Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.685
Peer-review started: July 4, 2021
First decision: October 18, 2021
Revised: October 22, 2021
Accepted: December 7, 2021
Article in press: December 7, 2021
Published online: January 14, 2022
Processing time: 191 Days and 14.5 Hours
Synovial chondromatosis (SC) is a rare benign lesion first reported by Ambrose Pare in 1558. It is most common in the knee joint, followed by the hip joint and elbow joint. It is characterized by the presence of multiple pearl-like osteo
We report a 6-year-old Chinese boy who presented to our hospital with left hip joint pain and claudication for more than one year. We performed total surgical resection of SC tissue in the left hip. A good prognosis was confirmed at the 6-wk follow-up. Pain and swelling symptoms were totally relieved, range of motion of his left hip returned to normal, and there was no clinical evidence of lesion recurrence at last follow-up. Our case is the youngest reported patient with SC occurring in the hip.
SC is a rare disease and can be easily misdiagnosed. When we encounter children with hip pain and claudication, increased vigilance and a comprehensive physical examination and imaging examination should be considered, in order to avoid misdiagnosis and delayed treatment in patients.
Core Tip: Synovial chondromatosis (SC) is a rare disease and can be easily misdiagnosed. We report a 6-year-old Chinese boy who received total surgical debridement of the left hip lesion. A good prognosis was confirmed at the 6-wk follow-up. Pain and swelling symptoms were totally relieved, range of motion of the left hip returned to normal, and there was no clinical evidence of lesion recurrence at last follow-up. Our case is the youngest reported patient with SC occurring in the hip.
- Citation: Yi RB, Gong HL, Arthur DT, Wen J, Xiao S, Tang ZW, Xiang F, Wang KJ, Song ZQ. Synovial chondromatosis of the hip joint in a 6 year-old child: A case report. World J Clin Cases 2022; 10(2): 685-690
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/685.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.685
Pain accompanied by claudication is a common complaint of hip joint disease in children. Routine imaging examination is often nonspecific. Early and correct diagnosis has a marked influence on the prognosis and function of the hip joint in children.
Synovial chondromatosis (SC) is a benign tumor secondary to synovial chondroma. It occurs mostly in men aged 30-50 years and is very rare in children. SC can be classified into primary and secondary SC. Primary SC occurs with no history of osteoarticular diseases, while secondary SC occurs in the presence of pathological changes, such as osteoarthritis, rheumatoid arthritis, and bone degeneration[1]. SC frequently involves a single joint. The knee joint is the most commonly affected joint, followed by the hip joint, elbow joint, shoulder joint, and ankle joint; 33 areas have been reported to be involved[2]. The most common symptoms of SC are joint pain, swelling, and limited motion. Diagnosis is mainly based on imaging; Seventy percent of patients with SC have calcified nodules on X-ray and computed tomography (CT) examinations, while some patients may not have obvious calcification and nodules in the early stage.
A 6-year-old child with hip pain and claudication was admitted to our hospital. X-ray of the hip in this child was nonspecific. Combined with physical and magnetic resonance examinations, the patient was diagnosed with synoviochondroma of the left hip joint. SC was confirmed by surgery and pathologic examination.
A 6-year-old male patient was admitted to hospital due to left hip joint pain and claudication.
He was admitted to the hospital due to left hip joint pain and claudication for more than 1 year. He was diagnosed with left hip joint synovitis in other hospitals. He was advised to rest in bed, but his symptoms did not significantly improve. Later, he was diagnosed with left femoral head avascular necrosis and underwent external fixation with bracing. His symptoms did not significantly improve, and the pain and claudication were aggravated.
Past medical history was negative.
Personal and family history, medication history, social history, and allergic history were negative.
No obvious swelling of the left hip joint was observed, with asymmetric groin lines, low skin temperature, local tenderness, pelvis tilting to the left, and unequal length of lower limbs of about 1.5 cm. The left hip joint internal rotation, external rotation, and flexion were limited, with left Allis sign (+), Thomas sign (+), and 4-character sign (+).
Laboratory examinations were within normal ranges, including erythrocyte sedimentation rate, white blood cell count, and levels of C-reactive protein, rheu
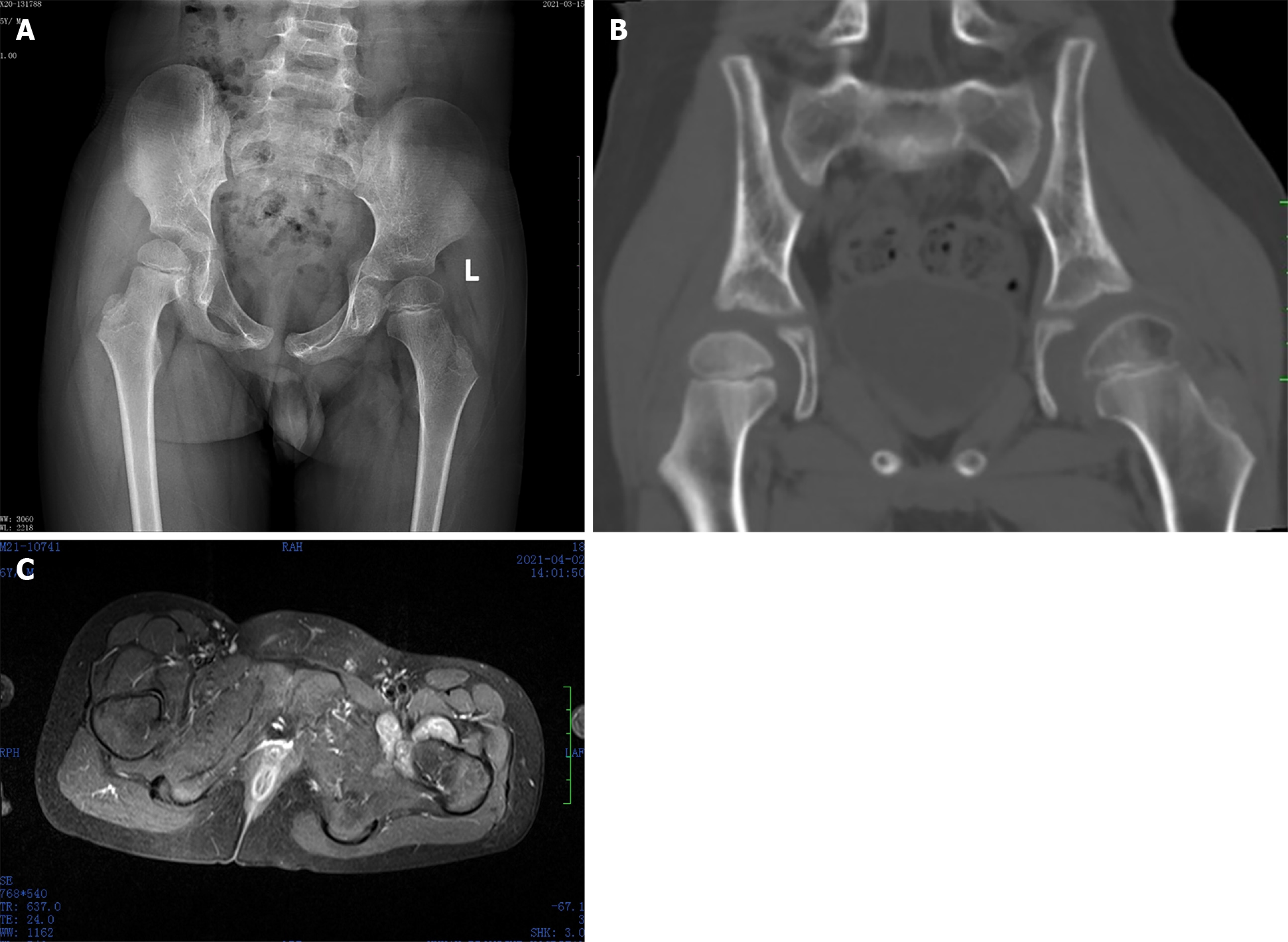
B-ultrasound showed left hip joint effusion. X-ray showed slight flattening of the left femoral head (Figure 1A). CT showed a decrease in the density of the left hip joint epiphysis and widening of the left hip joint space (Figure 1B). Magnetic resonance imaging (MRI) showed synovial thickening of the left hip joint (Figure 1C).
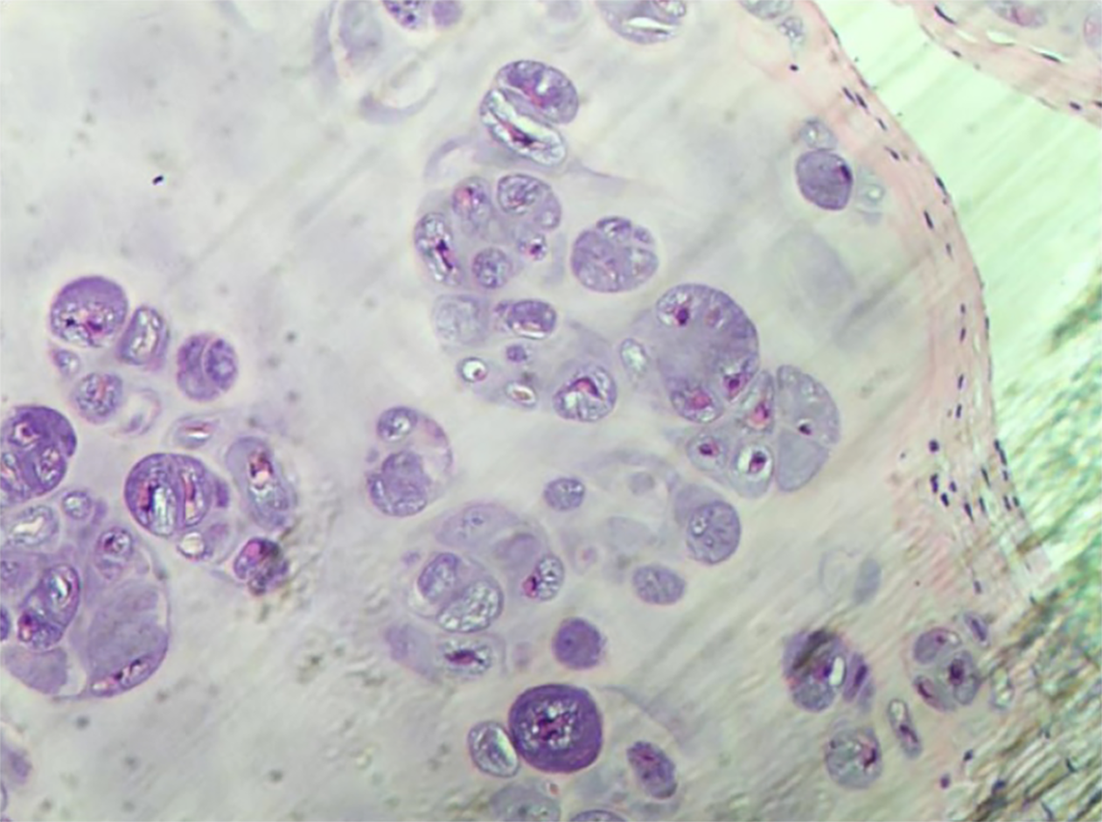
Biopsy confirmed SC (Figure 2).
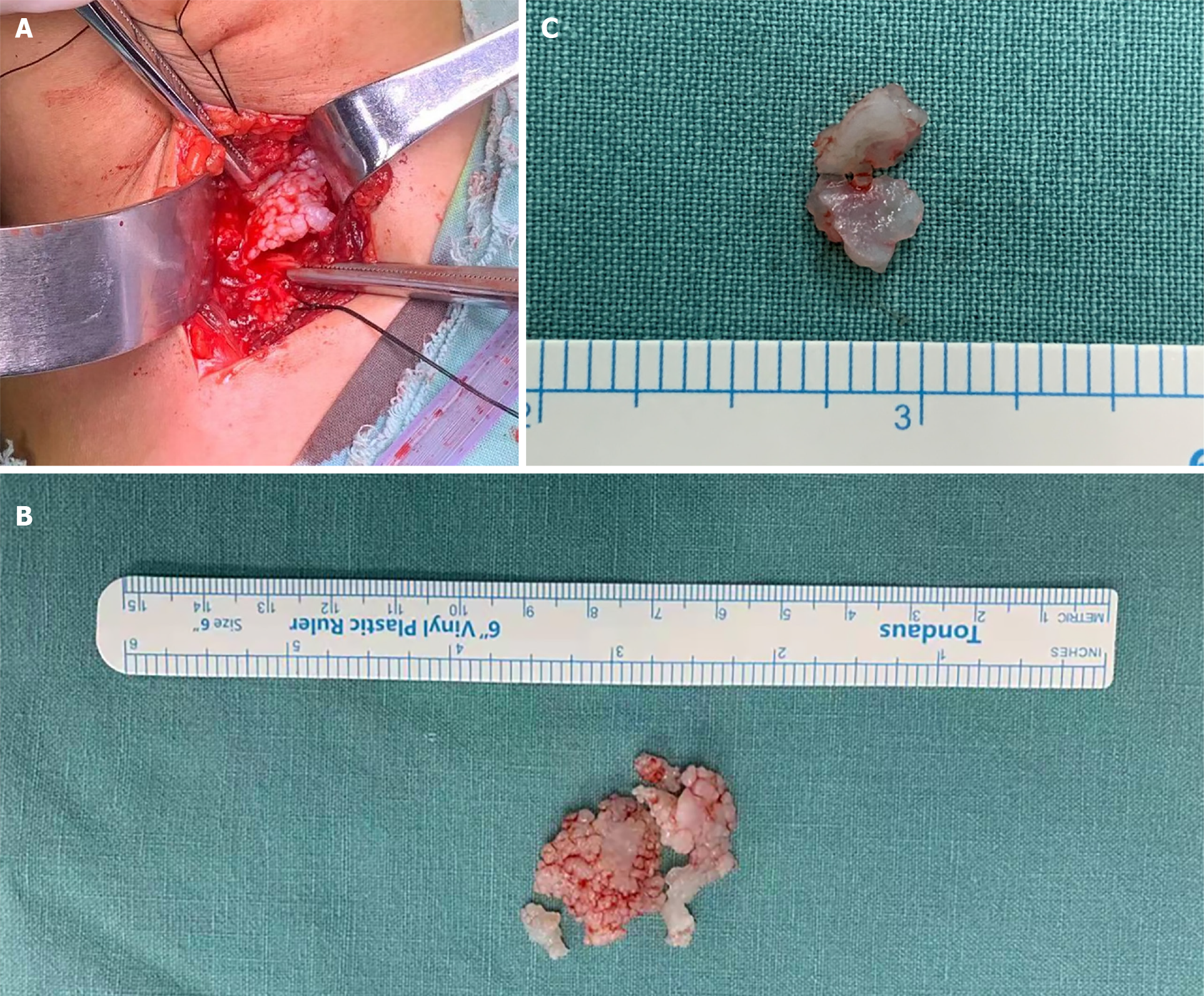
The patient underwent an open biopsy and curettage of the lesion with orthopedic surgery under general anesthesia via a bikini incision of the left hip. After the skin tissue was cut, the hip capsule was revealed by turning down the rectus femoris through the gap between the tensor fasciae latae and the sartorius muscle. The hip capsule was cut along the acetabulum direction. Several irregular, milky white cartilage-like granules (Figure 3A) were seen in the articular cavity, with a maximum size of 2 cm × 2 cm × 0.5 cm. The hip joint was moved, and the cartilage particles were thoroughly cleaned. The hip joint was explored, the left femoral head was slightly flattened, and the synovial tissue showed proliferation and thickening. The sizes of the free bodies were different in block connection; the color was white or milky white; the surface was smooth (Figure 3B); the texture was tough, cartilage-like, and elastic; and the inside of the free bodies was solid without liquid outflow (Figure 3C).
After the surgery, the pain and limp symptoms disappeared. At the 6-wk follow-up, pain and limping had disappeared, and the range of motion of the hip joint was restored to a normal level.
SC is a rare benign lesion first reported by Ambrose Pare in 1558[3]. SC is most commonly seen in the knee joint, followed by the hip joint and elbow joint. It is characterized by the presence of multiple pearl-like osteochondral bodies in the joint.
The disease most commonly occurs in men aged 20-40 years[4], but its incidence is very low; the incidence in children is even lower. Hence, the literature on SC in children is in the form of case reports (Table 1). In 1983, Pelker et al[5] reported an 11-year-old boy who underwent synoviochondroma resection of the hip joint, with good postoperative effect. In the same year, Carey[6] reported two cases of knee joint synoviochondroma, in children aged 9 years and 10 years, and both underwent synovectomy. In 1991, Kistler[7] reported one case of knee joint synoviochondroma. In 2006, Tiedjen[8] reported a 9-year-old patient who underwent arthroscopic treatment without follow-up results. In 2014, Ali et al[9] reported the case of a 12-year-old female child who underwent arthroscopic synovectomy at the hip joint. In 2017, Manesh et al[10] reported a 7-year-old girl who underwent arthrotomy through an anterolateral approach. In 2018, Wen et al[11] reported a 7-year-old male child who underwent synovial chondroma resection of the hip joint. In this case, after 6 wk of postoperative follow-up, the symptoms of pain and claudication disappeared, and the range of motion of the hip joint returned to normal. Our case was the youngest child with SC of the hip reported in the English literature. We performed open synovectomy and removal of the free bodies in the hip lesion; in a subsequent follow-up, his hip pain and claudication symptoms completely disappeared.
The etiology of cartilage tumors is not clear. It is speculated that the connective tissue under the synovial tissue metastasizes into cartilage cells, followed by cartilage ossification, to gradually produce cartilage nodules. These nodules are nourished by the joint fluid and gradually enlarge. Most of the cartilage nodules are later calcified or ossified. Milgram[12] described the classification of SC based on the location of intra-articular free bodies and pathological findings of synovial and free bodies. He described the first stage as an active intrasynovial lesion with microscopic metaplasia of intrasynovial chondromatosis and no gross abnormalities. The second stage was a transitional intrasynovial lesion with synovial osteochondroma and free bodies. The pedicled cartilage bodies could be seen overhanging the synovial membrane without falling off. The third stage was the synovial lesion and the formation of cartilaginous or osteochondral free bodies. The difference in the present case was that obvious isolated bodies were not formed (Figure 3A), but lumps with irregular shapes deve
Imaging examination plays an important role in diagnosing synovial osteo
When we encounter children with hip pain and claudication, increased vigilance and comprehensive physical and imaging examinations should be considered, in order to avoid misdiagnosis and delayed treatment in patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsai HW S-Editor: Li X L-Editor: Webster JR P-Editor: Li X
| 1. | Jiménez-Martín A, Zurera-Carmona M, Santos-Yubero FJ, Pérez-Hidalgo S. Arthroscopic treatment of synovial chondromatosis, an unusual cause of shoulder pain. Reumatol Clin. 2014;10:416-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Davis RI, Hamilton A, Biggart JD. Primary synovial chondromatosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol. 1998;29:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 157] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Barwell R. Clinical lectures on movable bodies in joints. Br Med J. 1876;1:403-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Lasmar NP, Vieira RB, Rosa Jde O, Lasmar RC, Scarpa AC. Synovial chondromatosis. Rev Bras Ortop. 2010;45:490-492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Pelker RR, Drennan JC, Ozonoff MB. Juvenile synovial chondromatosis of the hip. A case report. J Bone Joint Surg Am. 1983;65:552-554. [PubMed] |
| 6. | Carey RP. Synovial chondromatosis of the knee in childhood. A report of two cases. J Bone Joint Surg Br. 1983;65:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Kistler W. Synovial chondromatosis of the knee joint: a rarity during childhood. Eur J Pediatr Surg. 1991;1:237-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Tiedjen K, Senge A, Schleberger R, Wiese M. Synovial osteochondromatosis in a 9-year-old girl: clinical and histopathological appearance. Knee Surg Sports Traumatol Arthrosc. 2006;14:460-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Raza A, Kailash K, Malviya A. Rare cause of hip pain in a young girl. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Philip MC, Usman S. Synovial Chondromatosis: A Rare Differential Diagnosis of Hip Pain in a Child. J Orthop Case Rep. 2017;7:37-39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Wen J, Liu H, Xiao S, Li X, Fang K, Tang Z, Cao S, Li F, Cai G, Hu C. Synovial chondromatosis of the hip joint in childhood: A case report and literature review. Medicine (Baltimore). 2018;97:e13199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Milgram JW. Synovial osteochondromatosis: a histopathological study of thirty cases. J Bone Joint Surg Am. 1977;59:792-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 388] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 13. | Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics. 2007;27:1465-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 200] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 14. | Levine BD, Motamedi K, Seeger LL. Synovial Tumors and Proliferative Diseases. Rheum Dis Clin North Am. 2016;42:753-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |