Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.677
Peer-review started: July 8, 2021
First decision: October 22, 2021
Revised: October 24, 2021
Accepted: December 8, 2021
Article in press: December 8, 2021
Published online: January 14, 2022
Processing time: 187 Days and 19.6 Hours
The short-term therapeutic efficacy of kyphoplasty on Kummell’s disease is obvious. However, postoperative refracture and adjacent vertebral fracture occur occasionally and are difficult to treat. Parkinson's disease (PD) is a pathological disorder associated with heterotopic ossification. In a patient with PD, an intervertebral bridge was formed in a short period of time after postoperative refracture and adjacent vertebral fracture, providing new stability.
A 78-year-old woman had been suffering from PD for more than 10 years. Three months before operation, she developed lower back pain and discomfort. The visual analog scale (VAS) score was 9 points. Preoperative magnetic resonance imaging indicated collapse of the L2 vertebra. Kyphoplasty was performed and significantly decreased the severity of intractable pain. The patient’s VAS score for pain improved from 9 to 2. Fifty days postoperatively, the patient suddenly developed severe back pain, and the VAS score was 9 points. X-ray showed L2 vertebral body collapse, slight forward bone cement displacement, L1 vertebral compression fracture, and severe L1 collapse. The patient was given calcium acetate capsules 0.6 g po qd and alfacalcidol 0.5ug po qd, and bed rest and brace protection were ordered. After conservative treatment for 2 mo, the patient's back pain was alleviated, and the VAS score improved from 9 to 2. Computed tomo
Kyphoplasty is currently a conventional treatment for Kummell's disease, with definite short-term effects. However, complications still occur in the long term, and these complications are difficult to address; thus, the treatment needs to be selected carefully. To avoid refracture, an interlaced structure of bone cement with trabeculae should be created to the greatest extent possible during the injection of bone cement. Surgical intervention may not be urgently needed when a patient with PD experiences refracture and adjacent vertebral fracture, as a strong bridge may help stabilize the vertebrae and relieve pain.
Core Tip: Kyphoplasty is an effective surgery for the treatment of Kummell's disease. However, occasional refracture of the vertebral body can seriously affect the prognosis of patients, and it is very difficult to treat. Parkinson's disease (PD) is a pathological disorder associated with high rates of heterotopic ossification. But no cases of Parkinson's disease causing intervertebral bridge formation have been reported. In our case, the PD patient suffered a refracture of the vertebra after kyphoplasty, and cured by the formation of a large number of intervertebral Bridges.
- Citation: Li J, Liu Y, Peng L, Liu J, Cao ZD, He M. Intervertebral bridging ossification after kyphoplasty in a Parkinson’s patient with Kummell’s disease: A case report. World J Clin Cases 2022; 10(2): 677-684
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/677.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.677
Kummell's disease is characterized by vertebral collapse, pseudarthrosis, and progressive pain caused by ischemic osteonecrosis of the vertebral body[1]. Parkinson's disease (PD) is a pathological disorder associated with heterotopic ossification[2]. However, there have been no reports of PD causing intervertebral bridge formation. Currently, kyphoplasty is an effective surgery for the treatment of Kummell's disease[3]. However, occasional refracture of the vertebral body can seriously affect the prognosis of patients and is very difficult to treat[4].
In the present case, vertebral refracture and adjacent vertebral fracture after kyphoplasty resulted in persistent severe pain and dysfunction. These fractures were cured by extensive callus formation around the T12-L2 vertebrae, and intervertebral bridging ossification provided new stability.
A 78-year-old woman experienced severe low back recurrence pain 2 mo after kyphoplasty.
Two months before admission, the patient underwent kyphoplasty for Kummell's disease at L2, and the postoperative pain was significantly relieved. Two months after surgery, the patient experienced severe back pain recurrence in the same area. The radiographic findings indicated L2 refracture and new L1 fractures.
The patient had been suffering from PD of the rigidity type for more than 10 years. The stage of the patient was Hoehn and Yahr stage IV. She had been taking 600 mg levodopa and 150 mg benserazide hydrochloride orally daily to control the PD symptoms. The patient had significant standing instability when turning her body and could not maintain balance when her body was pushed. Functionally, the patient's mobility was significantly affected, and she could still walk and stand on her own, but she was unable to live independently.
The patient had no previous or family history of similar illnesses.
The patient's L1-2 spinous processes and pain on paravertebral muscle percussion were obvious, and lumbar movement was limited. No neurological injury was observed.
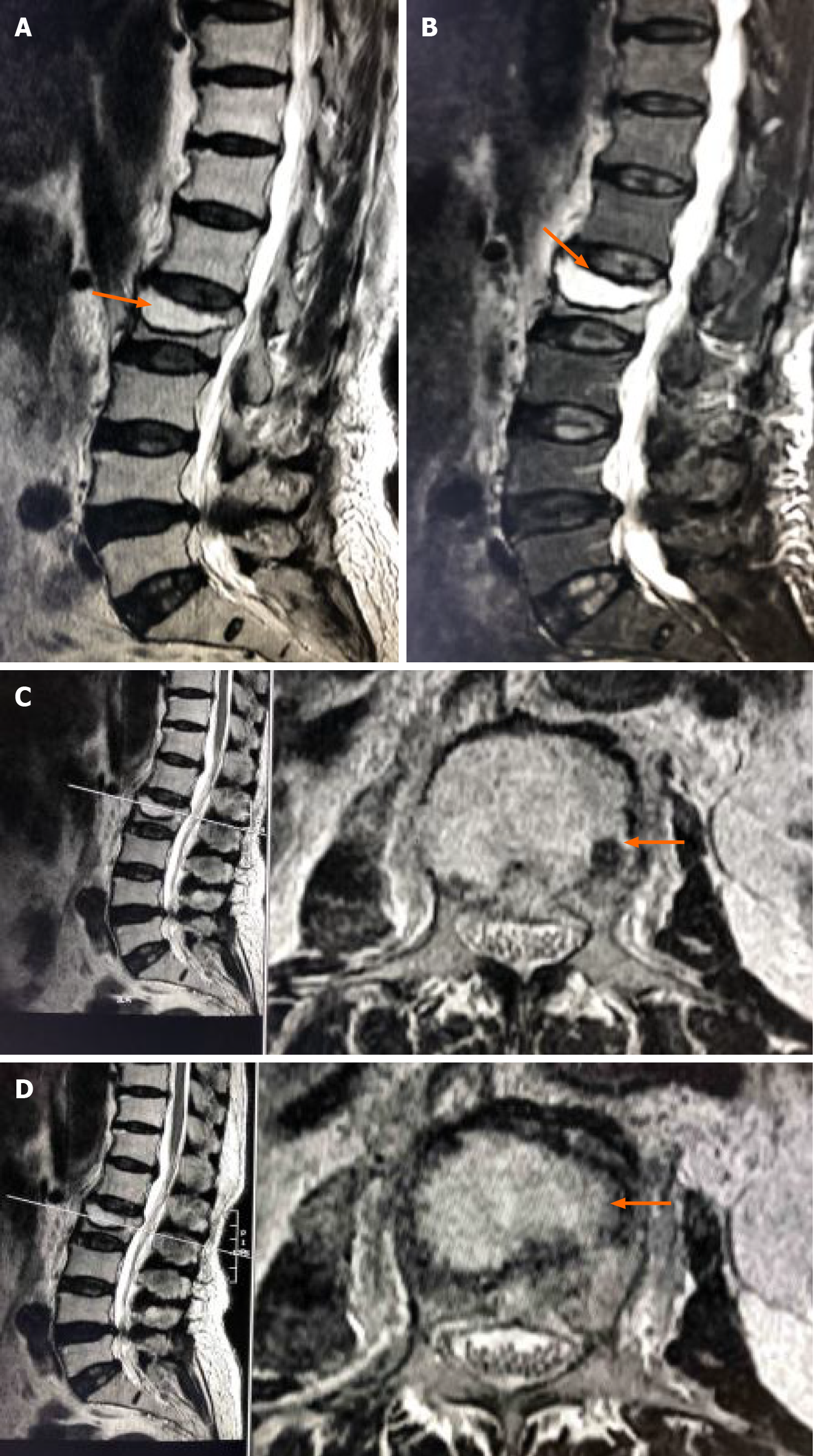
Preoperative magnetic resonance imaging (MRI) indicated collapse of the L2 MRI ertebral body and the formation of an intravertebral cavity-like structure indicated by the arrows (Figure 1A). T2WI with fat suppression (T2WI FS) showed a fluid-filled intravertebral vacuum, with little of the upper endplate structure remaining indicated by the arrows (Figure 1B). T2WI showed a low signal at the cavity edge, indicating vertebral bone necrosis and fibrous perichondrium formation, indicated by the arrows (Figure 1C and D).
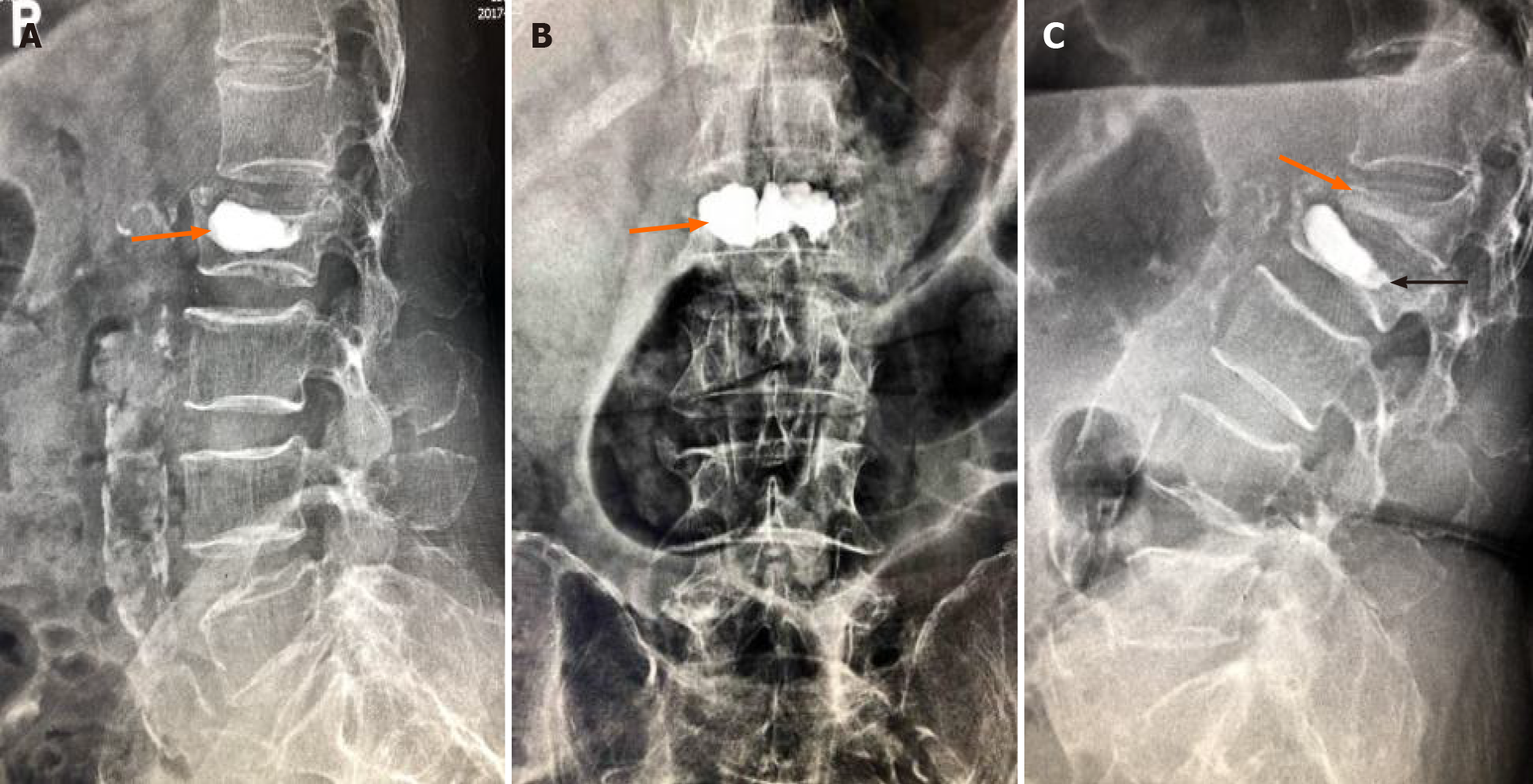
Postoperative X-ray images showed that bone cement filled the cystic cavity of the L2 vertebral body with smooth edges, and there was insufficient bone cement dispersion outside the cystic cavity (Figure 2A and B). Fifty days postoperatively, X-ray images showed L2 vertebral body collapse, slight forward bone cement displacement (indicated by the black arrow), L1 vertebral compression fracture, and severe collapse (indicated by the orange arrow) (Figure 2C).
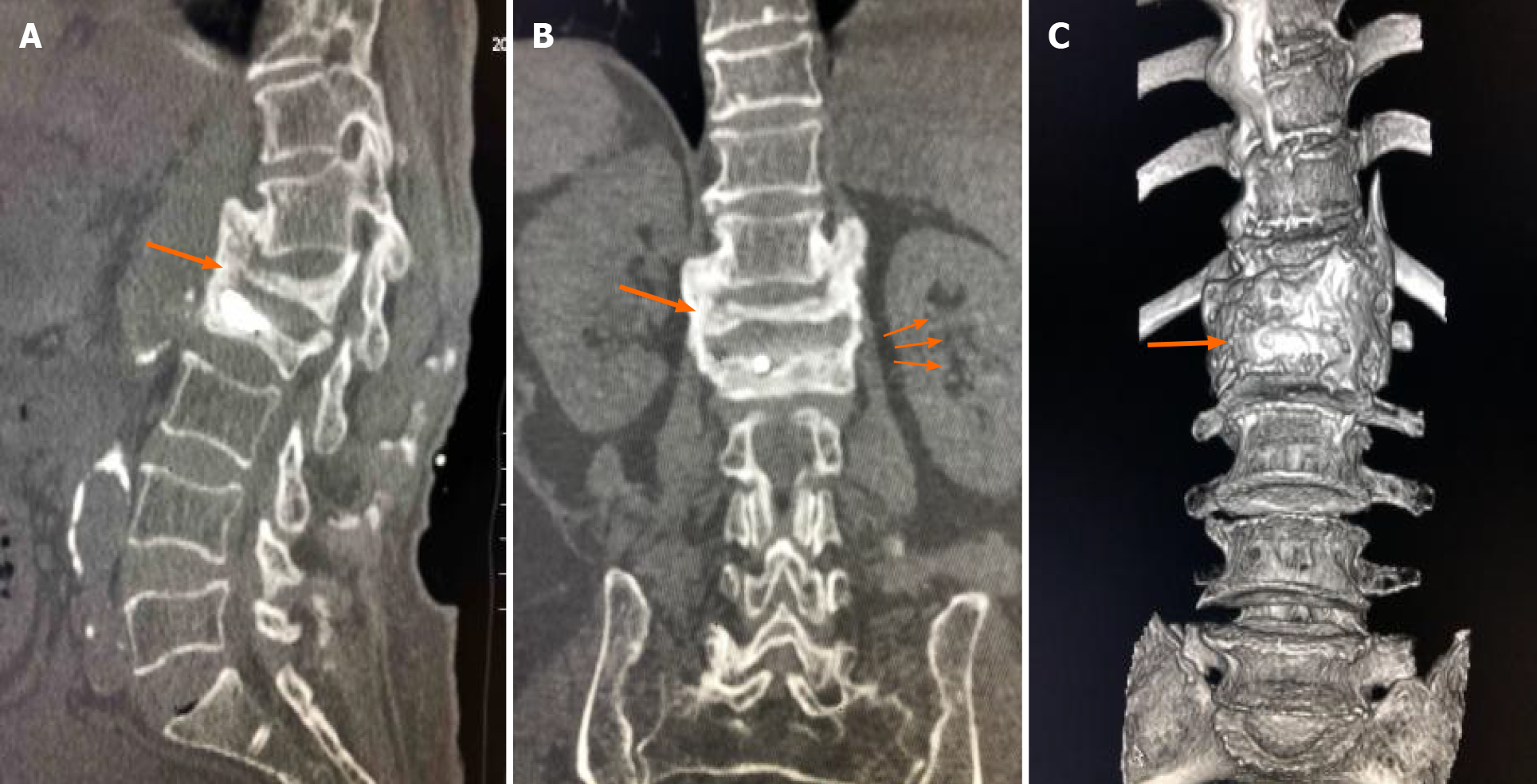
Seven-month follow-up CT indicated extensive callus formation around the T12-L2 vertebrae and intervertebral bridging ossification, providing new stability, as indicated by the arrow (Figure 3).
The patient's L1-2 spinous processes and pain on paravertebral muscle percussion were obvious, and lumbar movement was limited. No neurological injury was observed.
The final diagnosis was Kummell's disease at L2, L2 vertebral refracture, and L1 vertebral compression fracture.
Three months before admission, the patient developed lower back pain and discomfort and was hospitalized. The visual analog scale (VAS) score was 9 points. Preoperative MRI indicated collapse of the L2 vertebral body and the formation of an intravertebral cavity-like structure indicated by the arrows (Figure 1A). T2WI with fat suppression (T2WI FS) showed a fluid-filled intravertebral vacuum, with little of the upper endplate structure remaining indicated by the arrows (Figure 1B). T2WI showed a low signal at the cavity edge, indicating vertebral bone necrosis and fibrous perichondrium formation, indicated by the arrows (Figures 1C and D).
Kyphoplasty was performed, and the severity of the intractable pain significantly decreased. Postoperative X-ray images showed that bone cement filled the cystic cavity of the L2 vertebral body with smooth edges, and there was insufficient bone cement dispersion outside the cystic cavity (Figure 2A and B). The patient’s VAS score for pain improved from 9 to 2. Fifty days postoperatively, the patient suddenly developed severe back pain, and the VAS pain score was 9 points. X-ray images showed L2 vertebral body collapse, slight forward bone cement displacement (Indicated by the black arrow), L1 vertebral compression fracture, and severe collapse (Indicated by the orange arrow) (Figure 2C).
The patient refused surgery, so she was given calcium acetate capsules (0.6 g po qd) and alfacalcidol (0.5 µg po qd), and bed rest and brace protection were ordered.
After conservative treatment for 2 mo, the patient's back pain was alleviated, and the VAS score improved from 9 to 2. CT at the 7-mo follow-up indicated extensive callus formation around the T12-L2 vertebrae and intervertebral bridging ossification, providing new stability, as indicated by the arrow (Figure 3).
The refracture of cemented vertebrae, displacement of bone cement and fracture of adjacent vertebrae are rare complications after percutaneous kyphoplasty for Kummell's disease and are relatively difficult to addres[5]. PD is a pathological disorder associated with heterotopic ossification[6,7]. There have been no reports in the literature on the occurrence or outcomes of postoperative complications in patients with both of these diseases at the same time.
Mckiernan et al[8] reported that osteonecrosis and pseudarthrosis are the main risk factors for refracture. Due to the presence of fractures in the movable vertebrae, the bone cement tends to form a mass structure rather than spread throughout the trabecular bone[9]. During polymethyl methacrylate (PMMA) injection, the bone cement follows the path of least resistance through the intravertebral space, resulting in insufficient filling and a lack of interlacing with nearby bone tissue[10].
In addition, the formation of fibrous perichondrium at the internal edge of the vertebral cystic cavity prevented PMMA from forming an intersecting structure with the trabeculae[11] (Figure 1D). The stimulation of mechanical stress at the bone-cement interface may lead to microfractures of the vertebral body, highly progressive collapse of the vertebral body, failure at the bone-cement interface, and even fracture of the bone cement and collapse of the vertebral body[12]. Therefore, Heo et al[13] proposed that vertebroplasty and kyphoplasty may be contraindicated by osteonecrosis or pseudoarthrosis of the fractured vertebral body.
After cementing the vertebral body, the protrusion of the endplate of the enhanced vertebral body increased as the height of the vertebral body was restored to a certain extent. At the same time, bone cement and residual endplates were fixed in the vertebral body adjacent to the endplate of the adjacent vertebral body. These factors lead to a lack of cushioning between adjacent vertebrae and bone cement, increasing the risk of refracture[14,15] (Figure 2C).
According to Fahim DK et al[16], the normal intervertebral disc, the endplate and part of the trabecular bone of the treated vertebral body act as buffers between the bone cement and adjacent vertebral body. When bone cement reaches the level of the intervertebral disc, the tissue buffer decreases or completely disappears, leading to a high rate of adjacent fractures. Baroud et al[17] found that bulging of the enhanced endplate results in hardening of the intervertebral joint and the entire motion segment. A high intervertebral pressure and an inward-facing endplate bulge may be responsible for adjacent fractures[18,19].
Refractured vertebrae and adjacent fractured vertebrae are fused through intervertebral bridge formation at T12, L1 and L2 to achieve ultimate stability and significantly improve pain in patients within a short period (Figure 3).
PD has been described as a disease associated with HO incidence[6,7]. Namazi proposed a pathway by which PD mediates heterotopic ossification development[20]. In PD, peripheral blood mononuclear cells produce interleukin-1, interleukin-6, and tumor necrosis factor, which have been shown to play an important role in HO[21-24]. In addition, levodopa mediates ectopic ossification, has been found to stimulate bone formation, callus formation, and healing through growth hormone (GH), and has been used in vivo to promote bone growth after internal fixation of fractures[25-29].
The patient had PD for 10 years and was treated with oral levodopa and benserazide hydrochloride, so we hypothesized that the formation of her intervertebral bridge might be related to her disease and drug treatment. However, the existence of other interfering factors, such as the fracture itself, mechanical instability, blood leakage, and bone cement stimulation, which are all factors that stimulate the growth of fracture, cannot completely explain the formation of a large number of calli in a short period of time in patients with intervertebral bone bridges connecting three vertebrae[29]. More case studies and further laboratory studies may be needed to confirm this phenomenon.
Kyphoplasty is currently a common treatment for Kummell's disease, with definite short-term effects. However, complications still occur in the long term, and these complications are difficult to address; thus, the treatment needs to be selected carefully. To avoid refracture, an interlaced structure of bone cement with trabeculae should be created to the greatest extent possible during the injection of bone cement. Surgical intervention may not be urgently needed when a patient with PD experiences refracture and adjacent vertebral fracture, as a strong bridge may help stabilize the vertebrae and relieve pain.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Byeon H, Tsai ST S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Dai SQ, Qin RQ, Shi X, Yang HL. Percutaneous vertebroplasty vs kyphoplasty for the treatment of neurologically intact osteoporotic Kümmell's disease. BMC Surg. 2021;21:65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Ifedi BO, Best CM, Reichel LM. Heterotopic ossification following distal radius fractures in a patient with Parkinson disease treated with levodopa-carbidopa. J Hand Surg Am. 2013;38:1259-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | JB Chen, YP Xiao, D Chen, JZ Chang, Te Li. Clinical observation of two bone cement distribution modes of percutaneous vertebroplasty in the treatment of thoracolumbar Kümmell's disease. J Orthop Surg Res. 15:250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Hu L, Sun H, Wang H, Cai J, Tao Y, Feng X, Wang Y. Cement injection and postoperative vertebral fractures during vertebroplasty. J Orthop Surg Res. 14:228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Zhu J, Zhang K, Luo K, Qiu Z, Yang S, Cui F, Weng X, Jiang G. Mineralized Collagen Modified Polymethyl Methacrylate Bone Cement for Osteoporotic Compression Vertebral Fracture at 1-Year Follow-up. Spine (Phila Pa 1976). 2019;44:827-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Shah A, Uy M, Yan JR, Khan M, Alolabi B. Heterotopic Ossification following Total Elbow Arthroplasty in a Patient with Parkinson's Disease: Case Report and Literature Review. Case Rep Surg. 2020;2020:2068045. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Biz C, Pavan D, Frizziero A, Baban A, Iacobellis C. Heterotopic ossification following hip arthroplasty: a comparative radiographic study about its development with the use of three different kinds of implants. J Orthop Surg Res. 2015;10:176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | McKiernan F, Jensen R, Faciszewski T. The dynamic mobility of vertebral compression fractures. J Bone Miner Res. 2003;18:24-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 207] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 9. | Li YX, Guo DQ, Zhang SC, Liang, Yuan K, Mo GY, Li DX, Guo HZ, Tang Y, Luo PJ. Risk factor analysis for re-collapse of cemented vertebrae after percutaneous vertebroplasty (PVP) or percutaneous kyphoplasty (PKP). Int Orthop. 2018;42:2131-2139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 80] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 10. | Wang M, Zhang L, Fu Z, Wang H, Wu Y. Selections of Bone Cement Viscosity and Volume in Percutaneous Vertebroplasty: A Retrospective Cohort Study. World Neurosurg. 2021;150:e218-e227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Heo DH, Choi JH, Kim MK, Choi HC, Jeong JH, Chin DK, Cho YJ. Therapeutic efficacy of vertebroplasty in osteoporotic vertebral compression fractures with avascular osteonecrosis: a minimum 2-year follow-up study. Spine (Phila Pa 1976). 2012;37:E423-E429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Zhu S, Su Q, Zhang Y, Sun Z, Yin P, Hai Y. Risk factors of cemented vertebral refracture after percutaneous vertebral augmentation: a systematic review and meta-analysis. Neuroradiology. 2020;62:1353-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Heo DH, Chin DK, Yoon YS, Kuh SU. Recollapse of previous vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int. 2009;20:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Zhang T, Wang Y, Zhang P, Xue F, Zhang D, Jiang B. What Are the Risk Factors for Adjacent Vertebral Fracture After Vertebral Augmentation? Global Spine J. 2020;2192568220978223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 15. | Chen C, Fan P, Xie X, Wang Y. Risk Factors for Cement Leakage and Adjacent Vertebral Fractures in Kyphoplasty for Osteoporotic Vertebral Fractures. Clin Spine Surg. 2020;33:E251-E255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Fahim DK, Sun K, Tawackoli W, Mendel E, Rhines LD, Burton AW, Kim DH, Ehni BL, Liebschner MA. Premature adjacent vertebral fracture after vertebroplasty: a biomechanical study. Neurosurgery. 2011;69:733-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Baroud G, Nemes J, Heini P, Steffen T. Load shift of the intervertebral disc after a vertebroplasty: a finite-element study. Eur Spine J. 2003;12:421-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 225] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 18. | Chen WJ, Kao YH, Yang SC, Yu SW, Tu YK, Chung KC. Impact of cement leakage into disks on the development of adjacent vertebral compression fractures. J Spinal Disord Tech. 2010;23:35-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 80] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Morozumi M, Matsubara Y, Muramoto A, Morita Y, Ando K, Kobayashi K, Machino M, Ota K, Tanaka S, Kanbara S, Ito S, Ishiguro N, Imagama S. A Study of Risk Factors for Early-Onset Adjacent Vertebral Fractures After Kyphoplasty. Global Spine J. 2020;10:13-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Reichel LM, Ifedi BO, Best CM. In reply. J Hand Surg Am. 2013;38:1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Brodacki B, Staszewski J, Toczyłowska B, Kozłowska E, Drela N, Chalimoniuk M, Stepien A. Serum interleukin (IL-2, IL-10, IL-6, IL-4), TNFalpha, and INFgamma concentrations are elevated in patients with atypical and idiopathic parkinsonism. Neurosci Lett. 2008;441:158-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 244] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 22. | Bessler H, Djaldetti R, Salman H, Bergman M, Djaldetti M. IL-1 beta, IL-2, IL-6 and TNF-alpha production by peripheral blood mononuclear cells from patients with Parkinson's disease. Biomed Pharmacother. 1999;53:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 100] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 23. | Olney RC. Regulation of bone mass by growth hormone. Med Pediatr Oncol. 2003;41:228-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Kimura A, Endo T, Inoue H, Takeshita K. Intervertebral bridging ossifications increase the risk of intravertebral cleft formation following a vertebral compression fracture. Eur Spine J. 2016;25:3456-3462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | van der Meer J. [Practolol (Eraldin)]. Ned Tijdschr Geneeskd. 1975;119:999-1000. [PubMed] |
| 26. | Pritchett JW. L-dopa in the treatment of nonunited fractures. Clin Orthop Relat Res. 1990;293-300. [PubMed] |
| 27. | Costa ER, Weinhold P, Tayrose GA, Hooker JA, Dahners LE. The effect of levodopa or levodopa-carbidopa (sinemet) on fracture healing. J Orthop Trauma. 2006;20:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Chihara K, Kashio Y, Kita T, Okimura Y, Kaji H, Abe H, Fujita T. L-dopa stimulates release of hypothalamic growth hormone-releasing hormone in humans. J Clin Endocrinol Metab. 1986;62:466-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 29. | Liu B, Sun C, Xing Y, Zhou F, Tian Y, Yang Z, Hou G. Intervertebral Bridging Ossification After Percutaneous Kyphoplasty in Osteoporotic Vertebral Compression Fractures. World Neurosurg. 2019;127:633-636.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |