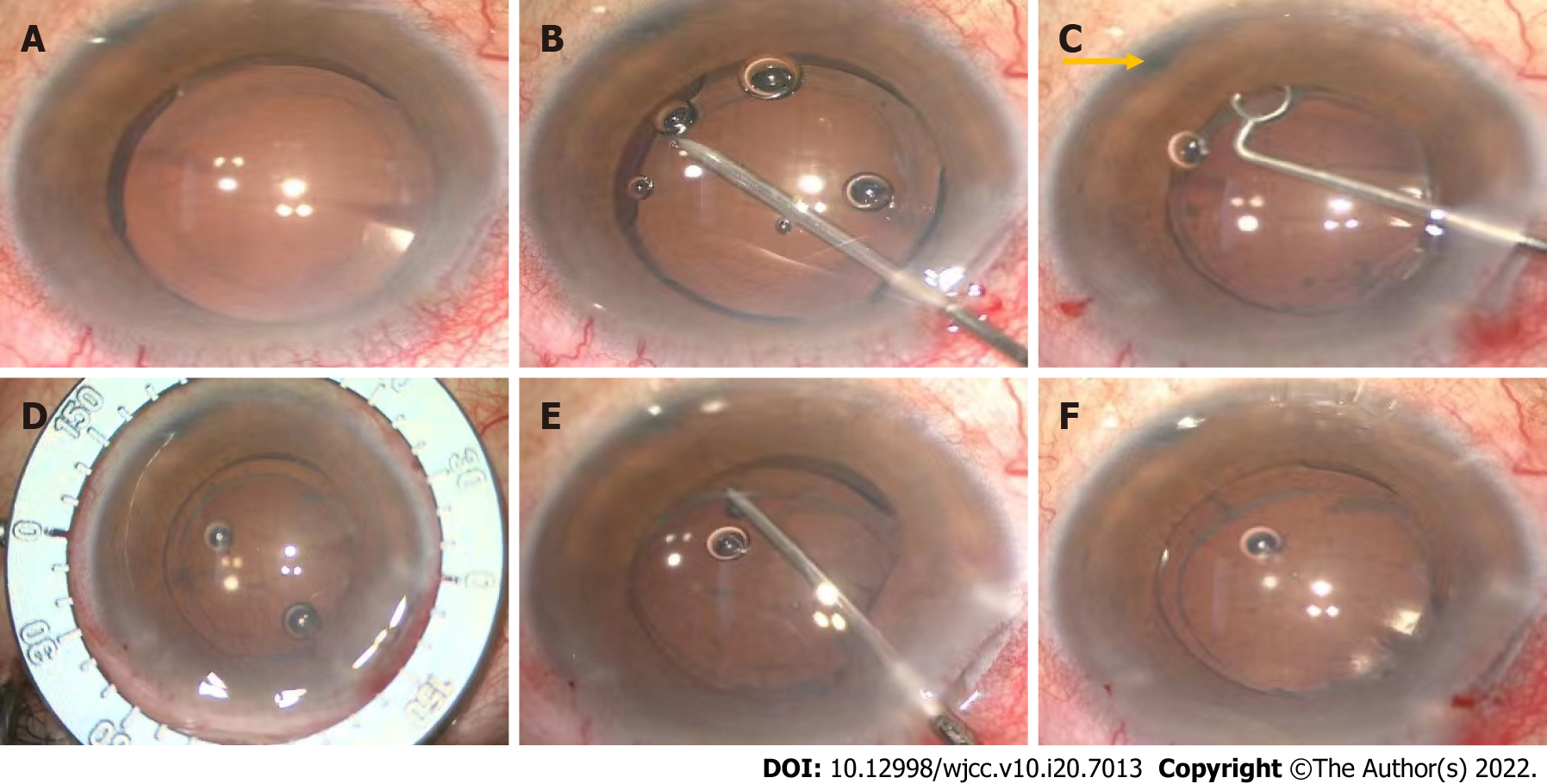
We performed surgery for polishing the capsule and repositioning the IOL. During surgery, the anterior capsule was polished with a polisher to reduce the incidence of capsular contraction syndrome and posterior capsular opacification (PCO). Meanwhile, the near segment of IOL was shifted to the superotemporal placement, and coinciding transition zone of IOL with angle Kappa was avoided. At the end of the operation, the central position of the IOL was checked to see whether the light projection of the microscope was on the central point of IOL (Figure 2). Postoperatively, the patient was treated with a schedule of levofloxacin 0.5%, prednisolone, and pranoprofen eyedrops for 4 wk.
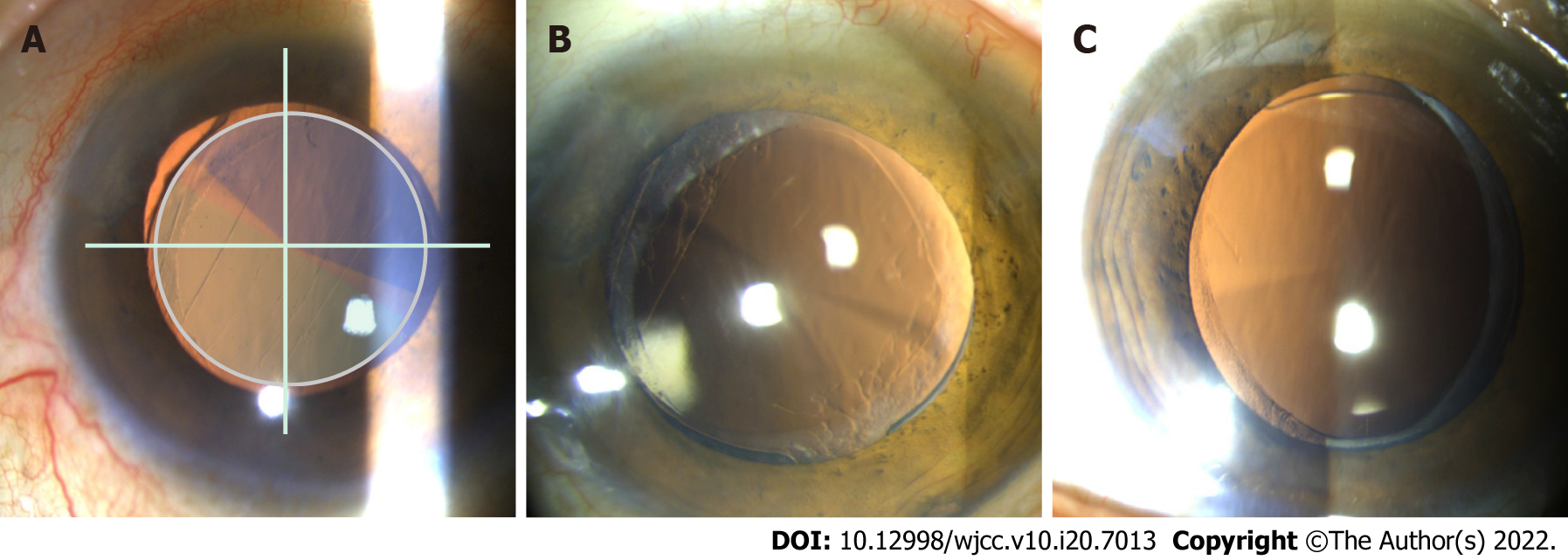
The first day after rotation, UDVA and UNVA were 0.2 logMAR (20/32 Snellen) and 0.3 logMAR (20/40 Snellen), respectively. UDVA improved to 0.0 logMAR (20/20 Snellen) 1 wk later (Table 2), and the intraocular pressure was 16 mmHg, which have remained stable during follow-up. One year after rotation, when she checked again, we found that she had a cataract surgery on her right eye at another hospital half a year ago, and the type of the IOL was the same as that on the left. In addition, the near segment of the lens on the right was positioned inferiorly with slight nasal deviation. For the right eye, UDVA and UNVA were 0.0 logMAR (20/20 Snellen) and 0.10 logMAR (20/25 Snellen), respectively. While for the left eye, UDVA and UNVA were 0.0 logMAR (20/20 Snellen) and 0.0 logMAR (20/20 Snellen), respectively. After a series of examinations, the lens position of the left eye was still positive, which almost was unchanged from the previous. Visual quality was assessed using OPD Scan III (Nidek Inc., Tokyo, Japan), and the tilt was acceptable in both horizontal and vertical directions without adversely affecting visual quality. At the same time, the lens position was also positive with no obvious tilt when viewed using ultrasound biomicroscopy (Supplementary Figure 1). The patient was very satisfied with the distant and near visual acuity, and achieved excellent visual performance.
| Preoperative | Postoperative 1 d | Postoperative 2 wk | 1 d after rotation | 1 wk after rotation | 1 yr after rotation | |
| UDVA | 0.2 (20/32 Snellen) | 0.0 (20/20 Snellen) | 1.0 (20/200 Snellen) | 0.2 (20/32 Snellen) | 0.0 (20/20 Snellen) | 0.0 (20/20 Snellen) |
| CDVA | 0.05 (20/25 Snellen) | 0.0 (20/20 Snellen) | 1.0 (20/200 Snellen) | 0.1 (20/25 Snellen) | 0.0 (20/20 Snellen) | 0.0 (20/20 Snellen) |
| UNVA | 1.0 (20/200 Snellen) | 0.1 (20/25 Snellen) | 0.5 (20/63 Snellen) | 0.3 (20/40 Snellen) | 0.3 (20/40 Snellen) | -0.10 (20/16 Snellen) |
We speculated the reasons for deterioration of postoperative visual quality, such as postoperative inflammation which could lead to proliferation of lens epithelial cells and migration to the anterior surface of IOL, and even corneal endothelial edema and opacity of refractive media. The unique functional and structural characteristics of glaucoma patients lead to an increased risk of PCO, inflammation, and anterior capsular opacification[6-8]. Above all, although the patient’s eyesight reflected well numerically, when we repeatedly confirmed her subjective experience on the first day postoperatively, there was no inflammatory reaction and no proliferation of lens epithelial cells, and the patient emphasized that she felt clearly in near vision while obscurely in distant vision. Consequently, we conjectured that lens position might play a key role. Given that the lens was a plate-haptic design for excellent stability, it will be more difficult to rotate it later. Meanwhile, anterior capsule polishing is a method to prevent the occurrence of PCO and enhance visual function[9]. Here, we decided to perform surgery for polishing capsule and repositioning the IOL in the same operation, trying to enhance the patient's visual quality and reduce the patient’s complaints and pain.
Why did we choose to rotate the near segment to the superotemporal position rather than somewhere else? SBL-3, as mentioned in this case, is designed based on the concept of asymmetric regional refraction, and the choice of its placement position appears to be particularly important. A study by de Wit et al[10] found that the difference between inferonasal near add positioning and superotemporal near add positioning was not statistically significant. What’s more, whether the near segment is positioned inferiorly, superiorly, or temporally, there was no significant effect on visual performance[11]. A study by McNeely et al[5] found that bilateral implantation of asymmetric multifocal IOLs with a combination of superotemporal placement of the near segment in the dominant eye and inferonasal placement of the near segment in the fellow eye enhanced quality of vision and reduced symptoms such as glare and halo compared with bilateral inferonasal placement. In our case, we chose to shift the near segment to the superotemporal position in the dominant eye (Figure 3); coincidentally, the near segment of the lens of the fellow eye was positioned inferonasally. The patient’s satisfactory postoperative results confirmed the feasibility of the mix and match placement scheme.
Because of its asymmetrical design, tilt and decentration had a prominent effect on optical quality with the rotational asymmetric multifocal IOL in vitro. Liu et al[12] found that the decentration induced increased or decreased optical quality, but tilt yielded decreased optical quality at different orientations. Pazo et al[13] also demonstrated that rotation of the asymmetric IOL can be used to both recenter the IOL and increase the required surface area of either distance or near component within the physiological pupil, thereby optimizing visual outcomes. These are all important considerations when using this asymmetric multifocal IOL.
There has been considerable debate over whether multifocal IOL implantation is a suitable choice for glaucoma patients. Studies have shown that glaucoma patients can benefit from multifocal IOL technology and achieve spectacle independence with no significant adverse effects[14]. Use of these IOLs in the presence of concurrent eye diseases has not been extensively studied. Thus, decisions regarding the choice of a multifocal IOL in patients with glaucoma must be made on an individual basis, with patient motivation and expectation being a prime mover. The rate of progression of glaucoma in an individual patient is also an important consideration[15].
The postoperative inflammatory reaction and lens epithelial cell proliferation were obvious in this glaucoma patient. Capsule polishing and rotation of the lens were beneficial to the patient, which not only enhanced the patient's vision, but also improved the patient's satisfaction. Glaucoma patients need to be cautious of implanting multifocal IOLs. Placement of a near segment of an asymmetrical multifocal IOL in the dominant eye should be performed on an individual basis. Although cataract surgery for glaucoma patients may be challenging, it affords an opportunity to dramatically improve the quality of life of patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chrcanovic BR, Sweden; Chrcanovic BR, Sweden A-Editor: Liu X, China S-Editor: Gao CC L-Editor: Wang TQ P-Editor: Gao CC
| 1. | Fraser IS. Relationship between gonadotrophin-releasing hormone analogue therapy and bone loss; a review. Reprod Fertil Dev. 1991;3:61-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Venter JA, Barclay D, Pelouskova M, Bull CE. Initial experience with a new refractive rotationally asymmetric multifocal intraocular lens. J Refract Surg. 2014;30:770-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Wang X, Tu H, Wang Y. Comparative Analysis of Visual Performance and Optical Quality with a Rotationally Asymmetric Multifocal Intraocular Lens and an Apodized Diffractive Multifocal Intraocular Lens. J Ophthalmol. 2020;2020:7923045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Moore JE, McNeely RN, Pazo EE, Moore TC. Rotationally asymmetric multifocal intraocular lenses: preoperative considerations and postoperative outcomes. Curr Opin Ophthalmol. 2017;28:9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | McNeely RN, Pazo E, Spence A, Richoz O, Nesbit MA, Moore TC, Moore JE. Comparison of the visual performance and quality of vision with combined symmetrical inferonasal near addition vs inferonasal and superotemporal placement of rotationally asymmetric refractive multifocal intraocular lenses. J Cataract Refract Surg. 2016;42:1721-1729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Teichman JC, Ahmed II. Intraocular lens choices for patients with glaucoma. Curr Opin Ophthalmol. 2010;21:135-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Quigley HA. Long-term follow-up of laser iridotomy. Ophthalmology. 1981;88:218-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 113] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Liebmann JM, Ritch R. Laser surgery for angle closure glaucoma. Semin Ophthalmol. 2002;17:84-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Han MY, Yu AH, Yuan J, Cai XJ, Ren JB. Effect of anterior capsule polish on visual function: A meta-analysis. PLoS One. 2019;14:e0210205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | de Wit DW, Diaz J, Moore TC, Moutari S, Moore JE. Effect of position of near addition in an asymmetric refractive multifocal intraocular lens on quality of vision. J Cataract Refract Surg. 2015;41:945-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Song IS, Yoon SY, Kim JY, Kim MJ, Tchah H. Influence of Near-Segment Positioning in a Rotationally Asymmetric Multifocal Intraocular Lens. J Refract Surg. 2016;32:238-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Liu X, Xie L, Huang Y. Effects of decentration and tilt at different orientations on the optical performance of a rotationally asymmetric multifocal intraocular lens. J Cataract Refract Surg. 2019;45:507-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Pazo EE, Richoz O, McNeely R, Millar ZA, Moore TC, Moore JE. Optimized Visual Outcome After Asymmetrical Multifocal IOL Rotation. J Refract Surg. 2016;32:494-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Ouchi M, Kinoshita S. Implantation of refractive multifocal intraocular lens with a surface-embedded near section for cataract eyes complicated with a coexisting ocular pathology. Eye (Lond). 2015;29:649-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Kumar BV, Phillips RP, Prasad S. Multifocal intraocular lenses in the setting of glaucoma. Curr Opin Ophthalmol. 2007;18:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |