Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.528
Peer-review started: June 22, 2021
First decision: September 28, 2021
Revised: September 29, 2021
Accepted: December 10, 2021
Article in press: December 10, 2021
Published online: January 14, 2022
Processing time: 203 Days and 15.9 Hours
Currently, the standard surgical procedure for right colon cancer is complete mesocolic excision. Whether preventive extended lymph node dissection for colon cancer located in the hepatic flexure or right transverse colon should be performed remains controversial because the safety and effectiveness of the operation have not been proven, and infrapyloric lymph nodes (No. 206) and lymph nodes in the greater curvature of the stomach (No. 204) have not been strictly defined and distinguished as surgical indicators in previous studies.
To analyze the metastatic status of infrapyloric lymph nodes and lymph nodes of the greater curvature of the stomach and perioperative complications and systematically evaluate the feasibility and safety of laparoscopic extended right colectomy using prospective data collected retrospectively.
The study was a clinical study. Twenty patients with colon cancer who underwent laparoscopic extended right colon resection in our hospital from June 2020 to May 2021 were included.
Among the patients who underwent extended right colon resection, there were no intraoperative complications or conversion to laparotomy; 2 patients had gastrocolic ligament lymph node metastasis, and 5 patients had postoperative complications. The patients with postoperative complications received conservative treatment.
Laparoscopic extended right colon resection is safe. However, malignant tumors located in the liver flexure or the right-side transverse colon are more likely to metastasize to the gastrocolic ligament lymph nodes, and notably, the incidence of gastroparesis was high. The number of patients was small, and the follow-up time was short. It is necessary to further increase the sample size to evaluate the No. 204 and No. 206 lymph node metastasis rates and the long-term survival impact.
Core Tip: Whether laparoscopic extended right colectomy should be performed in patients with malignant tumors located in the hepatic flexure and right-side transverse colon remains controversial mainly because of the lack of an understanding of lymph node metastasis in the gastrocolic ligament and doubts regarding the safety of the operation. No prospective studies assessed the possibility and safety of laparoscopic extended right colon resection. Although the sample size in this article was small, the cases were strictly screened and had a certain degree of representativeness, which can provide some insight to surgeons.
- Citation: Zheng HD, Xu JH, Liu YR, Sun YF. Analysis of 20 patients with laparoscopic extended right colectomy. World J Clin Cases 2022; 10(2): 528-537
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/528.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.528
Colorectal cancer (CRC) is the second leading cause of cancer-related death[1]. Studies have shown that the survival rate of patients with right colon cancer is significantly lower than that of patients with colorectal malignancies in other locations[2]. Most colorectal surgeons consider complete mesocolic excision (CME) the standard surgery for right-side colon cancer, and CME can improve the long-term survival rate of patients. The principles are as follows: (1) Accurate dissection of the Toldt space and preservation of the colonic membrane; (2) Ligation of the root vessels; and (3) Extended lymph node dissection in tumors located in the liver curve and right half of the transverse colon[3,4]. So-called extended lymph node dissection refers to the removal of the infrapyloric lymph nodes and greater curvature lymph nodes that are 10 cm to 15 cm from the tumor[5]. In 1995, Toyota et al[6] found that 5 cases (2%) of colonic hepatic flexure cancer had infrapyloric lymph node metastasis and advocated that if lymph node metastasis is suspected, the infrapyloric lymph node should be removed. Feng et al[7] showed that the infrapyloric lymph node metastasis rate in colonic hepatic flexure cancer was 9.1%, and the greater gastric curvature lymph node metastasis rate was 7.1%. Near colonic hepatic flexure cancer has the possibility of metastasis to the infrapyloric and greater curvature lymph nodes. Few studies concerning the metastasis of the gastrocolic ligament (infrapyloric lymph nodes and greater curvature lymph nodes) in liver flexure and right-side transverse colon adenocarcinoma have been conducted, and these studies were retrospective with small sample sizes. Most extended operations did not sweep the infrapyloric lymph nodes, resulting in great heterogeneity at baseline. We aimed to analyze the metastasis of gastrocolic ligament lymph nodes and perioperative complications to evaluate the feasibility and safety of laparoscopic extended right colectomy.
This prospective study included 20 patients who underwent laparoscopic extended right colectomy at the Gastrointestinal Surgery Department of The Second Affiliated Hospital of Fujian Medical University from June 2020 to May 2021. The study was approved by the Ethics Committee of The Second Affiliated Hospital of Fujian Medical University.
The inclusion criteria were as follows: (1) Patients aged ≥ 18 years or ≤ 75 years; (2) An ASA score of I-III; (3) Colon adenocarcinoma or high-grade intraepithelial neoplasia pathologically confirmed by preoperative colonoscopy biopsy; (4) A tumor located on the near liver flexure of the colon or the right 1/3 of the transverse colon; (5) The surgical method of extended right hemicolectomy (CME); (6) A preoperative staging assessment using cT2-4aN0M0 or cTanyN+M0; and (7) Elective surgery. The exclusion criteria were as follows: (1) A number of lesions greater than 2; (2) Preoperative staging of cT1N0 or cT4bNany; (3) Distant metastasis or tumor invading the surrounding tissues; (4) History of malignant tumors or history of major abdominal surgery; and (5) Emergency surgery. All operations were performed by the same surgeon, who performed over 3000 Laparoscopic colorectal surgeries.
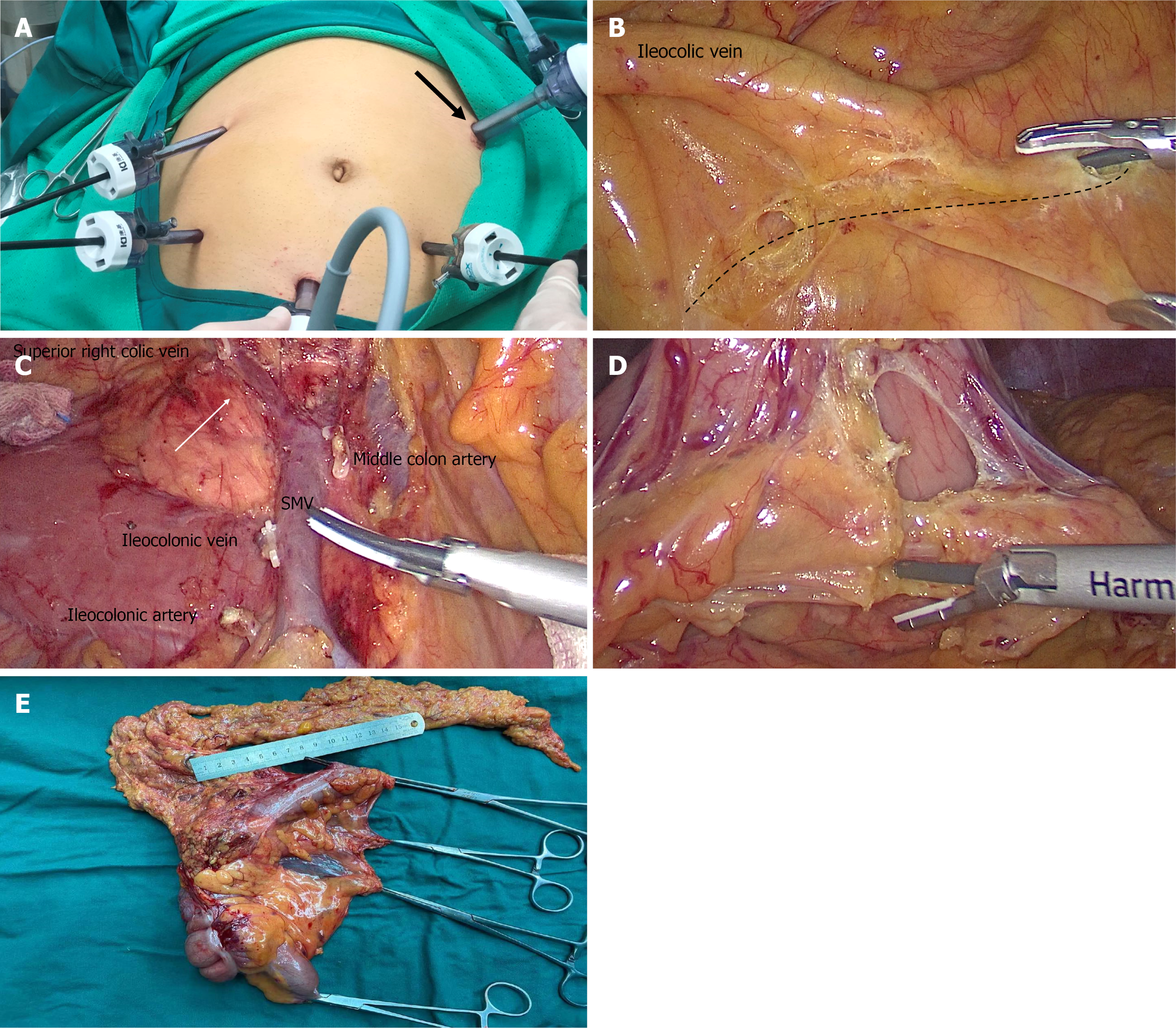
All operations were performed by the same colorectal surgeon, who has experience with 3000 cases of gastrointestinal tumor surgery. The intestinal segment was removed on the basis of CME[8]. We strictly defined the scope of lymph node dissection in No. 204 and No. 206 as follows: No. 206 was defined as lymph nodes in the area surrounding the root of the right gastroepiploic artery (up to its first branch and down to the junction of the right gastroepiploic vein and superior anterior pancreaticoduodenal vein), No. 204 was defined as lymph nodes distributed along the greater curvature of the stomach distal to the first branch of the right gastroepiploic artery. Each patient was placed in the supine position. The five-hole method was used (Figure 1A). (1) The surgical approach was the caudal ventral approach (Figure 1B); (2) The D3 lymph node tissue dissection method was as follows: centered on the left edge of the superior mesenteric artery (SMA) and separated toward the pancreatic neck; the SMA branch was first cut, and then, the superior mesenteric vein (SMV) branch was cut. This approach does not easily damage the SMA branch across the SMV or cause bleeding. Notably, the middle colonic artery had to be ligated and cut at the root (Figure 1C); (3) Radical resection of expanded right colon cancer requires sweeping the lymphatic tissue on the gastro-omental arch 10 cm from the cancer, including infrapyloric lymph nodes (No. 206) and greater curvature lymph nodes (No. 204) (Figure 1D). Care should be taken when separating the infrapyloric blood vessels, which easily causes bleeding and the rapid formation of hematomas, and it can be difficult to find the bleeding points; (4) Intestinal resection and anastomosis were performed as follows: we used an auxiliary incision to remove the intestine, cut along the precut line to remove the specimen, and performed an end-to-side anastomosis of the distal ileum and the distal transverse colon (Figure 1E); and (5) The skin was sutured.
After the specimen was obtained, an attending physician with rich clinical experience cut the lymph node tissue according to the distribution of the blood vessels, including the lymph nodes at the beginning of the ileocolonic artery, right colon artery, and middle colon artery, and separated the No. 206 and No. 204 lymph nodes for the pathological examination.
The complications were described in accordance with the Clavien-Dindo classification[9]. The postoperative complications of the patients were recorded in detail.
The study lasted 11 mo and included 20 patients who strictly met the inclusion criteria. The entire operation process was performed smoothly in 20 patients, and there were no intraoperative conversions to laparotomy or serious intraoperative complications. The median age was 63.5 years (range, 26-75 years), and only one patient was younger than 40 years. The median intraoperative blood loss was 50 mL (range, 20-300 mL). The median operative time in our study was 150 min (range, 170-389 min). The median postoperative anal exhaust time was 3 d (range, 2-6 d). The median time to eat semiliquid food after surgery was 5 d (range, 4-7 d). The median length of hospital stay after surgery was 11.5 d (range, 8-24 d). One case (5%), 16 cases (80%), 3 cases (15%), 9 cases (45%), 7 cases (35%), and 4 cases (20%) had postoperative pathological stages T2, T3, T4, N0, N1, and N2, respectively. The detailed information is shown in Table 1.
| Variable | n (%) |
| Age, median (range) | 63.5 (26–75) |
| Sex (male) | 15 (75) |
| BMI (> 25) | 7 (35) |
| ASA ≤ 2 | 19 (95) |
| Tumor location | |
| Hepatic flexure | 13 (65) |
| Right transverse | 7 (35) |
| Pathology | |
| pT1 | 0 (0) |
| pT2 | 1 (5) |
| pT3 | 16 (80) |
| pT4 | 3 (15) |
| pN0 | 9 (45) |
| pN1 | 7 (35) |
| pN2 | 4 (20) |
| Perineural invasion | 5 (25) |
| Vascular invasion | 8 (40) |
| Defective mismatch repair | 5 (25) |
| Intraoperative complications | 0 (0) |
| Transition to open abdomen | 0 (0) |
In total, 5 (25%) patients had postoperative complications, including 2 cases of delayed gastric emptying (gastroparesis), 2 cases of intestinal obstruction, 1 case of postoperative gastrointestinal bleeding, 1 case of wound infection, 1 case of pancreatic fistula, and 1 case of chylous ascites. One patient had three complications (wound infection, intestinal obstruction, and pancreatic fistula). All patients were cured by conservative treatment. The details are shown in Table 2.
| Variable | n (%) |
| Postoperative complication | 5 (25) |
| Anastomotic leakage | 0 (0) |
| Pancreatic fistula POPF grade | |
| Grade A | 0 (0) |
| Grade B | 1 (5) |
| Grade C | 0 (0) |
| Intestinal obstruction | 2 (10) |
| Chylous ascites | 1 (5) |
| Incision infection | 1 (5) |
| Gastroparesis | 2 (10) |
| Organ infection | 0 (0) |
| Gastrointestinal bleeding | 1 (5) |
| Clavien–Dindo classification | |
| Grade I | 1 (5) |
| Grade II | 5 (25) |
| Grade III and above | 1 (5) |
| Anal exhaust time, median (range) (d) | 3 (2-6) |
| Semiliquid diet, median (range) (d) | 5 (4-7) |
| Length of hospital stay | 11.5 (8-24) |
The number of lymph nodes retrieved and metastases found are shown in Table 2. In total, 11 (55%) patients had lymph node metastasis, and 8 (40%) patients had apical lymph node metastases. The mean ± SD of the number of lymph nodes dissected was 39.3 ± 10.9 nodes, and the median number of metastatic lymph nodes was 1 node (range, 0-28 nodes). The median number of No. 204 lymph nodes was 2 (range, 0-8 nodes), and the median number of No. 206 lymph nodes was 2.5 (range, 0-9 nodes); only 1 patient had lymph node metastasis of No. 206, and 1 patient had lymph node metastasis of No. 204. The details are shown in Table 3.
| Variable | n (%) |
| Total LN yield, mean ± SD | 39.3 ± 10.9 |
| LN metastases, median (range) | 1 (0-28) |
| No. 204 LN yield, median (range) | 2 (0-8) |
| No. 206 LN yield, median (range) | 2.5 (0-9) |
| Apical LN metastases | 8 (40) |
| No. 204 LN metastases | 1 (5) |
| No. 206 LN metastases | 1 (5) |
The detailed information of the patients with No. 204 lymph node or No. 206 lymph node metastasis is shown in Table 4. We found the following pattern: The patients with No. 204 lymph node or No. 206 lymph node metastasis generally had late T and N staging, and apical lymph nodes often had metastases. Moreover, cancer cells can usually be found in the vasculature or nerve tissue, affecting the survival time of patients.
| Patient | Patient 1 | Patient 2 |
| Age (yr) | 69 | 61 |
| Gender | Female | Female |
| BMI | 30.04 | 20.96 |
| Symptom | Abdominal pain | Abdominal pain |
| CEA (ng/mL) | 33.28 | 25.39 |
| ASA score | II | III |
| Location | R | H |
| Pathological type | Ulcerative | Ulcerative |
| Differentiation | M | m-p |
| T stage | T4a | T3 |
| N stage | N2 | N2 |
| Tumor size (cm) | 6.0 × 3.5 | 6.0 × 5.5 |
| Mesocolic LN metastases/mesocolic LN yield (n) | 5/34 | 28/58 |
| Apical LN metastases/apical LN yield (n) | 4/13 | 16/30 |
| No. 204 LN metastases/GCLN yield (n) | 1/2 | 0/2 |
| No. 206 LN metastases/GCLN yield (n) | 0/6 | 3/3 |
| Venous invasion (n) | Yes | Yes |
| Perineural invasion (n) | No | Yes |
| Mismatch repair protein | Expression | Expression |
| Postoperative complications | No | No |
| Chemotherapy method | XELOX | XELOX |
| Relapse | No | Metastasis |
| Mortality | Alive | Death |
CME is currently recognized as a surgical method for right-side colon cancer that can improve lymph node collection and the length of surgical specimens without increasing intraoperative and postoperative complications[9]. Compared with left-side colon carcinoma and rectal carcinoma, the prognosis of right-side colon cancer is worse, which may be the result of inadequate tumor and lymph node resection, especially in the liver flexure and right transverse colon. Tumors often appear as No. 204 and No. 206 lymph node metastases if the lymph node is not cleared, which may increase the possibility of tumor recurrence and reduce the survival rate of patients with right colon cancer[2,4]. Although our study has a small sample size, the inclusion criteria are strict, and currently, similar prospective studies are lacking; thus, this study can provide a good reference for clinicians.
Laparoscopic extended right colectomy is one of the most challenging operations in colorectal surgery due to the difficulty in determining the origin of the middle colon artery because of the complex anatomy near the pancreatic neck[11]. The correct identification and cutting of the middle colon artery and careful separation of the inferior pylorus vessels are critical for the safe implementation of laparoscopic extended right hemicolectomy, representing a serious challenge for surgeons[12]. Therefore, the safety of laparoscopic extended right hemicolectomy is still controversial, but most studies suggest that the procedure is safe and feasible. Zhao et al[13] considered that laparoscopic extended right hemicolectomy was a technically feasible and safe surgical method and could obtain the same short-term oncological results as open surgery. In their study, 9 cases (9/220, 4.1%) were converted to open abdomen, 4 cases (4/9, 44.4%) were T4a, and two cases (2/9, 22.2%) had massive bleeding during the process of stripping the right gastrocnemic artery root, which is less than 14% to 19% of the other randomized control study[14,15]. However, the above study did not clarify the lymph node metastasis incidence of No. 204 and No. 206 and only focused on a comparison of laparoscopic and open surgery.
We observed some characteristics of the postoperative complications in our study. The incidence rate of gastroparesis was 10% in the present study, which is significantly higher than that of right colectomy without clearing the lymph nodes of the gastrocolic ligament (10% vs 0.3%)[16]. It is generally believed that 30%-50% may cause gastroparesis in diabetic patients. However, our patients with gastroparesis had normal blood sugar[17]. We considered that the occurrence of gastroparesis was related to the patients who underwent gastrocolic lymph node dissection. Therefore, additional research is needed to determine the best surgical indications and avoid unnecessary and futile gastrocolic ligament lymph node dissection in the future. Few studies examined the causes of gastroparesis after extended right hemicolectomy. We suggest that the ultrasound knife burns the stomach during the removal of the omental blood vessels, resulting in decreased gastric motility. You et al[18] suggested that preserving the right gastroepiploic vessels can reduce the incidence of gastroparesis; however, in this case, No. 206 lymph nodes cannot be completely cleared. According to our clinical experience, when dissociating from the arch, we should cut the blood vessels 0.5 cm away from the great curvature of the stomach when dissociating on the arch to avoid burning the stomach and causing gastroparesis. The other complications seem to be related to colectomy rather than gastrocolic ligament resection. Some authors[4] observed gastric perforation after extended right hemicolectomy, which may be related to gastrocolic ligament resection, and some patients had a dissecting thoracic aorta aneurysm, which may be due to an impaired blood supply to the main abdominal cavity. In our study, there were no intraoperative complications or conversion to laparotomy. The reasons may be that this study had a small sample because the inclusion criteria were strict and the operation was performed by the same gastrointestinal oncologist with extensive laparoscopic experience. In conclusion, we believe that laparoscopic extended right colectomy is safe but should be performed by skilled surgeons.
The probability of metastasis of gastrocolic ligament lymph nodes was 10% in our study. This result is similar to previous studies showing that the probability of lymph node metastasis of the gastrocolic ligament is relatively low. We found that the probability of lymph node metastasis of the gastrocolic ligament with tumors located in the hepatic flexure or right-side transverse colon is significantly higher than that of colon cancer in other locations. Therefore, tumors located in high-risk locations should undergo extended right hemicolectomy combined with infrapyloric and greater curvature lymph node dissection[6]. The main risk factors for gastrocolic ligament lymph node metastasis in right colon cancer are nerve invasion, pN2 stage, carcinoembryonic antigen, poor differentiation and apical lymph node metastasis[4,16]. We can further confirm this conclusion given the data shown in Table 4. These factors are high-risk and lead to a poor prognosis in colon cancer patients, indicating that the occurrence of gastrocolic ligament lymph node metastasis is closely related to the patient survival rate.
Whether lymph node metastasis of the gastrocolic ligament is regional lymph node metastasis or distant metastasis remains controversial[4,19]. Based on the limited available data, it is difficult to draw a conclusion. However, this does not affect the need for postoperative chemotherapy in some patients. Twelve patients received regular adjuvant chemotherapy, oxaliplatin combined with capecitabine. One patient died of liver metastasis and pulmonary infection 7 mo after the operation. The TNM stage of the patient was T3N2M0, with lymph node metastasis of the gastrocolic ligament and vascular and nerve invasion, indicating a poor prognosis. The remaining patients had no recurrence or metastasis during the follow-up. Notably, Saluja et al[20] showed that there was no significant difference in survival between young patients and elderly patients. To date, few studies conducted a survival analysis of patients with laparoscopic extended right colectomy. The short-term efficacy and long-term prognosis still require further investigation.
This study demonstrated the rate of gastrocolic ligament lymph nodes located in the liver flexure or the right transverse colon and comprehensively evaluated the safety, feasibility, and short-term efficacy of lymph node dissection in this area, providing important clinical significance; however, there are still several limitations. First, this article reports a single-center analysis based on a clinical study. The inclusion and exclusion criteria were strict, and the length of time was short, resulting in a small sample size, which cannot reach the sample size required for calculation. Second, due to the current short follow-up time, the long-term prognosis of the patients cannot be assessed. A multicenter clinical study investigating this subject in the future is expected to further confirm the results we discussed and evaluate the long-term prognosis of patients.
Malignant tumors located in the hepatic flexure or right transverse colon have the possibility of gastrocolic ligament lymph node metastasis, and there are indications for laparoscopic extended right colectomy. The surgical approach is safe but could notably increase the incidence of gastroparesis. However, the prognostic effect still needs further analysis.
Whether laparoscopic extended right colectomy is necessary for colon cancer with tumor located in hepatic flexure and right transverse colon is still controversial.
It is of great concern whether laparoscopic extended right colectomy is necessary for tumors located in the hepatic flexure and the right transverse colon. Currently, there is an urgent need to understand the law of lymph nodes of the gastrocolic ligament and the safety of the operation.
This study aimed to study the necessity and safety of laparoscopic extended right colectomy.
This is a clinical study of 20 patients who underwent laparoscopic extended right colectomy. This article describes the surgical technique of laparoscopic extended right colectomy and the perioperative information of patients.
There were no intraoperative complications and conversion to laparotomy in 20 patients. Lymph node metastasis of gastrocolic ligament occurred in 10% of patients, and postoperative complications occurred in 5 patients.
Laparoscopic extended right colectomy is safe, but it may significantly increase the risk of postoperative gastroparesis.
This study is expected to increase the sample size and follow-up time.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Sachdeva S S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Doubeni CA, Corley DA, Jensen CD, Schottinger JE, Lee JK, Ghai NR, Levin TR, Zhao WK, Saia CA, Wainwright JV, Mehta SJ, Selby K, Doria-Rose VP, Zauber AG, Fletcher RH, Weiss NS. The effect of using fecal testing after a negative sigmoidoscopy on the risk of death from colorectal cancer. J Med Screen. 2021;28:140-147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Nakagawa-Senda H, Hori M, Matsuda T, Ito H. Prognostic impact of tumor location in colon cancer: the Monitoring of Cancer Incidence in Japan (MCIJ) project. BMC Cancer. 2019;19:431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Søndenaa K, Quirke P, Hohenberger W, Sugihara K, Kobayashi H, Kessler H, Brown G, Tudyka V, D'Hoore A, Kennedy RH, West NP, Kim SH, Heald R, Storli KE, Nesbakken A, Moran B. The rationale behind complete mesocolic excision (CME) and a central vascular ligation for colon cancer in open and laparoscopic surgery : proceedings of a consensus conference. Int J Colorectal Dis. 2014;29:419-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 164] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 4. | Olmi S, Oldani A, Cesana G, Ciccarese F, Uccelli M, Giorgi R, Villa R, Maria De Carli S. Surgical Outcomes of Laparoscopic Right Colectomy with Complete Mesocolic Excision. JSLS. 2020;24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Bertelsen CA, Bols B, Ingeholm P, Jansen JE, Jepsen LV, Kristensen B, Neuenschwander AU, Gögenur I. Lymph node metastases in the gastrocolic ligament in patients with colon cancer. Dis Colon Rectum. 2014;57:839-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Toyota S, Ohta H, Anazawa S. Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum. 1995;38:705-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 142] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 7. | Feng B, Ling TL, Lu AG, Wang ML, Ma JJ, Li JW, Zang L, Sun J, Zheng MH. Completely medial vs hybrid medial approach for laparoscopic complete mesocolic excision in right hemicolon cancer. Surg Endosc. 2014;28:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1104] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 9. | Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18532] [Cited by in RCA: 24805] [Article Influence: 1181.2] [Reference Citation Analysis (0)] |
| 10. | Di Buono G, Buscemi S, Cocorullo G, Sorce V, Amato G, Bonventre G, Maienza E, Galia M, Gulotta L, Romano G, Agrusa A. Feasibility and Safety of Laparoscopic Complete Mesocolic Excision (CME) for Right-sided Colon Cancer: Short-term Outcomes. A Randomized Clinical Study. Ann Surg. 2021;274:57-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 11. | Chew SS, Adams WJ. Laparoscopic hand-assisted extended right hemicolectomy for cancer management. Surg Endosc. 2007;21:1654-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Koh FH, Tan KK. A Safe Method for Middle Colic Dissection and Ligation at its Origin in a Laparoscopic Extended Right Hemicolectomy. Ann Surg Oncol. 2016;23:665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Zhao LY, Chi P, Ding WX, Huang SR, Zhang SF, Pan K, Hu YF, Liu H, Li GX. Laparoscopic vs open extended right hemicolectomy for colon cancer. World J Gastroenterol. 2014;20:7926-7932. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | 2017 and 2015 European Society of Coloproctology (ESCP) collaborating groups. The impact of conversion on the risk of major complication following laparoscopic colonic surgery: an international, multicentre prospective audit. Colorectal Dis. 2018;20 Suppl 6:69-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Gorgun E, Benlice C, Abbas MA, Stocchi L, Remzi FH. Conversion in laparoscopic colorectal surgery: Are short-term outcomes worse than with open surgery? Tech Coloproctol. 2016;20:845-851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Huang S, Wang X, Deng Y, Jiang W, Huang Y, Chi P. Gastrocolic Ligament Lymph Node Dissection for Transverse Colon and Hepatic Flexure Colon Cancer: Risk of Nodal Metastases and Complications in a Large-Volume Center. J Gastrointest Surg. 2020;24:2658-2660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | De Block CE, De Leeuw IH, Pelckmans PA, Callens D, Máday E, Van Gaal LF. Delayed gastric emptying and gastric autoimmunity in type 1 diabetes. Diabetes Care. 2002;25:912-917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | You XL, Lian YJ, Wu J, Wang YJ, Dai JW, Zhao XJ, Cheng ZY, Huang CJ, Li WQ, Zhou Y. [Clinical study on preserving right gastroepiploic vein during laparoscopic right hemicolectomy]. Zhonghua Wei Chang Wai Ke Za Zhi. 2020;23:1164-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | Uematsu D, Akiyama G, Sugihara T, Magishi A, Yamaguchi T, Sano T. Laparoscopic radical lymph node dissection for advanced colon cancer close to the hepatic flexure. Asian J Endosc Surg. 2017;10:23-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Saluja SS, Manipadam JM, Mishra PK, Sachdeva S, Solanki N, Shah H. Young onset colorectal cancer: How does it differ from its older counterpart? Indian J Cancer. 2014;51:565-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |