Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6991
Peer-review started: November 12, 2021
First decision: March 15, 2022
Revised: March 29, 2022
Accepted: May 22, 2022
Article in press: May 22, 2022
Published online: July 16, 2022
Processing time: 234 Days and 16.9 Hours
A radicular groove is an anatomic malformation that usually initiates at the central fossa, extending along the root at varying lengths and depths and predisposes the involved tooth to a severe periodontal defect. Severe grooves that extend to the root apex often lead to complex combined periodontal-endodontic lesions. They are a serious challenge for doctors to diagnose and treat.
In this report, we described a patient with a maxillary lateral incisor with a deep palatogingival groove with two roots, which led to complex combined perio
Intentional replantation and root resection offer a predictable procedure and should be considered a viable treatment modality for the management of palatogingival grooves, especially for two-rooted teeth.
Core Tip: We present a case of type III radicular groove with complex combined periodontal-endodontic lesions in a tooth, which was successfully treated by a combination of endodontic therapy, intentional replantation, and root resection. Sufficient knowledge about the diagnosis and treatment strategies and multidisciplinary involvement are essential to obtain the best outcome in a short period with a conservative and minimally periodontal trauma procedure.
- Citation: Tan D, Li ST, Feng H, Wang ZC, Wen C, Nie MH. Intentional replantation combined root resection therapy for the treatment of type III radicular groove with two roots: A case report. World J Clin Cases 2022; 10(20): 6991-6998
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6991.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6991
A radicular groove is an anatomic malformation that usually initiates at the central fossa, extending along the root at varying lengths and depths. These malformations are associated with the maxillary incisors and has an incidence of 3%-18%[1-6]. According to the latest classification standards, radicular grooves are classified into three types based on the depth and length of the groove and cross-sectional shape on cone-beam computed tomography (CBCT) images: type I, with a shallow groove depth, corresponding to a normal, simple, and single root canal; type II, with a medium groove depth, corresponding to a C-shaped canal system; and type III, with a deep groove depth, almost bisecting the root of the tooth, simultaneously present with two independent root canals and an apex with a normal shape, corresponding to a labial groove connecting with a palatal groove[4,7-9].
The depth and length of groove determines the prognosis; the deeper the groove, the worse the prognosis. Previously, teeth with severe radicular grooves were usually extracted because of the combined periodontal-endodontic lesions and a hopeless prognosis. Previously, operators have attempted to save these teeth by a variety of therapies, such as scaling and root planing, periodontal regeneration, guided periodontal tissue regeneration, and endodontic surgery; however, the prognosis is unfavorable[10-14].
In this report, we described a 16-year-old boy with a maxillary lateral incisor with type III radicular groove (deep radicular groove extending to the root apex and with two independent root canals). In this case, a combination of endodontic therapy, intentional replantation, and radectomy were used, resulting in periodontal healing and healing of the periradicular radiolucency after 12 mo. At 1-year follow-up, the patient was comfortable and complete resolution of the periapical pathology was evident.
A 16-year-old boy presented to our clinic complaining of the gum pustule with suppuration.
The gum pustule was found by accident 3 d ago without special treatment.
The patient had a negative medical history, and he denied a history of trauma.
Denial of personal and family history.
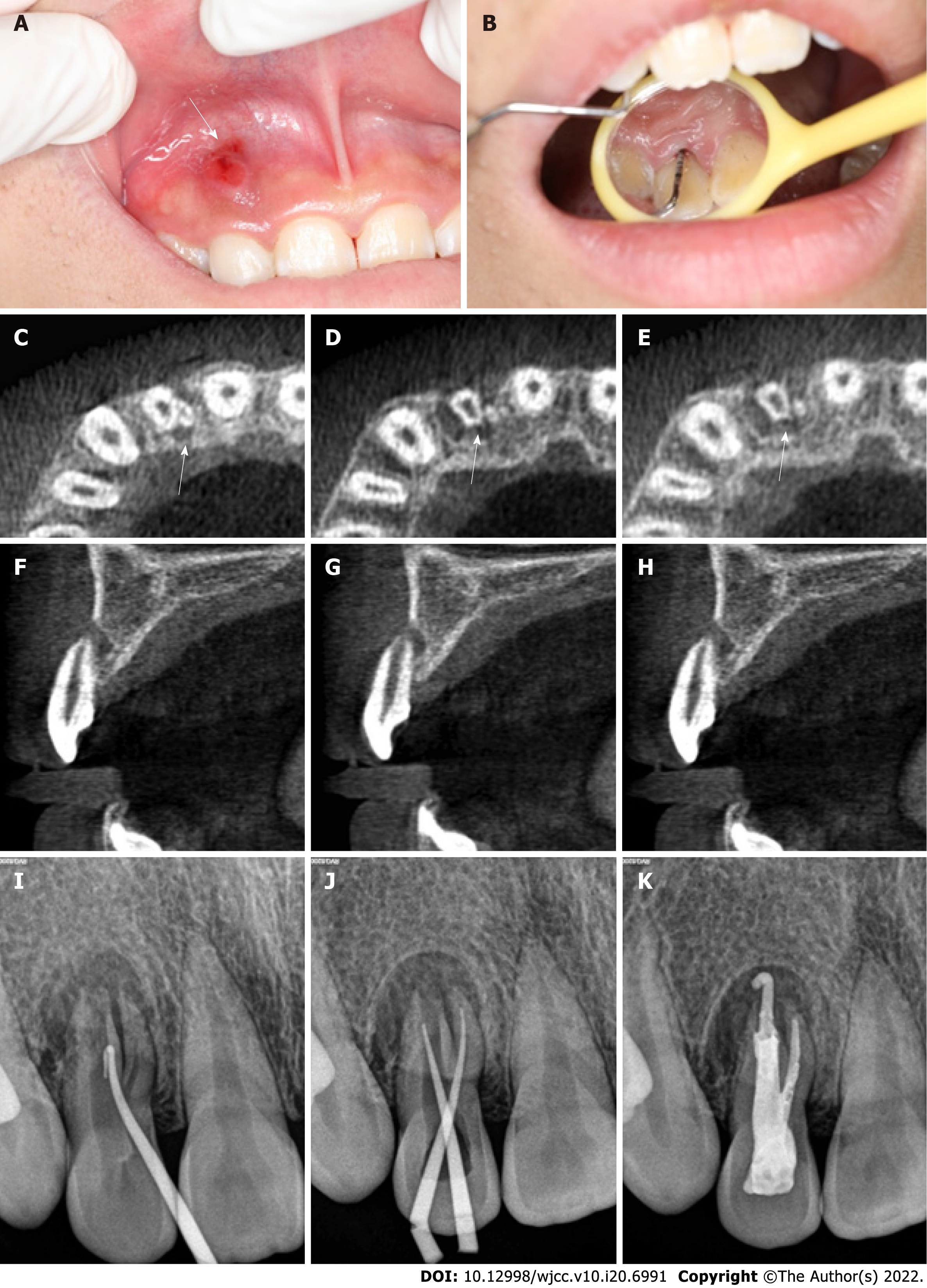
Visual examination revealed a draining sinus tract on the labial gingival surface associated with the maxillary right lateral incisor (tooth #12) (Figure 1A). Thermal and electric pulp vitality tests were negative. A radicular groove was detected, extending from the cingulum to the gingival sulcus, and clinical probing depth was 13 mm almost to the root apex. (Figure 1B).
Blood tests disclosed a slight increase of red blood cell (5.7 × 1012/L).
CBCT imaging confirmed that the palatogingival groove extended to the root apex, and a combined endodontic and periodontal origin lesion was identified (Figure 1C-H). A radiograph taken with a gutta-percha cone introduced through the sinus tract that showed that the affected tooth had two roots with large periradicular radiolucency (Figure 1I).
Based on the clinical (clinical periodontal probing of 13 mm, pulp vitality tests were negative) and radiographic (CBCT imaging disclosed the palatogingival groove extended to the root apex) evidence, diagnosis of radicular groove combined periodontal-endodontic lesions was established.
Although the prognosis of the tooth was questionable, the patient elected conservative treatment after the possible complications were explained. After sufficient doctor-patient communication, the treatment plan consisted of intentional replantation with endodontic and root resection.
The tooth was isolated with a rubber dam, and endodontic treatment was initiated (Figure 1J and K). Working length was established with the help of an electronic apex locator (J Morita Manufacturing, Kyoto, Japan), and chemomechanical preparation was performed in a crown-down manner with copious irrigation with 2.0% sodium hypochlorite solution. Intracanal calcium hydroxide dressing was placed (Prime Dental Products, Mumbai, India). After 8 wk, the patient was asymptomatic. Root canal obturation was completed with guttapercha and AH-Plus root canal sealer (Dentsply, Petropolis, Brazil), and the access cavity was restored with composite resin (Esthet X HD; Dentsply) at this visit.
Twelve weeks later, however, the sinus tract had not healed, with a depth of clinical periodontal probing of 13 mm. At that time, it was decided to perform an intentional reimplantation procedure[6]. The details, possible benefits, and risks of the procedure were explained to the patient, and written consent was obtained.
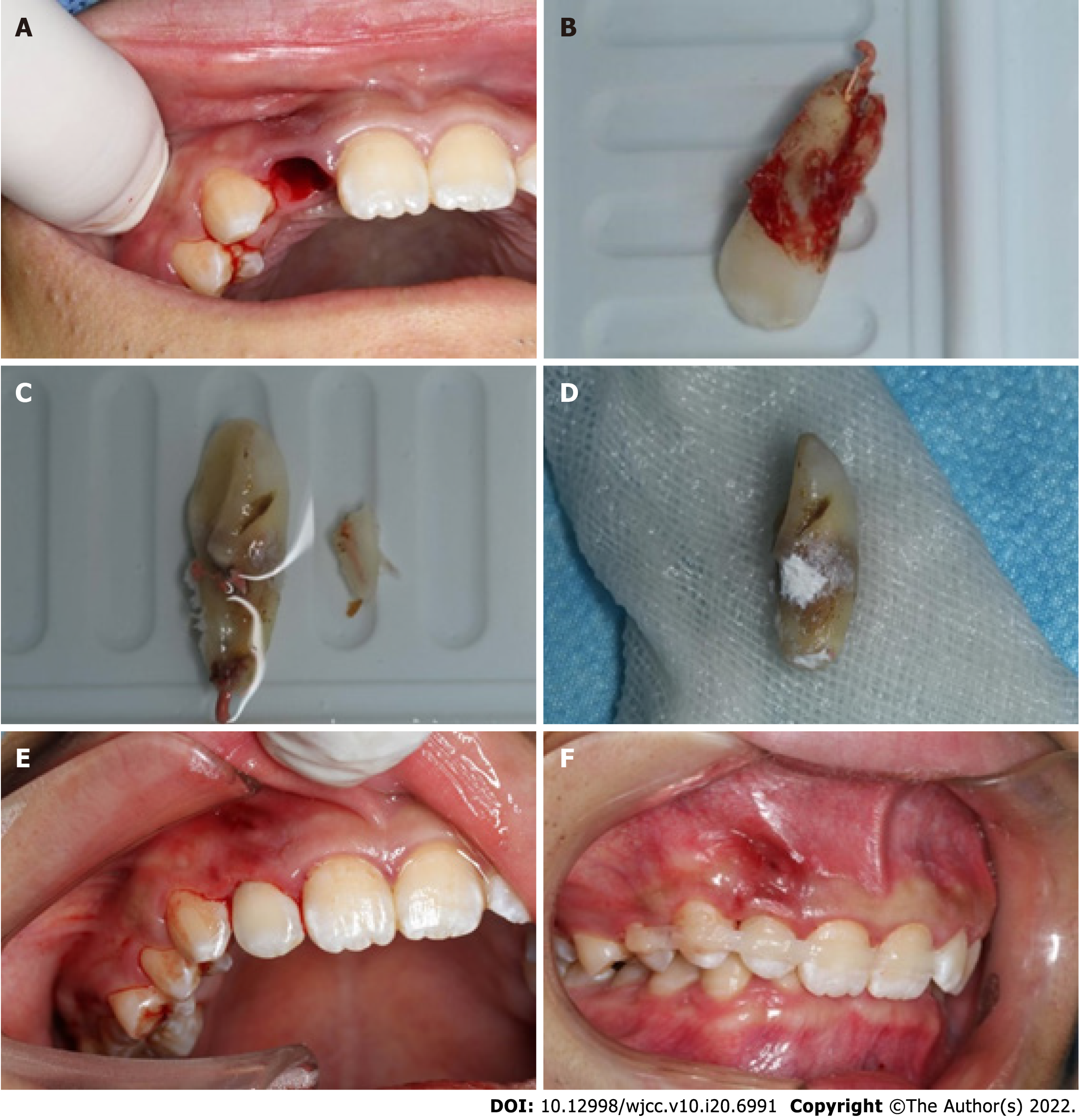
Local single tooth anesthesia (STA) of 2% lidocaine with 1:100000 epinephrine was applied using the electronic STA Wand System (Milestone Scientific, Livingston, NJ, United States). The tooth was extracted atraumatically with forceps, and the periodontal ligament remained intact (Figure 2A). During the extraction, the tooth was gently held by the crown with physiological-saline-soaked gauze, and the root was continuously rinsed with plenty of saline. Under a dental operating microscope (OPMI ProErgo; Carl Zeiss, Oberkochen, Germany), the tooth was divided into two independent root canals and an apex with a normal shape by the radicular groove that extended from the central fossa to the root apex (Figure 2B). Along the radicular groove, we used a fissure bur to remove the small root (Figure 2C). About 3-mm length of the main root end was resected, and root-end preparation was performed with a #700 fissure bur. Root tips were back-filled with iRoot BP Plus Root Repair Material (Innovative BioCeramix, Vancouver, BC, Canada) (Figure 2D). The complete extraoral procedure lasted < 8 min. The tooth was then replanted into its alveolar bone (Figure 2E) and splinted with a flexible splint for 1 wk (Figure 2F)[15-18]. Antibiotic therapy (amoxicillin plus clavulanic acid 1 g daily) was given by oral administration for 1 wk, and soft brushing was recommended, avoiding the surgical site for the first 48 h. The use of 0.12% chlorhexidine gluconate was recommended to maintain oral hygiene measures[19,20]. The patient was informed of review at 1, 3, 6, and 12 mo after the procedure.
Postsurgical healing was favorable, and the sinus tract was significantly reduced at the 1 wk postoperative visit (Figure 3A-C). At the 1-mo recall, the sinus tract was closed, and radiography showed a reduction in the periapical lesion. The clinical probing depth was 3 mm, indicating that the periapical tissue was healing (Figure 3D-F). At the 3-mo recall, radiography showed no periapical lesion, and the tooth was asymptomatic with no periodontal pocket, which indicated almost complete periapical healing (Figure 3G-I). At the 6-mo recall, clinical and radiographic examination revealed complete periapical healing (Figure 3J-L). At the 12-mo recall, the tooth remained asymptomatic, and the patient was comfortable. CBCT imaging showed that the periapical tissue was normal (Figure 3M-O).
The radicular groove is an ideal access for oral bacteria to invade periodontal tissues and cause periodontal damage, and concomitant pulp necrosis and/or apical periodontitis, which present a dilemma in terms of diagnosis and treatment planning[20]. Previously, teeth with type III palatal radicular grooves were usually extracted because of the complicated endoperiodontal damage and hopeless prognosis[15-18]. Intentional replantation has the characteristics of minimal invasion, good vision, short treatment time, and fast recovery[21]. Recently, there have been reports of significant results in the treatment of radicular groove (with endo - periodontal lesion) by using this method[22-25]. The main steps were the minimally invasive extraction of the affected tooth, resection of the root end, filling of both palatogingival groove and the root apex iroot BP, replantation of the affected tooth into the alveolar socket, and periodontal splinting. These cases are usually type II with one root[26-28].
According to Gu’s classification system[7-9], the present case belonged to type III because it presented with a shallow and deep groove that extended to the root apex, with a complex root canal system and an extra root. If we follow the method proposed in the previous literature, we could not eliminate the groove by filling with biological material (iroot BP) because of the two independent roots. Therefore, we used previous literature to guide a novel intervention for this patient. The only way to eliminate the infected pathway (the radicular groove) is to remove the root; therefore, we adopted intentional replantation and radectomy. Since we did not scratch the alveolar fossa to remain the periodontal ligament intact, the infection of the root tip was serious, which was not suitable for guided bone regeneration (GBR). Moreover, GBR would increase the difficulty of replanting the teeth to the appropriate position, which might cause occlusion trauma. We considered that if the effect of this operation was not ideal, later GBR might be needed, but did not choose to perform simultaneous surgery.
During the follow-up, the outcome of the procedure was favorable. There was an acceptable healing process. The patient’s initial complaints had resolved. Significant healing could be detected in the clinical examination (the sinus tract and the depth of clinical probing depth). The follow-up radiographs showed bone deposition in the affected area, as evidenced by the reduced area of radiolucency. Based on this, it was decided that intentional replantation and radectomy would be sufficient, and no further surgical (GBR) would be needed.
The most important concern related to the procedure is preserving the periodontal ligament (PDL) and the extraoral time[26], which should be as short as possible. Many researchers have emphasized the importance of preserving the PDL and limiting the extraoral time to 30 min. An extraoral time greater than 30 min increases the possibility of replacement resorption. In this case, the tooth was held gently at both the crown and root with gauze soaked in physiologic saline. The total extraoral time was only 7 min, allowing to the root surface to enhance PDL fiber attachment or prevent ankylosis[28].
In practice, to improve the treatment success of endodontic-periodontal disease which caused by radicular grooves, the clinicians must have sufficient knowledge concerning the etiology, classification, diagnosis, and treatment strategies of the condition. The complexity of such lesions makes diagnosis and treatment more difficult. Therefore, detailed extraoral and intraoral examination, periapical and CBCT radiographic imaging, periodontal analysis, and the application of additional tests to check for the tooth vitality should be performed to improve our understanding of the detail of the case, which can guide the clinicians towards a proper treatment plan. What's more, we should grasp the details of the operation to improve the success of the operation. In this case report, the intentional replantation combined endodontic and radectomy provides a viable option for the management of type III radicular grooves with two independent root canals.
The authors appreciate the help of the nursing staff for their help with imaging data.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Galiatsatos A, Greece; Ozden F, Turkey; Pameijer CH, United States; Rakhshan V, Iran; Santos FA, Brazil A-Editor: Liu X, China S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Lee KW, Lee EC, Poon KY. Palato-gingival grooves in maxillary incisors. A possible predisposing factor to localised periodontal disease. Br Dent J. 1968;124:14-18. [PubMed] |
| 2. | Kogon SL. The prevalence, location and conformation of palato-radicular grooves in maxillary incisors. J Periodontol. 1986;57:231-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Choi YH, Bae JH, Kim YK, Kim HY, Kim SK, Cho BH. Clinical outcome of intentional replantation with preoperative orthodontic extrusion: a retrospective study. Int Endod J. 2014;47:1168-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Zhu J, Wang X, Fang Y, Von den Hoff JW, Meng L. An update on the diagnosis and treatment of dens invaginatus. Aust Dent J. 2017;62:261-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | August DS. The radicular lingual groove: an overlooked differential diagnosis. J Am Dent Assoc. 1978;96:1037-1039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Peer M. Intentional replantation - a 'last resort' treatment or a conventional treatment procedure? Dent Traumatol. 2004;20:48-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Wei PC, Geivelis M, Chan CP, Ju YR. Successful treatment of pulpal-periodontal combined lesion in a birooted maxillary lateral incisor with concomitant palato-radicular groove. A case report. J Periodontol. 1999;70:1540-1546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Rethman MP. Treatment of a palatal-gingival groove using enamel matrix derivative. Compend Contin Educ Dent. 2001;22:792-797. [PubMed] |
| 9. | Becker BD. Intentional Replantation Techniques: A Critical Review. J Endod. 2018;44:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Xuelian T, Lan Z, Dingming H. [Intentional replantation for the treatment of palatal radicular groove with endo-periodontal lesion in the maxillary lateral incisor: a case report]. Hua Xi Kou Qiang Yi Xue Za Zhi. 2017;35:448-452. [PubMed] |
| 11. | Mittal M, Vashisth P, Arora R, Dwivedi S. Combined endodontic therapy and periapical surgery with MTA and bone graft in treating palatogingival groove. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Simon JH, Glick DH, Frank AL. Predictable endodontic and periodontic failures as a result of radicular anomalies. Oral Surg Oral Med Oral Pathol. 1971;31:823-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Robison SF, Cooley RL. Palatogingival groove lesions: recognition and treatment. Gen Dent. 1988;36:340-342. [PubMed] |
| 14. | Everett FG, Kramer GM. The disto-lingual groove in the maxillary lateral incisor; a periodontal hazard. J Periodontol. 1972;43:352-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 86] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Forero-López J, Gamboa-Martínez L, Pico-Porras L, Niño-Barrera JL. Surgical management with intentional replantation on a tooth with palato-radicular groove. Restor Dent Endod. 2015;40:166-171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Ennes JP, Lara VS. Comparative morphological analysis of the root developmental groove with the palato-gingival groove. Oral Dis. 2004;10:378-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Kim HJ, Choi Y, Yu MK, Lee KW, Min KS. Recognition and management of palatogingival groove for tooth survival: a literature review. Restor Dent Endod. 2017;42:77-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Tan XL, Chen X, Fu YJ, Ye L, Zhang L, Huang DM. Diverse microbiota in palatal radicular groove analyzed by Illumina sequencing: Four case reports. World J Clin Cases. 2021;9:6846-6857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 19. | Al-Hezaimi K, Naghshbandi J, Simon JH, Oglesby S, Rotstein I. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy. Dent Traumatol. 2004;20:226-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Gound TG, Maze GI. Treatment options for the radicular lingual groove: a review and discussion. Pract Periodontics Aesthet Dent. 1998;10:369-375; quiz 376. [PubMed] |
| 21. | Cortellini P, Pini Prato G, Tonetti MS. Periodontal regeneration of human infrabony defects. I. Clinical measures. J Periodontol. 1993;64:254-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 195] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 22. | Vermeersch G, Leloup G, Delmée M, Vreven J. Antibacterial activity of glass-ionomer cements, compomers and resin composites: relationship between acidity and material setting phase. J Oral Rehabil. 2005;32:368-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Corbella S, Alberti A, Zotti B, Francetti L. Periodontal Regenerative Treatment of Intrabony Defects Associated with Palatal Grooves: A Report of Two Cases. Case Rep Dent. 2019;2019:8093192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Grossman LI. Intentional replantation of teeth: a clinical evaluation. J Am Dent Assoc. 1982;104:633-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 36] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Yu YH, Kim M, Kratchman S, Karabucak B. Surgical management of lateral lesions with intentional replantation in single-rooted mandibular first premolars with radicular groove: 2 case reports. J Am Dent Assoc. 2022;153:371-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Yan H, Xu N, Wang H, Yu Q. Intentional Replantation with a 2-segment Restoration Method to Treat Severe Palatogingival Grooves in the Maxillary Lateral Incisor: A Report of 3 Cases. J Endod. 2019;45:1543-1549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Plotino G, Abella Sans F, Duggal MS, Grande NM, Krastl G, Nagendrababu V, Gambarini G. Clinical procedures and outcome of surgical extrusion, intentional replantation and tooth autotransplantation - a narrative review. Int Endod J. 2020;53:1636-1652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 28. | Al-Hezaimi K, Naghshbandi J, Simon JH, Rotstein I. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy: four years follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e82-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |