Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6966
Peer-review started: September 27, 2021
First decision: March 7, 2022
Revised: April 9, 2022
Accepted: May 22, 2022
Article in press: May 22, 2022
Published online: July 16, 2022
Processing time: 280 Days and 8.2 Hours
To report an unusual case of bilateral optic disc coloboma associated with macular retinoschisis in the left eye.
A 37-year-old woman presented with complaints of blurred and distorted vision in her left eye for more than 1 year. Fundus examination demonstrated choroidal atrophy around the optic disc in both eyes, with a cup-to-disc ratio of 0.9. Serous retinal detachment in the macular area of the left eye. Left eye macular blood flow imaging optical coherence tomography (Angio-OCT) showed macular retinal serous cleavage. En-face OCT showed that the canal gully-like structure formed by the defect of the optic disc nerve fiber layer between the optic disc and macula, serous detachment area was connected with the enlarged optic disc coloboma through the canal gully-like structure, and the fluid leaked from the enlarged and thinned optic disc coloboma into the retinal layer of the macular area. Patients with optic disc abnormalities and macular degeneration must be monitored appropriately. During the follow-up period, the use of optic disc stereography and 3D-OCT, en-face, and Angio-OCT imaging can clarify the correlation between macular retinoschisis and optic disc coloboma.
Macular retinoschisis may be owing to the combined force of disc edge loss, enlarged optic disc coloboma, the canal gully-like structure formed by the defect of the nerve fiber layer around the optic disc, and the traction of the posterior vitreous cortex.
Core Tip: We reported an unusual case of bilateral optic disc coloboma associated with macular retinoschisis in the left eye. Macular retinoschisis may be owing to the combined force of disc edge loss, enlarged optic disc coloboma, the canal gully-like structure formed by the defect of the nerve fiber layer around the optic disc, and the traction of the posterior vitreous cortex.
- Citation: Zhang W, Peng XY. Optic disc coloboma associated with macular retinoschisis: A case report. World J Clin Cases 2022; 10(20): 6966-6973
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6966.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6966
Clinically, optic disc coloboma is considered a bowl-shaped depression. The frequency of unilateral and bilateral occurrence is similar, and it is mostly owing to congenital optic disc abnormalities, physiological large optic cups, glaucoma optic disc cupping, and optic nerve atrophic coloboma[1-3]. Optic disc coloboma can cause abnormal visual fields[4-6]. The author found that optic disc coloboma is related to serous macular retinoschisis, which is similar to optic disc pit-related macular serous retinoschisis[7-9]. The literature regarding optic disc coloboma associated with macular retinoschisis is limited.
A 37-year-old woman presented with complaints of blurred and distorted vision in her left eye for more than 1 year.
There was no family history of ocular diseases. One month ago, she was diagnosed with left eye macular retinoschisis, and optic disc pit and underwent a left eye vitrectomy in another hospital.
The patient had no systemic diseases.
There was no family history of ocular diseases.
Ophthalmic examination showed the unaided visual acuity was 20/1000 in the right eye which was improving up to 20/20 (with -10.25 D) and 20/1000 in the left eye, improving up to 20/200 (with -10.75 D). Intraocular pressure (IOP) measured with Goldmann applanation tonometry was 10 mmHg and 12 mmHg in the right and left eye respectively. Examination of the anterior segment of both eyes showed no abnormality. Gonioscopy examination showed the normal width of the anterior chamber angle of both eyes. Fundus examination demonstrated choroidal atrophy around the optic disc in both eyes, with a cup-to-disc ratio of 0.9. Serous retinal detachment in the macular area of the left eye.
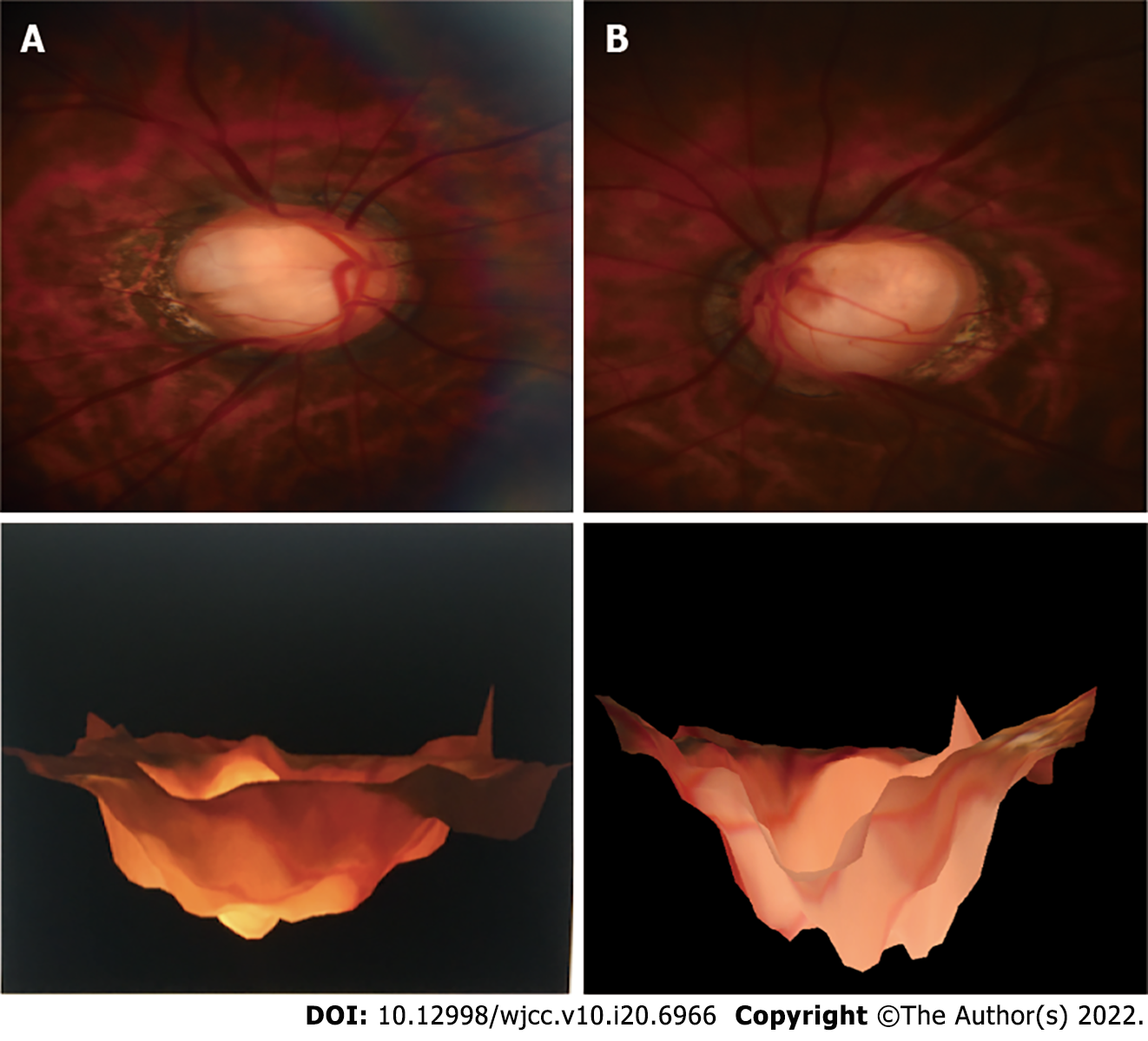
Magnetic head imaging revealed no brain abnormalities. Optic disc stereography (Kowa nonmyd WX 3D, Japan) demonstrated choroidal atrophy around the optic disc in both eyes, with optic disc coloboma is illustrated in Figure 1. Visual field examination for both eyes were performed with Humphrey Field Analyzer II (Zeiss) using 24-2 Swedish Interactive Threshold Algorithm (SITA) standard strategy. Binocular visual field examination revealed that the physiological blind spots of both eyes enlarged. Using IOL Master 700 (Zeiss), the axial length was measured as 27.72 mm and 27.42 mm for the right and left eyes, respectively. Blood flow imaging optical coherence tomography (United States Optovue, Angio-OCT) three-dimensional (3D) mode showed local defects in the temporal disc edge of the binocular optic disc. Moreover, the optic disc circular scan mode indicated that the thickness of the nerve fiber layer around the optic disc in the left eye was thinned. OCT B-scan of the left eye revealed macular serous neurosensory retinal detachment, discontinuity of the ellipsoid zone, and fracture of the outer nuclear layer of the retina. En-face OCT showed that the canal and gully-like structure formed by the defect of the optic disc nerve fiber layer between the optic disc and macula, serous detachment area, and the enlarged optic disc coloboma inferior to the temporal area were connected via the canal and gully-like structure. The fluid was considered to leak from the enlarged partial defect of the optic disc, gully-like thinning of the optic disc nerve fiber layer, and gully-like structure into the retinal layer of the macular area (Figures 2-4).
The final clinical diagnosis was optic disc coloboma in both eyes and optic disc coloboma associated with macular retinoschisis in the left eye.
On November 27, 2019, posterior scleral macular buckling of the left eye was performed under general anesthesia.
Re-examination was performed at 3 mo, 6 mo, 12 mo, and 24 mo after operation. OCT showed complete recovery of the left eye serous macular retinoschisis until 24 mo after the operation (Figure 5). The visual acuity of the left eye was gradually improved to 20/33.
Congenital optic disc coloboma includes optic disc pit, optic nerve dysplasia, and morning glory syndrome. Congenital pits of the optic disc may be present alone or occasionally combined with optic disc defects[10]. Previous case reports have described the presence of optic disc defects in the same eye combined with optic disc pit[11,12]. Optic nerve defects can occasionally be misdiagnosed as morning glory syndrome[13]. The pathophysiology of morning glory syndrome caused by abnormal fetal fissure closure is similar to that of optic disc defect[14]. However, tiny pigments can be detected with no glial hyperplasia around the optic disc in the optic disc defect, while a large amount of glial hyperplasia and pigment can be observed around papilla in the morning glory syndrome[15]. Additionally, Hotta et al[16] reported a case of choroidal and optic disc defect with a rare type of macular detachment and retinoschisis.
Serous macular retinoschisis related to optic disc coloboma is similar to that related to optic disc pit. The pathogenesis may be the result of multiple factors such as age, traction of the posterior vitreous cortex, local defects of the optic disc coloboma, and peripheral nerves of the optic disc. The drainage channel formed by the local defect of the nerve fiber layer, fluctuation of IOP, direct natural potential gap between the neuroepithelium and the pigment epithelium, and high perfusion of the choroidal capillaries (similar to the pathogenesis of the central serous chorioretinopathy) are related to the peripheral nerves of the optic disc. The secondary related factors are the canal-like channel structure formed by the local defect of the nerve fiber layer and traction of the posterior vitreous cortex and other factors. There is evidence that retinal neuroepithelial detachment in the macula becomes obvious after the age of 20 years. Liconff described that the communication between the optic disc fovea and retina resulted in a split-like separation of the inner layer of the retina[17]. Cleavage formation is the first step in the progression of serous retinal detachment related to optic disc coloboma. Krivoy et al[18] believe that the optic disc coloboma is the fluid passage between the subretinal fluid and cleavage cavity or subretinal space. SS-OCT draws a thin line in the optic disc, presumably related to the subretinal space. In an eye with an optic disc pit, the subretinal space has a direct connection with the vitreous cavity. Ohno-Matsui et al[19] reported that in 93.2% of highly myopic eyes, the subretinal space can be detected using SS-OCT. They believe that the subretinal space around the optic nerve is low reflex. In a patient with myopia, the subretinal space has a direct connection with the vitreous cavity. Previous reports have only inferred that in the optic disc pit, there is direct communication between the optic disc pit, vitreous cavity, and subretinal space. Kuhn et al[20] reported a case of an optic disc pit with silicone oil injected into the vitreous cavity. The echo of silicone oil was detected in the subretinal space, showing the communication between the subretinal space and the vitreous cavity. Additionally, the complete separation of the outer layer of the retina (full-thickness detachment of the macula) may be secondary and related to the hole in the outer layer of the macula. Some authors speculate that vitreous traction in the macula may be the cause of retinal detachment and cleavage in the macula. Therefore, vitrectomy with or without peeling the inner limiting membrane, laser photocoagulation, and intraocular gas packing can reduce or eliminate vitreous traction. A recent report found that simple vitrectomy without gas tamponade and intraocular laser can completely cure macular retinoschisis. Yokoi et al[21] used fundus photography and swept OCT images to evaluate six eyes of seven macular retinopathy patients with optic disc pit. They detected abnormal traction of the vitreous by reconstructing 3D swept OCT images and observing the vitreous at the vitreous retinal interface. This may be one of the causes of this disease. Visual acuity and OCT should be monitored through proper follow-up to observe retinal changes[22]. In our case, the most likely cause of visual impairment was the damage to the macular retinal ellipsoid zone of the left eye.
The 37-year-old patient, in this case, had no posterior detachment of the posterior vitreous cortex and had optic disc coloboma in both eyes. Further, 3D-OCT revealed more evident optic disc defects in the right eye than that in the left eye. Consequently, a serous macular retinoschisis occurred in the left eye. En-face OCT demonstrated that the canal and gully-like structure formed by local atrophy and loss of nerve fibers around the optic disc communicated with the macular retinoschisis, which might be the most fundamental cause of the disease. The pathogenesis of optic disc coloboma-related macular serous retinoschisis may be similar to optic disc pit-related macular serous retinal retinoschisis[23]. The age of onset is 30–40 years (the third decade)[24]. Posterior vitreous detachment appears gradually during this period. Another important factor may be the traction of the posterior cortex. Vitrectomy is considered the preferred and effective treatment. Even if vitrectomy is combined with optic disc edge laser, internal limiting membrane peeling and covering, gas filling, and posterior scleral macular buckling, this type of serous macular retinoschisis often results in complete recovery in 1–2 years. The success rate of different treatment methods reported in different studies is variable[25-27]. For fluids derived from the cerebrospinal fluid or vitreous liquids, which is still debatable. Both the liquids may enter the macular retinal layer. The cerebrospinal fluid enters through the defect of the lamina edge, and the vitreous humor enters through the deep coloboma of the large optic disc. The optic disc is composed of a scleral defect (the cup of the optic disc) and optic nerve fibers (the disc edge of the optic disc). Nerve fibers are tightly covered and horizontally distributed in the retinal hierarchy to prevent fluid from directly entering the retinal layers and maintain the transparent state of the retina. Local nerve fiber defects may lose this covering and protection function, allowing fluid to easily enter between the retinal layers, causing serous macular cleavage. The fovea is the lowest point of fluid outflow, similar to an hourglass or a pool floor drain. Therefore, the liquid flows from the top to the bottom. Thus, the subretinal fluid flows from the coloboma of the optic disc to the center of the macula.
Macular retinoschisis may be owing to the combined force of disc edge loss, enlarged optic disc coloboma, the canal gully-like structure formed by the defect of the nerve fiber layer around the optic disc, and the traction of the posterior vitreous cortex (Figure 6). Vitrectomy may be the preferred and effective treatment for the macular retinoschisis associated with optic disc coloboma. Proper monitoring of patients with optic disc coloboma and macular degeneration is critical. The use of optic disc stereography, and 3D, En-face, and Angio-OCT imaging during the follow-up period can clarify the correlation between macular retinoschisis and optic disc coloboma.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mohapatra SSD, India A-Editor: A S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Duvall J, Miller SL, Cheatle E, Tso MO. Histopathologic study of ocular changes in a syndrome of multiple congenital anomalies. Am J Ophthalmol. 1987;103:701-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Dutton GN. Congenital disorders of the optic nerve: excavations and hypoplasia. Eye (Lond). 2004;18:1038-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249:1113-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 136] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 4. | Brown GC, Shields JA, Goldberg RE. Congenital pits of the optic nerve head. II. Clinical studies in humans. Ophthalmology. 1980;87:51-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 183] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Brodsky MC. Congenital optic disk anomalies. Surv Ophthalmol. 1994;39:89-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 150] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Meirelles RL, Aggio FB, Costa RA, Farah ME. STRATUS optical coherence tomography in unilateral colobomatous excavation of the optic disc and secondary retinoschisis. Graefes Arch Clin Exp Ophthalmol. 2005;243:76-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Ohno-Matsui K, Hirakata A, Inoue M, Akiba M, Ishibashi T. Evaluation of congenital optic disc pits and optic disc colobomas by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54:7769-7778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Vedantham V. Double optic discs, optic disc coloboma, and pit: spectrum of hybrid disc anomalies in a single eye. Arch Ophthalmol. 2005;123:1450-1452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Özelce R, Gürlü V, Güçlü H, Özal SA. Coexistence of optic pit and coloboma of iris, lens, and choroid: a case report. Arq Bras Oftalmol. 2016;79:328-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Denis D, Girard N, Levy-Mozziconacci A, Berbis J, Matonti F. [Ocular coloboma and results of brain MRI: preliminary results]. J Fr Ophtalmol. 2013;36:210-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Steinkuller PG. The morning glory disk anomaly: case report and literature review. J Pediatr Ophthalmol Strabismus. 1980;17:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 47] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kindler P. Morning glory syndrome: unusual congenital optic disk anomaly. Am J Ophthalmol. 1970;69:376-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 164] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Lee BJ, Traboulsi EI. Update on the morning glory disc anomaly. Ophthalmic Genet. 2008;29:47-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Takkar B, Venkatesh P, Agarwal D, Kumar A. Optic disc coloboma with pit treated as glaucoma: diagnostic utility of ultrasound and swept source optical coherence tomography. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Savell J, Cook JR. Optic nerve colobomas of autosomal-dominant heredity. Arch Ophthalmol. 1976;94:395-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Hotta K, Hirakata A, Hida T. Retinoschisis associated with disc coloboma. Br J Ophthalmol. 1999;83:124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Lincoff H, Lopez R, Kreissig I, Yannuzzi L, Cox M, Burton T. Retinoschisis associated with optic nerve pits. Arch Ophthalmol. 1988;106:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Krivoy D, Gentile R, Liebmann JM, Stegman Z, Rosen R, Walsh JB, Ritch R. Imaging congenital optic disc pits and associated maculopathy using optical coherence tomography. Arch Ophthalmol. 1996;114:165-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 136] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 19. | Ohno-Matsui K, Akiba M, Moriyama M, Ishibashi T, Tokoro T, Spaide RF. Imaging retrobulbar subarachnoid space around optic nerve by swept-source optical coherence tomography in eyes with pathologic myopia. Invest Ophthalmol Vis Sci. 2011;52:9644-9650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 20. | Kuhn F, Kover F, Szabo I, Mester V. Intracranial migration of silicone oil from an eye with optic pit. Graefes Arch Clin Exp Ophthalmol. 2006;244:1360-1362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 102] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 21. | Yokoi T, Nakayama Y, Nishina S, Azuma N. Abnormal traction of the vitreous detected by swept-source optical coherence tomography is related to the maculopathy associated with optic disc pits. Graefes Arch Clin Exp Ophthalmol. 2016;254:675-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Snead MP, James N, Jacobs PM. Vitrectomy, argon laser, and gas tamponade for serous retinal detachment associated with an optic disc pit: a case report. Br J Ophthalmol. 1991;75:381-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Hirakata A, Inoue M, Hiraoka T, McCuen BW 2nd. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012;119:810-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 24. | Ferry AP. Macular detachment associated with congenital pit of the optic nerve head. pathologic findings in two cases simulating malignant melanoma of the choroid. Arch Ophthalmol. 1963;70:346-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 101] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Besada E, Barr R, Schatz S, Brewer C. Vitreal pathogenic role in optic pit foveolar retinoschisis and central serous retinopathy. Clin Exp Optom. 2003;86:390-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Irvine AR, Crawford JB, Sullivan JH. The pathogenesis of retinal detachment with morning glory disc and optic pit. Trans Am Ophthalmol Soc. 1986;84:280-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 71] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Schatz H, McDonald HR. Treatment of sensory retinal detachment associated with optic nerve pit or coloboma. Ophthalmology. 1988;95:178-186. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 1.8] [Reference Citation Analysis (0)] |