Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.691
Peer-review started: July 3, 2021
First decision: September 28, 2021
Revised: October 9, 2021
Accepted: December 2, 2021
Article in press: December 2, 2021
Published online: January 14, 2022
Processing time: 192 Days and 17.8 Hours
The role of occlusal factors on the occurrence of temporomandibular joint disorders (TMDs) is still unclear and it is tricky for orthodontists to treat malocclusions in patients with TMDs. We report the case of the second orthodontic treatment of an adult female with Class II division 2 malocclusion associated with TMD. With the removal of anterior occlusal interference, TMD symptoms were alleviated and cone beam computed tomography (CBCT) images showed the bilateral condyles shifted forward.
This case report presented an orthodontic retreatment of an adult female with TMD and mandibular backward positioning based on CBCT examination and Joint Space Index (JSI) analysis. The left and right JSI values of -38.5 and -52.6 indicated that the position of bilateral condyles had posterior displacement. Ten years prior to this evaluation, she underwent orthodontic treatment resulting in the extraction of two upper premolars and one lower central incisor. The joint symptoms, including pain and sounds, were alleviated along with verified mandibular forward repositioning by extraction of another lower central incisor.
Mandibular backward positioning could be associated with TMD. JSI analysis based on CBCT is a convenient way to examine condylar positions quantitatively.
Core Tip: Class II division 2 malocclusion is considered to be a risk factor for temporomandibular joint disorders (TMDs). In this case of the second orthodontic treatment of an adult female with Class II division 2 malocclusion associated with TMD, we measured the joint space to assess the condylar position and found that the bilateral condyles were located in the posterior position. We suspected that this patient’s TMD was a manifestation of mandibular backward positioning. Temporomandibular joint symptoms were alleviated with the removal of anterior occlusal interference, and the posttreatment cone beam computed tomography images showed that bilateral condyles shifted forward after orthodontic treatment.
- Citation: Yu LY, Xia K, Sun WT, Huang XQ, Chi JY, Wang LJ, Zhao ZH, Liu J. Orthodontic retreatment of an adult woman with mandibular backward positioning and temporomandibular joint disorder: A case report. World J Clin Cases 2022; 10(2): 691-702
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/691.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.691
Temporomandibular joint disorders (TMDs) are common public health problems and affect approximately 60% to 70% of people worldwide, according to statistics in different countries[1]. The clinical symptoms of TMDs include pain, joint sounds, and functional limitations, such as restricted mandibular movement and limited mouth opening[2]. Pain-related disorders can affect a patient’s social interactions, psychological health, and quality of life. Epidemiological researchers found that the prevalence of TMDs was associated with age, sex, occlusion, and orthodontic treatment[3,4]. However, the exact causes of TMDs are still largely unknown, and it is often difficult to find an obvious cause. Moreover, the role of occlusal factors in the occurrence of TMDs has remained controversial until recently[5]. Therefore, the treatment of malocclusion with TMDs is a complex problem for orthodontists.
Functional malocclusion was reported to cause displacement of the condyle in the glenoid fossa[6] and might result in functional disorders of the temporomandibular joint (TMJ)[7]. Condylar displacement could be a sign of functional deviation, which was analyzed by cone beam computed tomography (CBCT) and Joint Space Index (JSI) analyses in the treatment of mandibular shift in an adult woman[8]. As another example, Class II division 2 patients have salient features, including deep bites, retroclined upper incisors, and mandibular retrognathism[9]. It was reported that mandibular retrognathism in Class II division 2 patients would have a risk of articular disk displacement[10]. Nevertheless, there are few scientific reports about the pathology and treatment of functional malocclusion.
In this case, we reported orthodontic retreatment of an adult female with TMD and mandibular backward positioning based on CBCT examination and JSI analysis. The joint symptoms, including pain and sounds, were alleviated along with verified mandibular forward repositioning. Mandibular backward positioning could be related to TMD. Moreover, JSI analysis is a convenient way to examine condyle positions quantitatively.
An adult woman aged 26 years visited the clinic to request orthodontic retreatment for her relapsed crowding in her mandibular dentition.
Ten years prior to the present visit to the clinic, she received orthodontic treatment resulting in the extraction of two upper premolars and one lower central incisor.
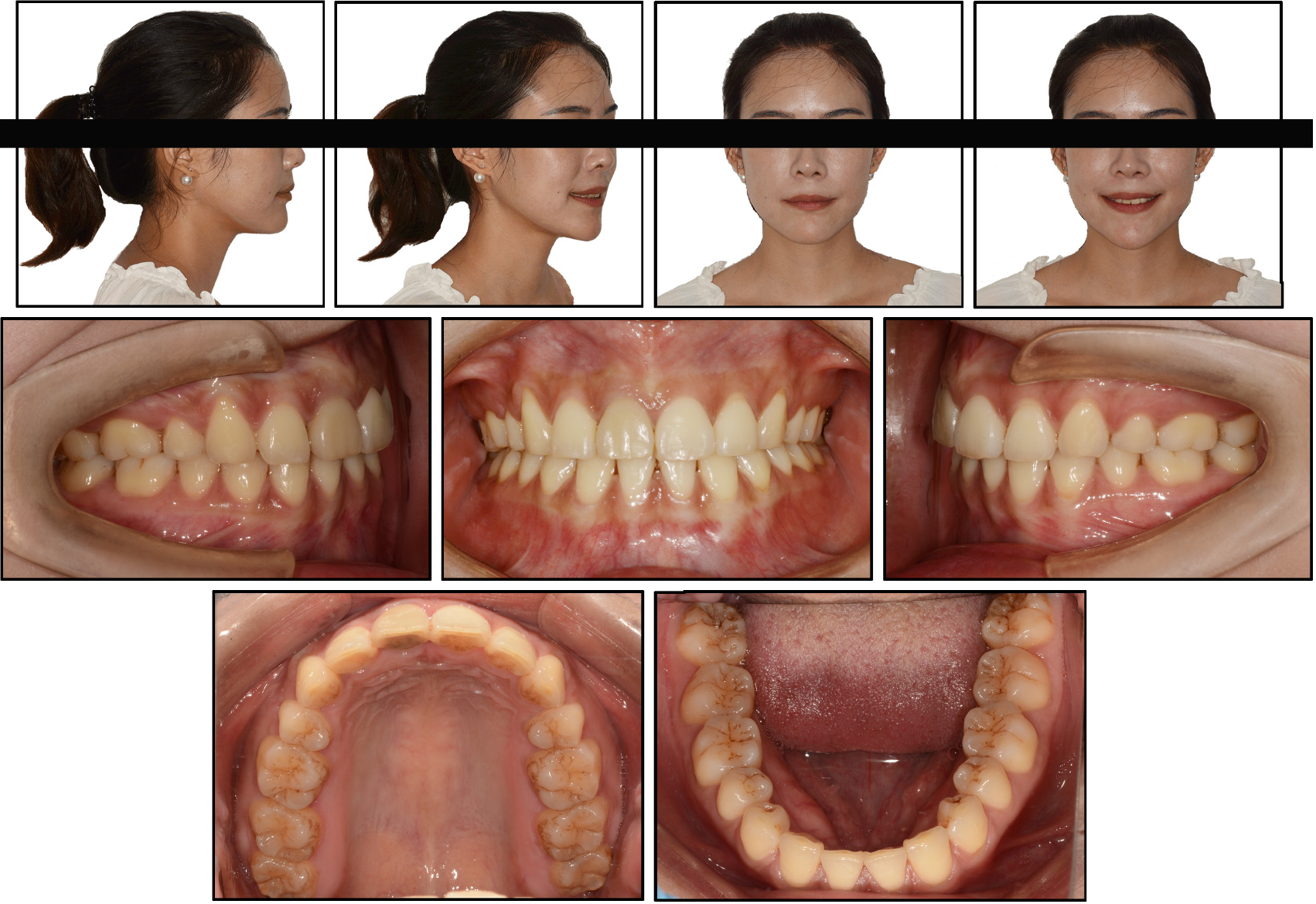
The clinical examination revealed that the patient had a straight profile and a strong chin (Figure 1). A 2.0 mm space in the maxillary dentition and 4.0 mm of crowding in the mandibular dentition were found. The upper incisors were retroclined, and the anterior overjet was minimal. The anterior overbite was within the normal range. Compared with the facial midline, the maxillary dental midline deviated by 0.5 mm to the right. The mandibular dental midline was basically the center of the remaining lower central incisor since the other lower central incisor was missing. No chin deviation was found. She had Class II molar and canine relationships bilaterally.
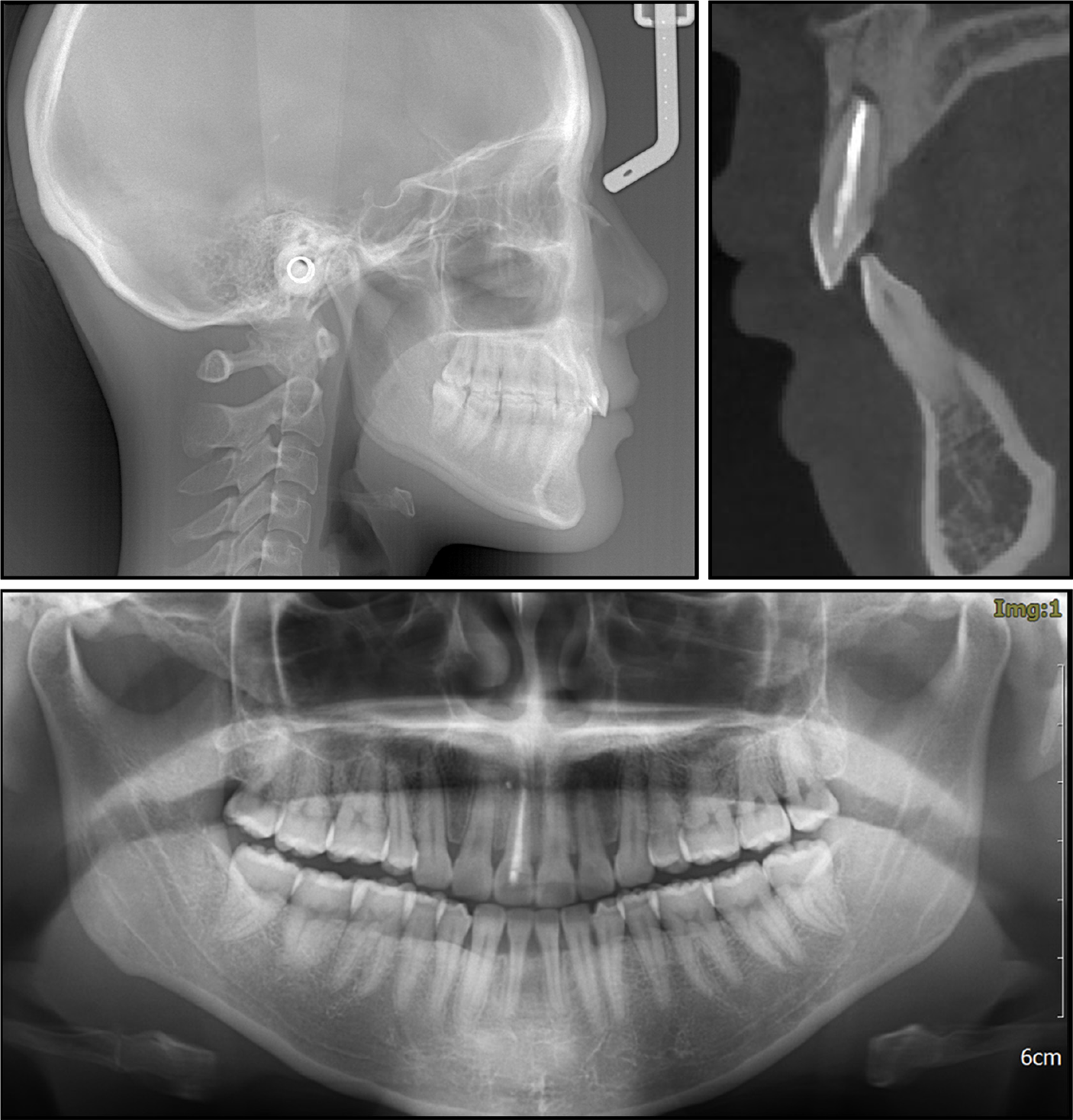
Cephalometric analysis (Figure 2 and Table 1) indicated skeletal Class I malocclusion (SNA, 82.4°; SNB, 79.5°; ANB, 2.9°) with a normal mandibular plane angle (SN-MP, 34.8°). The maxillary incisors were retroclined (U1-SN, 82.8°; U1-NA, 15.8°).
| Measurement | Normal | Pretreatment | Posttreatment |
| SNA° | 81.7 ± 2.5 | 82.4 | 82.2 |
| SNB° | 78.9 ± 2.2 | 79.5 | 79.9 |
| ANB° | 2.8 ± 1.2 | 2.9 | 2.3 |
| SN-MP° | 32.9 ± 4.2 | 34.8 | 34.2 |
| U1-L1° | 123.2 ± 6.2 | 136.8 | 129.2 |
| U1-SN° | 105.1 ± 6.2 | 82.8 | 101.3 |
| U1-NA° | 23.3 ± 6.2 | 15.8 | 17.6 |
| L1-NB° | 27.4 ± 4.7 | 28.1 | 26.0 |
| IMPA (L1-MP)° | 95.4 ± 4.7 | 93.0 | 91.5 |
| UL-EP (mm) | -0.5 ± 1.9 | -2.5 | -1.7 |
| LL-EP (mm) | 1.3 ± 1.9 | -2.2 | -1.1 |
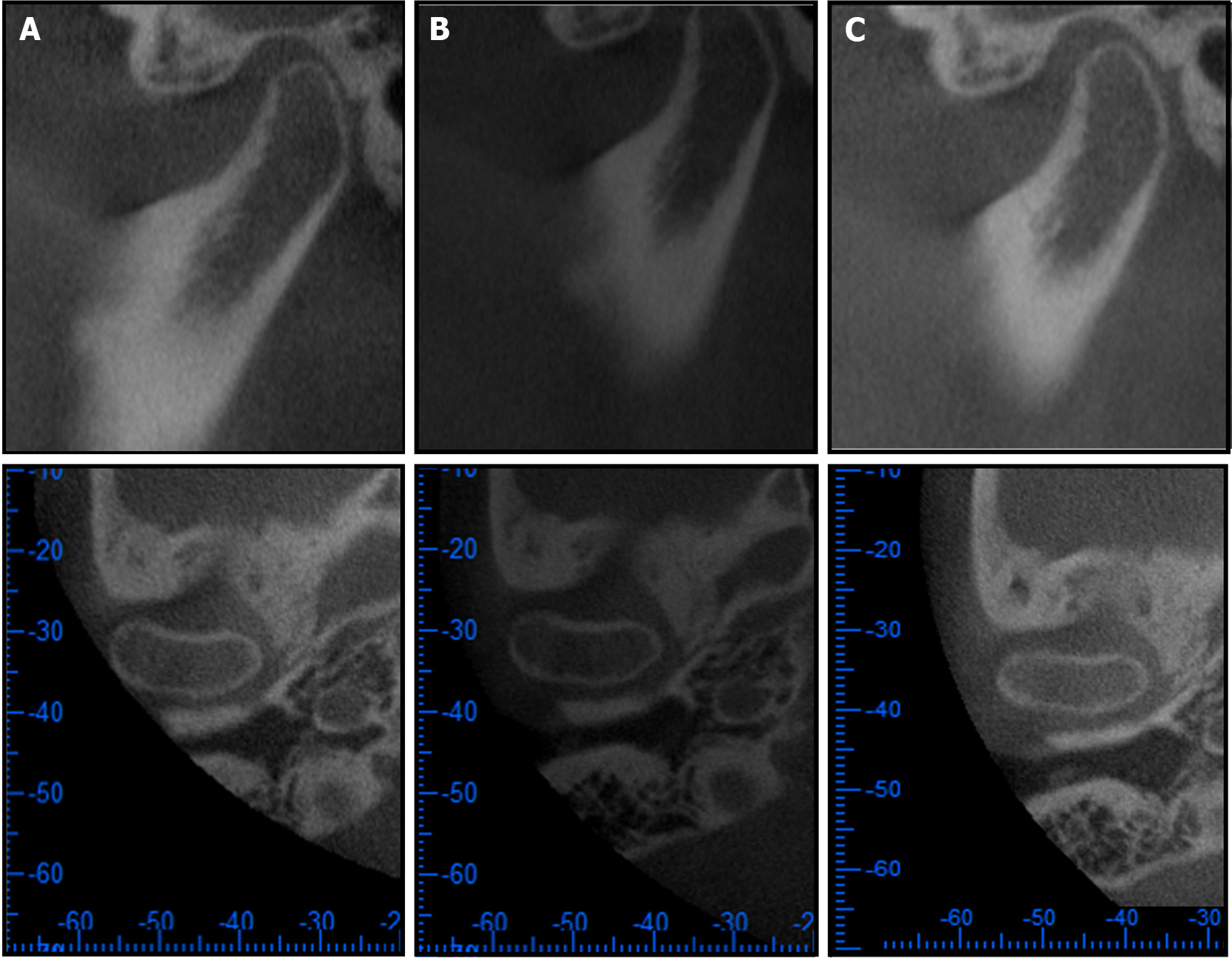
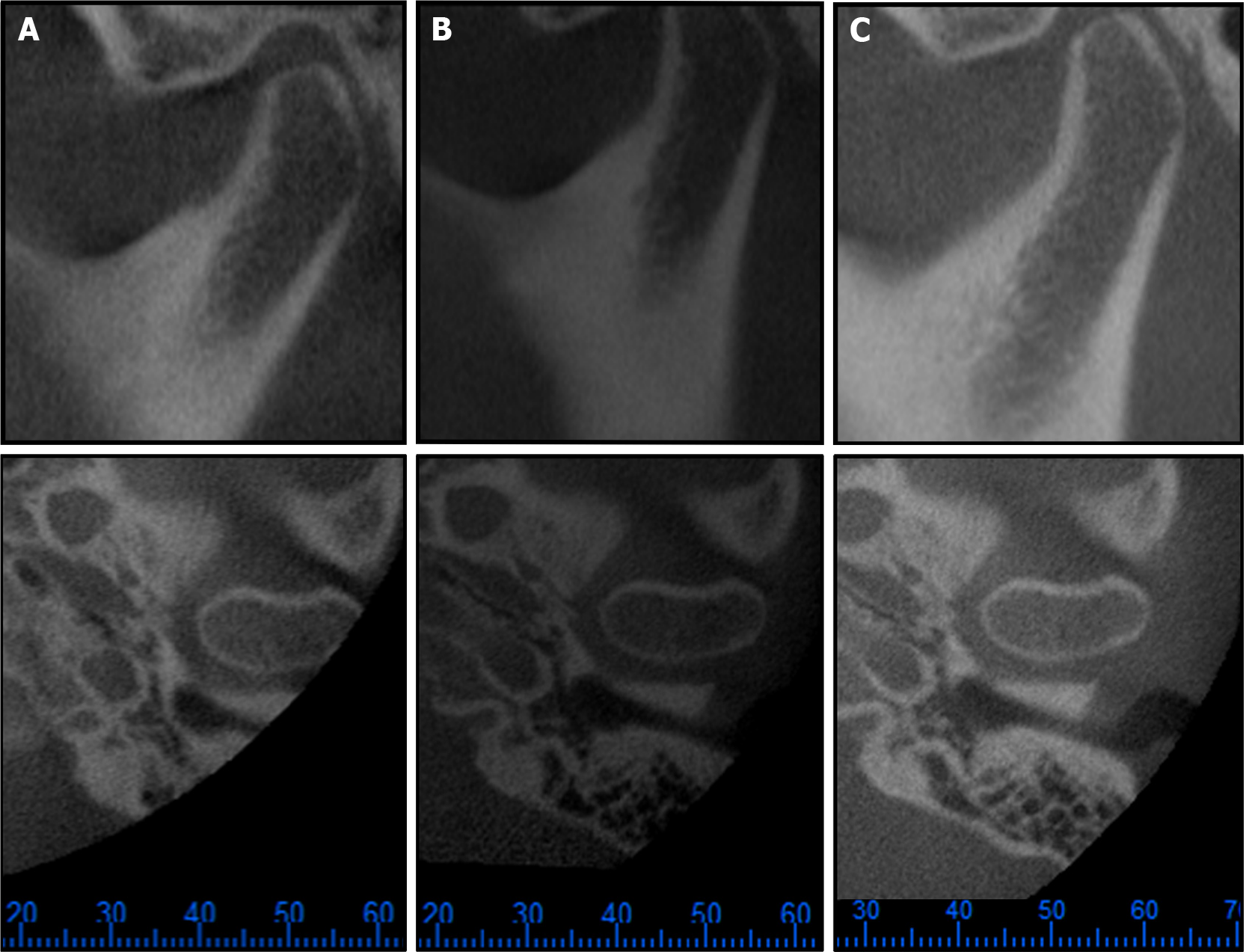
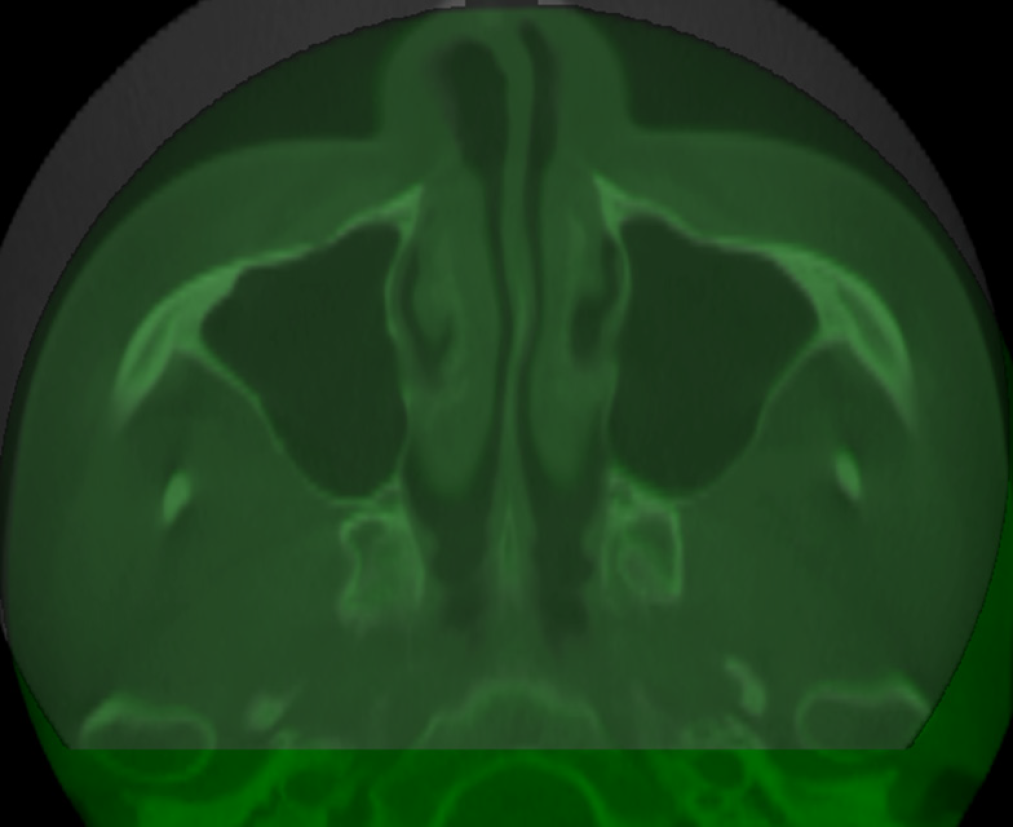
The patient had experienced TMJ pain many times after her first orthodontic treatment, and we found joint clicking at the start of mouth opening in TMJ clinical examination. CBCT examination was performed to check the TMJs. CBCT examination was performed when the maxillary and mandibular teeth were in maximum intercuspation (MI). JSI was used to assess the condylar position by calculating the ratio of the anterior and posterior joint spaces[11]. Vargas-Pereira [12] described that the physiologic range of JSI values for the condylar position was -32.5 to 21.1. A greater value indicated an anterior position, while a smaller value indicated a posterior position. CBCT images of the TMJs were oriented sagittally and taken perpendicular to the maximum transverse of the long axis of the condylar region, as previously reported[13]. Left and right JSI values of -38.5 and -52.6 (Table 2), respectively, were obtained in this case. The results indicated that the position of bilateral condyles had posterior displacement and that the right condyle displacement was more severe than that of the left condyle. The right upper central incisor had dark gray discoloration, but the panorama examination showed no obvious findings. CBCT examination revealed a large periapical radiolucency associated with the upper right central incisor (Figure 2). We collected the medical history and the patient gave no history of trauma, caries, and clinical symptoms of upper right central incisor. We speculated that the periapical periodontitis of the upper right central incisor might be associated with anterior occlusal interference.
| Right temporomandibular joint | Left temporomandibular joint | |||||
| Anterior JS (mm) | Posterior JS (mm) | JSI | Anterior JS (mm) | Posterior JS (mm) | JSI | |
| Pretreatment | 3.57 | 1.11 | -52.6 | 2.75 | 1.22 | -38.5 |
| Retention for 22 mo | 3.28 | 1.30 | -43.2 | - | - | - |
| Relative change (re-pre) | -0.29 | 0.19 | 9.4 | - | - | - |
The final diagnoses of the presented case were Class II malocclusion and TMD.
In accordance with the pretreatment records and the patient's chief complaint, the treatment objectives were to: (1) Advise the endodontist to treat periapical periodontitis of the upper right central incisor; (2) Align the dental arch, eliminate dental crowding, and close the space; (3) Achieve ideal overjet and overbite as well as coincident dental and facial midlines; and (4) Prevent the aggravation of TMD and hopefully alleviate the TMD symptoms.
One possible option was nonextraction treatment. Three teeth were removed during the first orthodontic treatment, and only slight crowding relapse occurred in the anterior mandibular dentition. Too much space might be created if more teeth were extracted. Interproximal enamel reduction (IPR) was recommended in mild crowding[14]. Therefore, the lower anterior teeth might be grinded for the mandibular dentition alignment. However, there were some disadvantages. First, IPR was reported to have risks of tooth sensitivity and caries[14]. In addition, the overjet would still be minimal after the space in the upper dentition was closed and the lower dentition was aligned. It was also difficult to correct the Class II occlusion relationship without tooth extraction.
Class II elastics are widely used for Class II malocclusion treatment; these elastics are conducive to correcting deep anterior overbite, closing the extraction space, and guiding the mandible forward. However, caution should be taken when treating hyperdivergent patients and those exhibiting progressive absorption of the condyle. In this case, the patient had a normal mandibular plane angle and posterior displacement of the condyles but no joint absorption. Class II elastics could guide the mandible forward to obtain a Class I occlusion relationship and change the position of the condyle, which might ease TMJ symptoms. However, when using Class II elastic traction, a larger overjet is required to prevent occlusal trauma in anterior teeth. Therefore, Class II elastics could not be used with the above treatment option.
The other treatment option was to extract one lower central incisor. Since two upper premolars and one lower central incisor were extracted in the first orthodontic treatment, the removal of another lower central incisor was beneficial to establish a coordinated and symmetrical dental arch. However, after aligning and closing the space in the upper and lower dentition, it was not clear if the anterior overjet would be too large. There was an advantage to using Class II elastics to correct molar relationships in this option while guiding the mandible forward to change the position of the condyle and establish an ideal anterior overjet. Based on the consideration of the treatment objectives, this option was chosen for this case.
Before orthodontic treatment, the patient received endodontic therapy, and the periapical periodontitis of the upper right central incisor was controlled. After extraction of the mandibular central incisor, the 0.022 × 0.028-inch slot preadjusted edgewise brackets were then bonded onto the entire dentition except for the second molars and the third molars. The archwire sequence progressed from 0.014-inch nickel-titanium wire to 0.018 × 0.025-inch stainless steel working wire. Seventeen months into treatment, all teeth were leveled and aligned, and space closure was completed. Although the use of Class II elastics had been planned, the occlusal relationship was corrected once an adequate anterior overjet was established, and Class II elastics were not actually applied. CBCT examination was performed to assess the recovery of 11 and changes in condylar positions. The total treatment time was 17 mo. A Hawley retainer was used for retention.
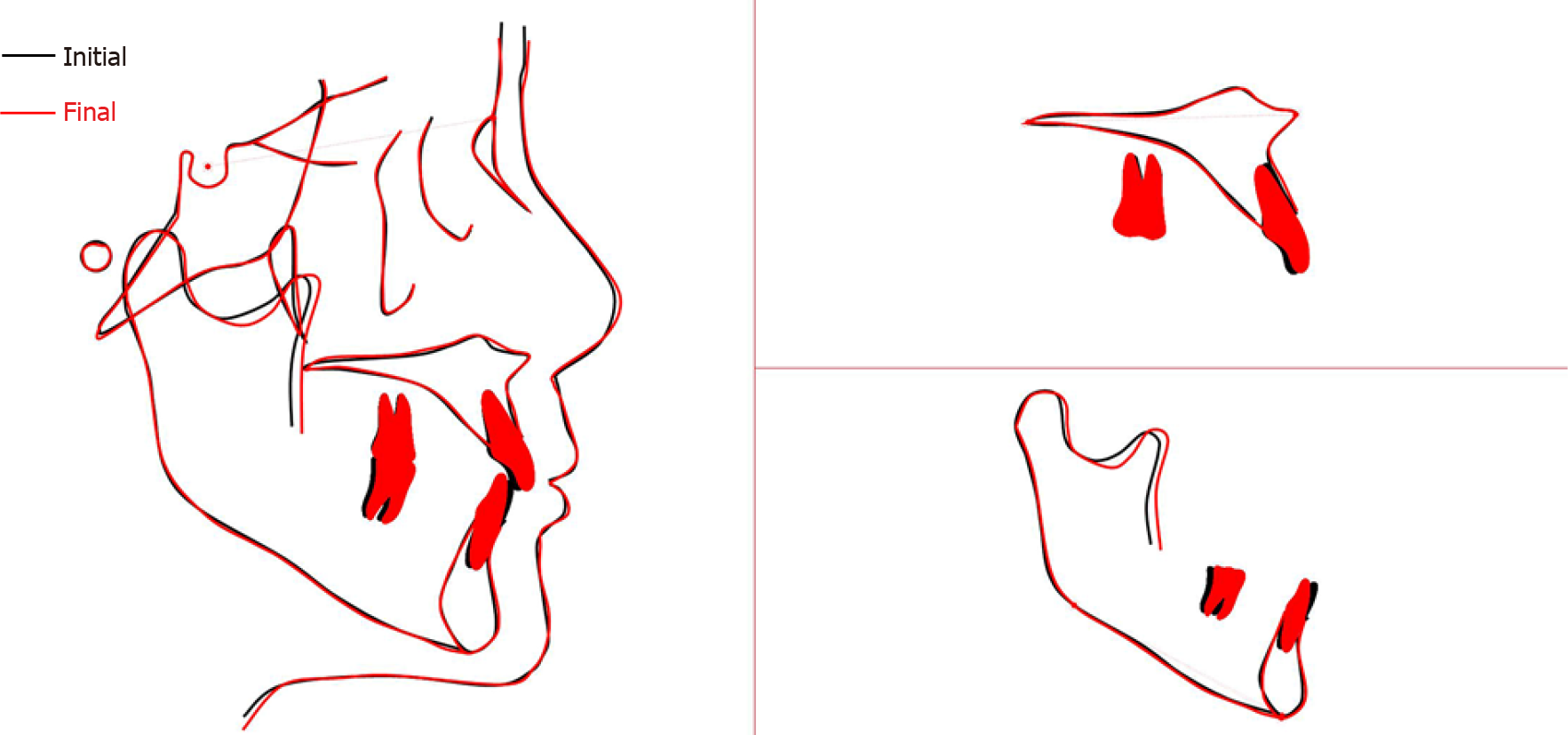
The posttreatment photographs showed a Class I canine and molar relationship, normal overbite and overjet, improved midline deviation, and neatly aligned teeth (Figure 3). The posttreatment panoramic radiograph showed no significant root resorption and good root parallelism (Figure 4). CBCT examination of 11 indicated the healing of periapical radiolucent lesions around the root of the upper right central incisor (Figure 4). The posttreatment cephalometric analysis is shown in Table 1. Superimposition of the pretreatment and posttreatment cephalometric radiographs showed mild retraction of the mandibular incisors and proclination of the upper incisors (Figure 5). The CBCT images of the TMJs in the aforementioned section showed the condyles shifted forward after orthodontic treatment (Figure 6 and Figure 7). The right JSI after 22 mo of retention was -43.2 and was larger than that observed at pretreatment (-52.6), which confirmed the condylar shifted forward (Table 2). Although the CBCT image showed an incompetent left condylar after 22 mo of retention, we inferred a larger JSI of the left condylar. CBCT superimposition of the pretreatment and retention bilateral TMJs also validated the same results (Figure 8). Joint clicking disappeared, and TMJ pain was relieved. After 22 mo of retention, the patient visited the clinic for tooth bleaching of the upper right central incisor. Facial and intraoral photographs showed a stable occlusion (Figure 9), and CBCT images showed the TMJ in a stable position without recurrence of TMJ pain and sound (Figures 6 and 7).
Functional or occlusal factors are considered a potential etiology of TMDs. It has been proposed that the presence of occlusal interferences usually results in TMJ functional disorders. Previous studies reported that occlusal interference could cause mandibular deviation, leading to changes in the condylar position and pain in the TMJ[15]. Hidaka et al[6] also commented that functional malocclusion from malocclusions or ortho
Many scholars, such as Roth[18], advocated for functional occlusion as the goal of orthodontic treatment. The authors believed that more attention should be given to achieving centric relation and MI harmony without occlusal interference after orthodontic treatment. Articulator mountings, including a Panadent condylar position indicator and mandibular position indicator[19], were designed to transfer the occlusal status and the condylar position to the outside of the mouth. The traditional method is to diagnose occlusal interference and premature contact and to detect functional displacement of the condyle. However, it was reported that this method could not accurately quantify small changes in joint position[20,21].
Imaging examination is an essential method for the diagnosis and treatment of TMDs. Various imaging examinations can be used to detect the TMJ, such as panoramic radiography, magnetic resonance imaging (MRI) and CBCT. The latter two methods can be used for quantitative analysis. MRI has excellent sensitivity in nonmineralized tissue and is widely used to evaluate cartilage and disc position and to diagnose TMD[22]. Although the quality of MRI has improved, there are still limitations in the low-quality images of the complex bone structure of the TMJ that it provides[23]. In addition, MRI evaluation was not easily accepted by patients due to high costs; also, stomatological hospitals are rarely equipped with MRI equipment. Maxillofacial CBCT is specially designed for the maxillofacial tissue. Maxillofacial CBCT was developed from conventional CT and is specially designed for maxillofacial tissues with low cost and a low radiological dose[24]. CBCT is an intuitive, simple and accurate method for comprehensive evaluation of hard tissue, diagnosis of condylar changes, and a clear display of joint space in three dimensions[25].
Mandibular retrognathism is usually associated with Class II division 2, and such patients are more susceptible to TMDs[9]. It was reported that adults with Class II malocclusion might experience muscle pain[26], and another study found that mandibular retrognathism in Class II division 2 patients increased the risk of articular disk displacement[10]. In this case, the patient extracted two upper premolars and one lower central incisor in the first orthodontic treatment, resulting in a minimal overjet to restrict mandibular movement and Class II division 2 malocclusion. We preliminarily estimated TMD risk based on medical history and TMJ clinical examination. CBCT was performed to evaluate the condyle position. Many researchers, such as Mavreas[27] and Ruf[13,28], recommended the use of the JSI to evaluate anterior and posterior joint spaces and condylar positions. Vargas-Pereira[12] calc ulated the physiologic range of the JSI (-32.5, 21.1), indicating positive anterior displacement and a negative posterior displacement[11]. We used the JSI to examine joint space in CBCT images and found that the bilateral condyles were located in the posterior position. Combined with the medical history, TMJ clinical examination, intraoral occlusion, and CBCT images, we suspected that the minimal overjet in the first orthodontic limited mandibular movement, led to backward positioning of the mandible, and caused TMJ symptoms. Therefore, the patient's TMD might be a consequence of functional mandibular retraction. In the second orthodontic treatment, with the proclination of upper anterior teeth and retraction of lower anterior teeth to construct an ideal overjet, joint symptoms were alleviated without using Class II elastic traction. Comparing the CBCT images of the TMJ before and after the second treatment, it was found that bilateral condyles shifted forward, which further suggested that occlusal factors might be closely associated with the patient's TMD. After 22 mo of retention, the condylar position was stable, and there was no recurrence of TMD.
The patient's TMD could be due to iatrogenic functional or occlusal factors during the first orthodontic treatment. Although the relationship between orthodontics and TMDs has been controversial, several studies have reported that incorrect orthodontic treatment results in iatrogenic TMDs. For example, it was reported that excessive retraction and retroclination of upper incisors could cause premature contacts and lead to distal displacement of the mandible and mandibular condyle. As a result, mandible retraction increases the risk of TMDs[29]. Therefore, more attention should be given to joint changes in orthodontic treatment.
In conclusion, mandibular backward positioning could be correlated with TMD and TMD symptoms might be alleviated with the mandibular forward repositioning for this situation. JSI analysis based on CBCT is convenient to evaluate condylar positions quantitatively.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kaku M, Panda M, Srivastava D S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Dantas CMG, Vivan CL, de Fantini SM, de Freitas Costa E Silva PM, Pannuti CM, Witzel AL, Dominguez GC. The influence of educational measures and low-level laser phototherapy on temporomandibular disorders: Study protocol clinical trial (SPIRIT Compliant). Medicine (Baltimore). 2020;99:e19005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, Ettlin D, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Jensen R, John MT, De Laat A, de Leeuw R, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF; International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group†. J Oral Facial Pain Headache. 2014;28:6-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1621] [Cited by in RCA: 2554] [Article Influence: 232.2] [Reference Citation Analysis (0)] |
| 3. | Agerberg G, Carlsson GE. Functional disorders of the masticatory system. I. Distribution of symptoms according to age and sex as judged from investigation by questionnaire. Acta Odontol Scand. 1972;30:597-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 216] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Poveda Roda R, Bagan JV, Díaz Fernández JM, Hernández Bazán S, Jiménez Soriano Y. Review of temporomandibular joint pathology. Part I: classification, epidemiology and risk factors. Med Oral Patol Oral Cir Bucal. 2007;12:E292-E298. [PubMed] |
| 5. | Stone JC, Hannah A, Nagar N. Dental occlusion and temporomandibular disorders. Evid Based Dent. 2017;18:86-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Hidaka O, Adachi S, Takada K. The difference in condylar position between centric relation and centric occlusion in pretreatment Japanese orthodontic patients. Angle Orthod. 2002;72:295-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Chen Q, Mai ZH, Lu HF, Chen L, Chen Z, Ai H. Treatment of a mandibular functional shift in an adolescent boy with temporomandibular disorder and crossbites. Am J Orthod Dentofacial Orthop. 2015;148:660-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Xia K, Sun W, Yu L, Huang X, Zhao Z, Liu J. Treatment of the mandibular shift in an adult woman and the diagnostic value of joint space index: a case report. Eur J Med Res. 2020;25:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Prasad SE, Indukuri RR, Singh R, Nooney A, Palagiri FB, Narayana V. Pathognomonic features of Angle's Class II division 2 malocclusion: A comparative cephalometric and arch width study. J Int Soc Prev Community Dent. 2014;4:S105-S109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Zuaiter S, Robin O, Gebeile-Chauty S, Raberin M. [Does dental class II division 2 predispose to temporomandibular disorders? Orthod Fr. 2013;84:277-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Chavan SJ, Bhad WA, Doshi UH. Comparison of temporomandibular joint changes in Twin Block and Bionator appliance therapy: a magnetic resonance imaging study. Prog Orthod. 2014;15:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Vargas-Pereira M. Quantitative Auswertungen bildgebender Verfahren und Entwicklung einer neuen metrischen Analyse für Kiefergelenkstrukturen im Magnetresonanztomogramm. PhD thesis, Uni Kiel. 1997. Available from: https://www.bibsonomy.org/bibtex/41b0fccf60ee6d70a50a809430557f1b. |
| 13. | Ruf S, Pancherz H. Temporomandibular joint growth adaptation in Herbst treatment: a prospective magnetic resonance imaging and cephalometric roentgenographic study. Eur J Orthod. 1998;20:375-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 93] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Lapenaite E, Lopatiene K. Interproximal enamel reduction as a part of orthodontic treatment. Stomatologija. 2014;16:19-24. [PubMed] |
| 15. | Egermark-Eriksson I, Carlsson GE, Magnusson T. A long-term epidemiologic study of the relationship between occlusal factors and mandibular dysfunction in children and adolescents. J Dent Res. 1987;66:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 115] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Koide D, Yamada K, Yamaguchi A, Kageyama T, Taguchi A. Morphological changes in the temporomandibular joint after orthodontic treatment for Angle Class II malocclusion. Cranio. 2018;36:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Roth RH. Temporomandibular pain-dysfunction and occlusal relationships. Angle Orthod. 1973;43:136-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Roth RH. Functional occlusion for the orthodontist. J Clin Orthod. 1981;15:32-40, 44. [PubMed] |
| 19. | Crawford SD. Condylar axis position, as determined by the occlusion and measured by the CPI instrument, and signs and symptoms of temporomandibular dysfunction. Angle Orthod. 1999;69:103-15; discussion 115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Kandasamy S, Boeddinghaus R, Kruger E. Condylar position assessed by magnetic resonance imaging after various bite position registrations. Am J Orthod Dentofacial Orthop. 2013;144:512-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 21. | Rinchuse DJ, Kandasamy S. Centric relation: A historical and contemporary orthodontic perspective. J Am Dent Assoc. 2006;137:494-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Walker TF, Broadwell BK, Noujeim ME. MRI assessment of temporomandibular disc position among various mandibular positions: a pilot study. Cranio. 2017;35:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Al-Saleh MA, Alsufyani NA, Saltaji H, Jaremko JL, Major PW. MRI and CBCT image registration of temporomandibular joint: a systematic review. J Otolaryngol Head Neck Surg. 2016;45:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Larheim TA, Abrahamsson AK, Kristensen M, Arvidsson LZ. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44:20140235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 157] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 25. | Hilgers ML, Scarfe WC, Scheetz JP, Farman AG. Accuracy of linear temporomandibular joint measurements with cone beam computed tomography and digital cephalometric radiography. Am J Orthod Dentofacial Orthop. 2005;128:803-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 213] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 26. | Mohlin B, Ingervall B, Thilander B. Relation between malocclusion and mandibular dysfunction in Swedish men. Eur J Orthod. 1980;2:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 70] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 27. | Mavreas D, Athanasiou AE. Tomographic assessment of alterations of the temporomandibular joint after orthognathic surgery. Eur J Orthod. 1992;14:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Ruf S, Pancherz H. Does bite-jumping damage the TMJ? Angle Orthod. 2000;70:183-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | McLaughlin RP, Bennett JC. The extraction-nonextraction dilemma as it relates to TMD. Angle Orthod. 1995;65:175-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |