Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.656
Peer-review started: June 14, 2021
First decision: October 16, 2021
Revised: October 22, 2021
Accepted: December 8, 2021
Article in press: December 8, 2021
Published online: January 14, 2022
Processing time: 212 Days and 1.4 Hours
Few reports have described lumbar foraminal stenosis-induced radiculopathy after treatment by full-endoscopic spine surgery (FESS) combined with percutaneous vertebroplasty (PVP) in patients with vertebral compression fractures. We herein report such a case, including the patient’s treatment process and doctor’s surgical experience.
A 79-year-old man presented with symptoms of radiculopathy after sustaining L4 vertebral compression fractures. Imaging and physical examination revealed L4 vertebral compression fractures combined with L3/4 Lumbar foraminal stenosis (LFS). The patient’s symptoms were low back pain with pain in the lateral left leg. Although many reports have described radiculopathy induced by osteoporotic vertebral compression fractures, the use of FESS combined with PVP has rarely been reported. This case report indicates that the combination of FESS and PVP is a safe and effective approach for the treatment of LFS-induced radiculopathy after vertebral compression fractures. This minimally invasive technique has great potential to replace traditional lumbar fixation and decompression surgery. Thus, we suggest the continued accumulation of similar cases to discuss the wider application of FESS.
For patients with osteoporotic vertebral compression fracture (OVCF) and LFS, PVP and FESS can be used to restore the vertebral height and reduce the pressure around the intervertebral foramen. Additionally, the combination of FESS and PVP can treat the pain or numbness of the low back and lower limbs and allow for recovery in a short time with excellent postoperative effects. In general, FESS is a good treatment for radiculopathy caused by foraminal stenosis after OVCF.
Core Tip: Clinically, the number of patients with osteoporotic vertebral compression fractures combined with nerve root entrapment symptoms is gradually increasing. Percutaneous vertebroplasty alone can not completely relieve the clinical symptoms of patients. We found that the choice of total spinal endoscopic surgery combined with percutaneous vertebroplasty can be a good treatment for such patients, suggesting that combined with minimally invasive technology is a positive and effective surgical treatment.
- Citation: Zhao QL, Hou KP, Wu ZX, Xiao L, Xu HG. Full-endoscopic spine surgery treatment of lumbar foraminal stenosis after osteoporotic vertebral compression fractures: A case report. World J Clin Cases 2022; 10(2): 656-662
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/656.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.656
Osteoporotic vertebral compression fracture (OVCF) is the most common spinal fracture in elderly people[1] and is caused by osteoporosis, violent trauma, or spinal tumours. Traditional percutaneous vertebroplasty (PVP) under X-ray fluoroscopy is a safe and effective surgical approach for the treatment of OVCFs in elderly patients[2]. Lumbar foraminal stenosis (LFS) is one of the more serious lumbar degenerative diseases among patients with low back and leg pain, leading to nerve root com
A 79-year-old man presented to the emergency department with a chief complaint of low back pain and limited mobility caused by an accidental fall 9 d previously.
The patient accidentally fell 9 d ago and failed to effectively respond to conservative treatment.
The patient had a history of hypertension for which he has been taking Betaloc tablets over an extended period of time. The patient had no family history of congenital, allergic, or systemic disease.
The patient had no history of familial genetic diseases.
Physical examination revealed a slight alteration in the physiological curvature of the spine, slight scoliosis, restricted range of motion in the lower back, tenderness over the L4 spinous process, and positive paravertebral muscle tenderness. The skin sensation of both upper extremities was normal, with a grade of 5 for muscle strength of the main muscle groups. The skin sensation of the lateral left leg was decreased, with normal sensation of the skin of the opposite leg. Straight-left leg-raise was positive above 45°. The patellar reflex of the left lower extremity was decreased, the quadriceps muscle strength of the left lower extremity was grade 4, and the right lower extremity was normal.
Laboratory examinations, including liver function tests, renal function tests, and routine urine tests, revealed no abnormalities. Lymphocyte count, eosinophil count and haematocrit decreased slightly; neutrophils, mean corpuscular volume and D-D slightly increased; other tests such as routine whole blood and coagulation function tests were normal.
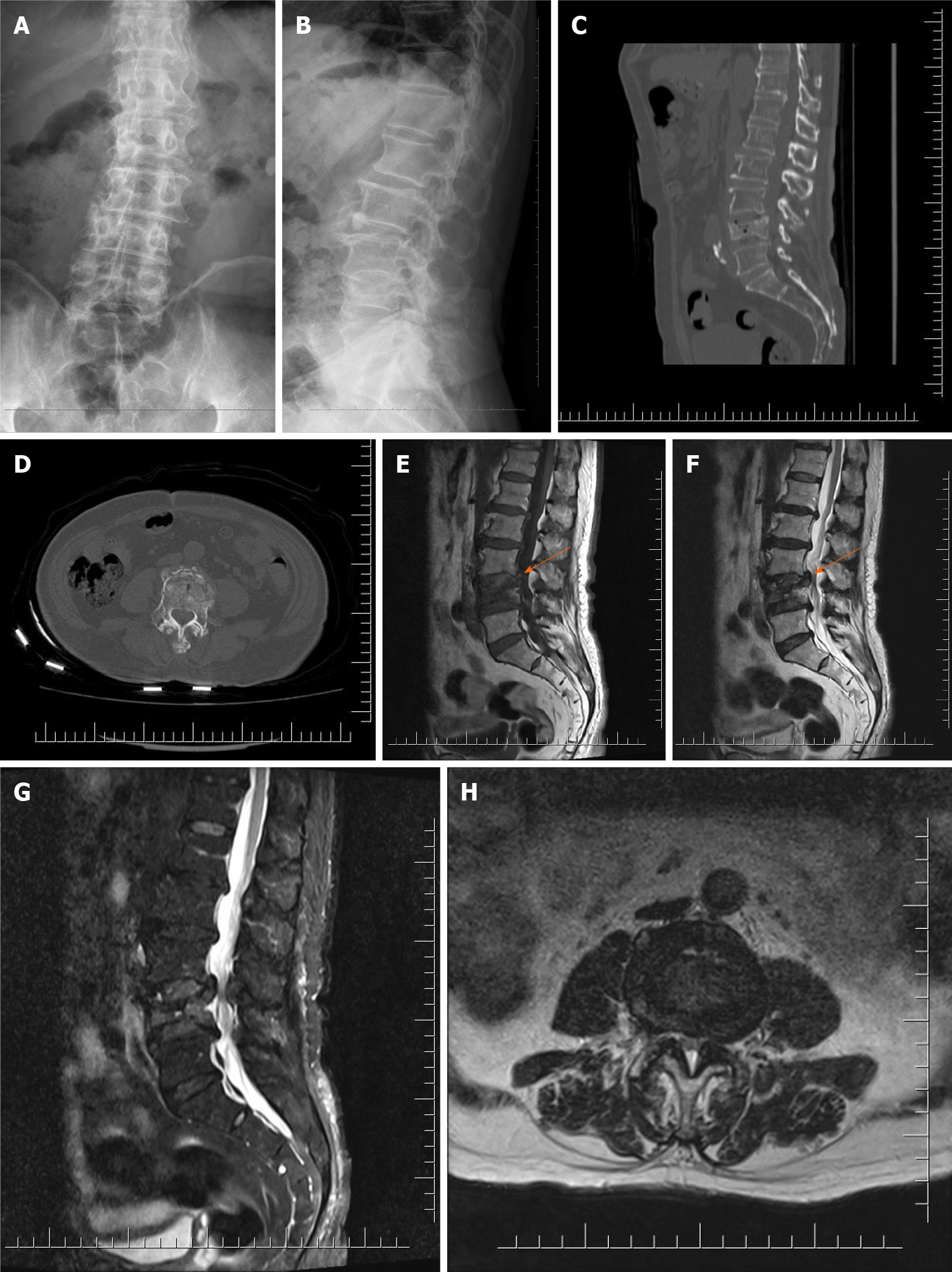
Radiography and computed tomography (CT) of the lumbar spine (Figure 1A-D) revealed an L4 vertebral compression fracture. Magnetic resonance imaging (MRI) (Figure 1E-H) showed that the left nerve root canal was significantly narrowed due to the oppression of the fracture fragment at the posterior upper edge of the L4 vertebral body (orange arrow).
L4 vertebral compression fracture and L3/4 Lumbar foraminal stenosis.
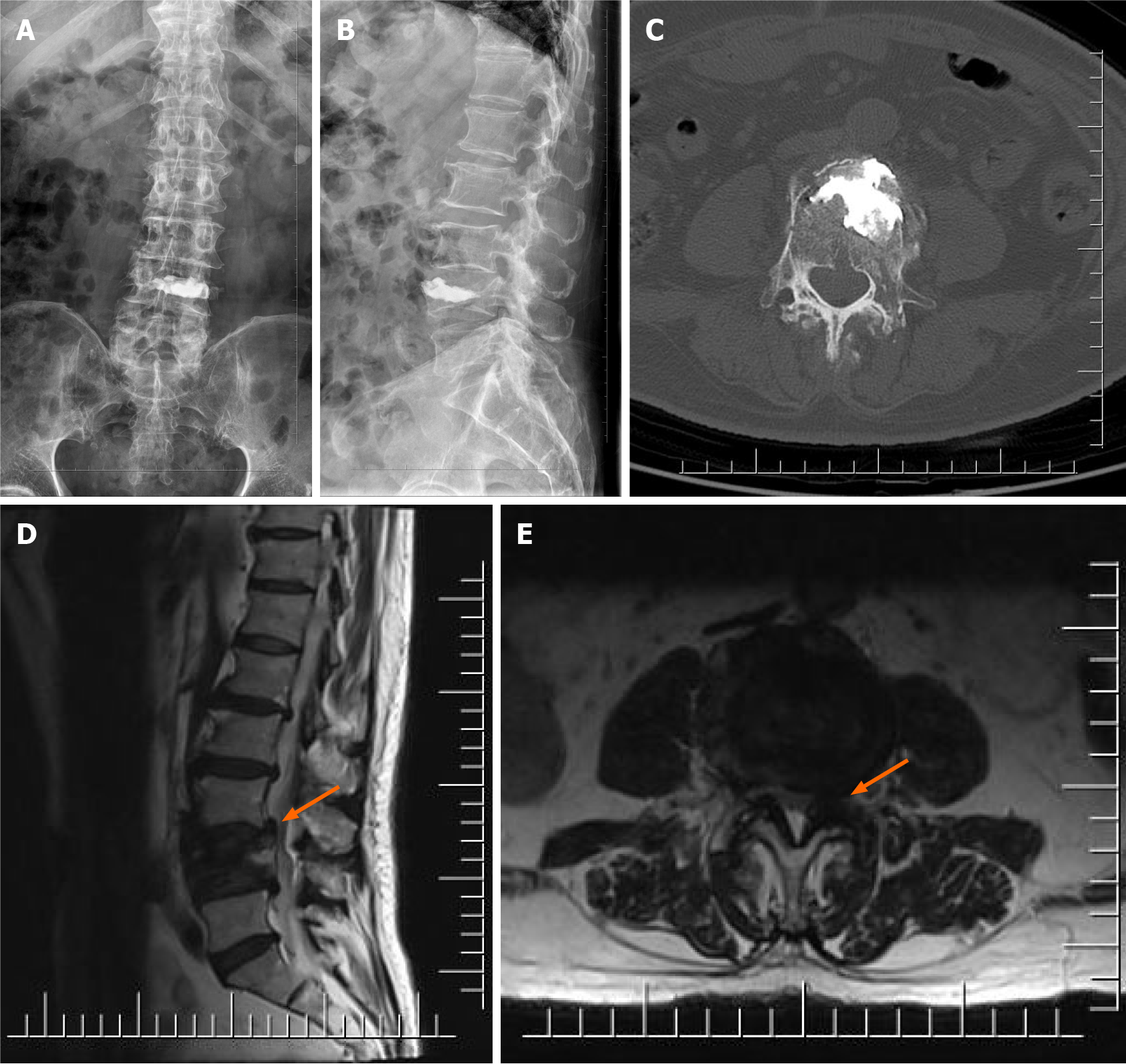
In the first surgery, the patient underwent left L4 pedicle puncture under local anaesthesia and overall monitoring in the prone position. During close monitoring of the patient’s vital signs, approximately 3.3 mL of bone cement was injected into the L4 vertebral body through the unilateral pedicle. Postoperatively, the mobility of the lower extremities recovered to baseline. Low back pain was significantly relieved, but left lateral leg pain was still present. The patient was instructed to take an oral form of diclofenac sodium sustained-release tablets, eperisone, and a neurotrophic drug. One week later, the pain was still present. Postoperative lumbar anteroposterior and lateral X-rays (Figure 2A and B), lumbar CT (Figure 2C), and lumbar MRI (Figure 2D and E) revealed changes in the L4 vertebral body after bone cement injection, particularly bone marrow oedema of the L4 vertebral body, as well as bilateral thickening of the ligamentum flavum at the L3/4 level. After PVP, necrosis was still present in the lateral recess of the L3/4 intervertebral foramen (orange arrow).
The patient then underwent FESS under local anaesthesia and decompression of the root canal of the L3/4 left nerve. Intraoperatively, significant hyperplasia of the L3/4 left articular process and hypertrophy of the ligamentum flavum were observed. The hypertrophic ligamentum flavum was removed, and the nerve root was fully released. The surgery was successful. Postoperatively, the patient underwent electrocardiographic monitoring, antibiotic prophylaxis, rehydration, and symptomatic treatment with close observation of his clinical status.
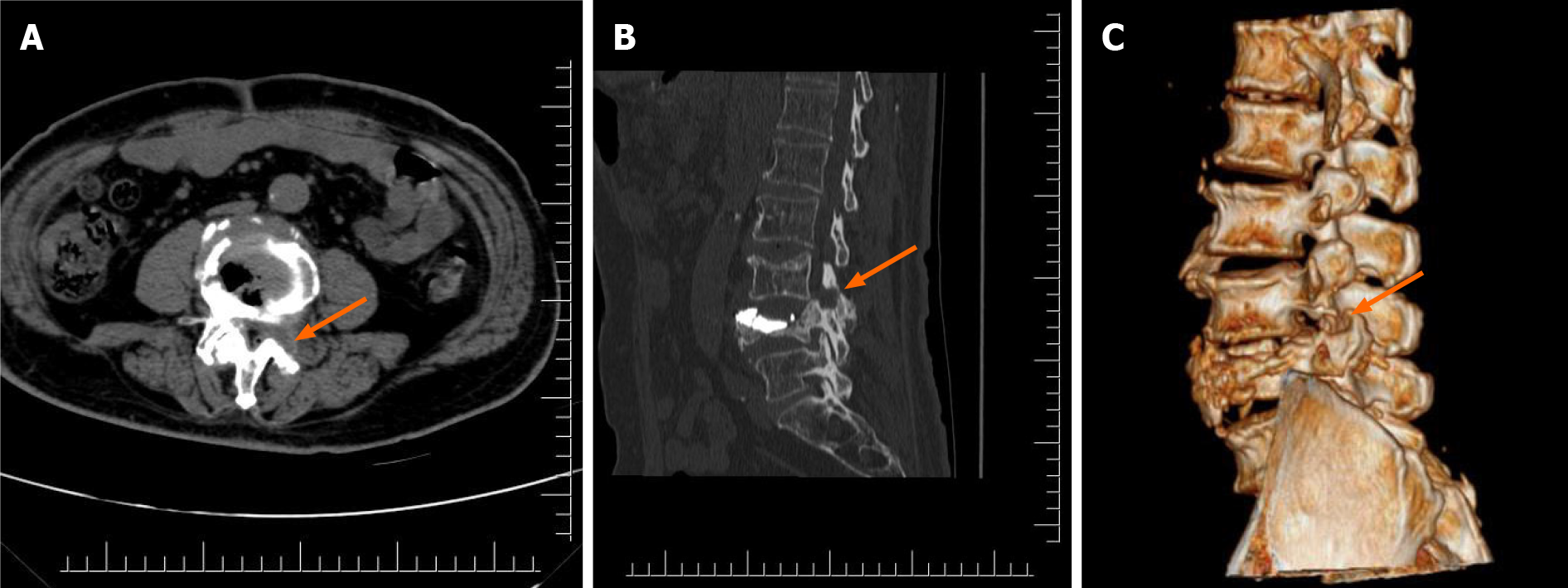
One month after discharge, three-dimensional lumbar CT revealed postoperative changes at the site of L4 vertebral bone cement injection as well as complete decompression in the L3/4 left nerve root canal and lateral recess (Figure 3, orange arrow). In addition, the patient complained of occasional slight pain in the left lateral leg, possibly caused by the loss of structural support of the surrounding tissue of the L4 nerve root after decompression and contact with the bone or tissue at the decompression site with movement. At the follow-up 3 mo after discharge, the mild leg pain had completely resolved.
With the recent ageing of the global population, the incidence of vertebral compression fractures is increasing. In a few cases, vertebral compression fractures lead to compression of the spinal cord[6]. In addition to severe back pain, such patients develop lower extremity pain or numbness. Sasaki et al[7] described 66 patients with vertebral compression fractures, 10 (15.2%) of whom had persistent radiculopathy. Seven patients were diagnosed with spinal canal stenosis, two with LFS, and one with lumbar disc herniation. Radiculopathy induced by lumbar vertebral compression fractures has been reported[8,9] and occurs secondary to LFS caused by compression of nerves by bone fragments or vertebral compression. The development of LFS after vertebral compression fractures may be due to changes in the foraminal geometry after fracture[10]. PVP and FESS may be effective approaches to relieve low back pain in patients with OVCFs combined with LFS.
We have herein reported a case of OVCF combined with LFS after lumbar fractures because of continuous movement and designed a novel endoscopic surgery technique. After PVP, FESS was performed to treat the nerve root disease induced by LFS after lumbar vertebral compression fracture, with a very satisfactory curative effect. Degenerative changes in L3/4 were observed intraoperatively, including hypertrophy of the ligamentum flavum, disc herniation, and entry of fibrous membrane-covered posterior wall debris into the intervertebral foramen. After L4 vertebral compression, the patient did not comply with the doctor’s advice regarding bed rest and instead continued his daily activities, further compressing and aggravating the L4 vertebral upper endplate, which resulted in symptoms of the lower extremity root. Severe leg pain induced by LFS after OVCF requires surgical treatment, but conservative treatment is also feasible for some patients with mild symptoms. We observed the patient for 1 wk after PVP to evaluate whether foraminal decompression could be avoided. It is possible to recover the height of the intervertebral foramen after distraction of the compressed vertebral body with bone cement. The patient’s lower extremity pain was not relieved over time under conservative treatment; therefore, FESS was performed. Weber et al[11] reported a case of radiculopathy after vertebral compression fracture in which a bone block compressed the spinal cord. After 2 wk of conservative treatment, the patient’s symptoms remained unchanged. Lumbar fusion and internal fixation were then performed, and the patient recovered well in the later stage. Isogai et al[12] reported that lumbar fusion and internal fixation were effective for radiculopathy after vertebral compression fracture. However, internal fixation is not suitable for the physical condition of elderly patients with osteoporosis. The risks of loosening of the internal fixation device and adverse reactions caused by the invasive operation are higher in these patients[13]. Our report shows that the combined use of bone cement and spinal endoscopy helps patients undergo a safer operation and achieve early rehabilitation. However, longer follow-up is required to assess the development of spinal instability over time.
Few studies to date have focused on the use of FESS in the treatment of nerve root disease induced by LFS after vertebral compression fracture. Full-visualization laminectomy or foraminal enlargement is a basic procedure of FESS. In the past, FESS was often used for lumbar discectomy[14]. In recent years, it has been gradually used for decompression of the spinal canal or nerve root canal[15], avoiding excessive medical treatment caused by unnecessary lumbar interbody fusion. Kim et al[16] reported radiculopathy caused by compression of nerve roots by osteophytes of fractured vertebrae after vertebral compression fractures. The incidence of radiculopathy in lower lumbar vertebral fractures is higher. Bone fragments (osteophytes) of the collapsed vertebrae might fall into the intervertebral foramen and directly compress the nerve roots. Philips et al[8] described three women with an average age of 81.7 years. The symptoms of nerve root compression were relieved by FESS via removal of bone cement leakage and osteophytes. Postoperative recovery was good, and no complications were observed. In this case, FESS showed good minimally invasive performance. Under spinal endoscopy, the osteophyte compressing the nerve root was completely removed, and the compressed part of the intervertebral foramen was relieved, thus avoiding the tissue damage caused by lumbar open surgery.
For patients with OVCF and LFS, PVP for restoring vertebral height and FESS for decompression around the foramina can remit pain or numbness in the lower back and lower extremities, allowing the patient to recover in a short time with an excellent postoperative effect. Generally, FESS is a good treatment for LFS-induced radiculopathy after OVCF.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Muthu S S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Parreira PCS, Maher CG, Megale RZ, March L, Ferreira ML. An overview of clinical guidelines for the management of vertebral compression fracture: a systematic review. Spine J. 2017;17:1932-1938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | Wang H, Sribastav SS, Ye F, Yang C, Wang J, Liu H, Zheng Z. Comparison of Percutaneous Vertebroplasty and Balloon Kyphoplasty for the Treatment of Single Level Vertebral Compression Fractures: A Meta-analysis of the Literature. Pain Physician. 2015;18:209-222. [PubMed] |
| 3. | Orita S, Inage K, Eguchi Y, Kubota G, Aoki Y, Nakamura J, Matsuura Y, Furuya T, Koda M, Ohtori S. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 2016;26:685-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 4. | Ahn Y. Percutaneous endoscopic decompression for lumbar spinal stenosis. Expert Rev Med Devices. 2014;11:605-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 131] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 5. | Gu S, Hou K, Jian W, Du J, Xiao S, Zhang X. Working Cannula-Based Endoscopic Foraminoplasty: A Technical Note. Biomed Res Int. 2018;2018:4749560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Tezer M, Ozturk C, Erturer E, Aydogan M, Hamzaoglu A. Bilateral L5 radiculopathy due to osteoporotic L1 vertebral fracture: A case report. J Spinal Cord Med. 2006;29:430-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Sasaki M, Aoki M, Nishioka K, Yoshimine T. Radiculopathy caused by osteoporotic vertebral fractures in the lumbar spine. Neurol Med Chir (Tokyo). 2011;51:484-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Philips GAC, Oshima Y, Inoue H, Kitagawa T, Iwai H, Takano Y, Inanami H, Koga H. Full-endoscopic spine surgery for radiculopathy after osteoporotic vertebral compression fractures: a case report. J Spine Surg. 2020;6:466-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Senturk S, Unsal UU. A New Technique That Percutaneous Endoscopic Decompression and Vertebroplasty in a Patient With Osteoporotic Vertebral Fracture: A Case Report. Spine (Phila Pa 1976). 2020;45:E967-E971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Maiman D, Curry W, Yoganandan N, Pintar F. Intervertebral foramen narrowing during vertical dynamic loading. Traffic Inj Prev. 2020;21:S163-S165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Weber M, Uehlinger K, Gerber H. Osteoporotic vertebral compression fracture causing neurologic deficit. J Clin Rheumatol. 2002;8:166-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Isogai N, Hosogane N, Funao H, Nojiri K, Suzuki S, Okada E, Ueda S, Hikata T, Shiono Y, Watanabe K, Kaito T, Yamashita T, Fujiwara H, Nagamoto Y, Terai H, Tamai K, Matsuoka Y, Suzuki H, Nishimura H, Tagami A, Yamada S, Adachi S, Ohtori S, Orita S, Furuya T, Yoshii T, Ushio S, Inoue G, Miyagi M, Saito W, Imagama S, Ando K, Sakai D, Nukaga T, Kiyasu K, Kimura A, Inoue H, Nakano A, Harimaya K, Kawaguchi K, Yokoyama N, Oishi H, Doi T, Ikegami S, Shimizu M, Futatsugi T, Kakutani K, Yurube T, Oshima M, Uei H, Aoki Y, Takahata M, Iwata A, Seki S, Murakami H, Yoshioka K, Endo H, Hongo M, Nakanishi K, Abe T, Tsukanishi T, Ishii K. The Surgical Outcomes of Spinal Fusion for Osteoporotic Vertebral Fractures in the Lower Lumbar Spine with a Neurological Deficit. Spine Surg Relat Res. 2020;4:199-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Rometsch E, Spruit M, Zigler JE, Menon VK, Ouellet JA, Mazel C, Härtl R, Espinoza K, Kandziora F. Screw-Related Complications After Instrumentation of the Osteoporotic Spine: A Systematic Literature Review With Meta-Analysis. Global Spine J. 2020;10:69-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 14. | Sivakanthan S, Hasan S, Hofstetter C. Full-Endoscopic Lumbar Discectomy. Neurosurg Clin N Am. 2020;31:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 15. | Ahn Y. Current techniques of endoscopic decompression in spine surgery. Ann Transl Med. 2019;7:S169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Kim DE, Kim HS, Kim SW. Clinical analysis of acute radiculopathy after osteoporotic lumbar compression fracture. J Korean Neurosurg Soc. 2015;57:32-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |