Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.477
Peer-review started: July 21, 2021
First decision: October 16, 2021
Revised: October 22, 2021
Accepted: December 10, 2021
Article in press: December 10, 2021
Published online: January 14, 2022
Processing time: 175 Days and 1.6 Hours
Supra- and infratentorial acute epidural hematoma (SIEDH) is a common posterior cranial fossa epidural hematoma located at the inner surface of the squamous part of the occipital bone (SOB). Traditionally, surgical treatment of the SIEDH requires a combined supra-infratentorial craniotomy.
To analyze the morphological characteristics of the SOB and introduce a single supratentorial craniotomy for SIEDH.
Skull computed tomography (CT) scan data from 32 adult patients were collected from January 1, 2019 to January 31, 2020. On the median sagittal plane of the CT scan, the angle of the SOB (ASOB) was defined by two lines: Line A was defined from the lambdoid suture (LambS) to the external occipital protuberance (EOP), while line B was defined from the EOP to the posterior edge of the foramen magnum (poFM). The operative angle for the SIEDH (OAS) from the supra- to infratentorial epidural space was determined by two lines: The first line passes from the midpoint between the EOP and the LambS to the poFM, while the second line passes from the EOP to the poFM. The ASOB and OAS were measured and analyzed.
Based on the anatomical study, a single supratentorial craniotomy was performed in 8 patients with SIEDH. The procedure and the results of the modified surgical method were demonstrated in detail. For males, the ASOB was 118.4 ± 4.7 and the OAS was 15.1 ± 1.8; for females, the ASOB was 130.4 ± 5.1 and the OAS was 12.8 ± 2.0. There were significant differences between males and females both in ASOB and OAS. The smaller the ASOB was, the larger the OAS was. The bone flaps in 8 patients were designed above the transverse sinus intraoperatively, and the SIEDH was completely removed without suboccipital craniotomy. The SOB does not present as a single straight plane but bends at an angle around the EOP and the superior nuchal lines. The OAS was negatively correlated with the ASOB.
The single supratentorial craniotomy for SIEDH is reliable and effective.
Core Tip: Traditionally, surgical treatment of a supra- and infratentorial acute epidural hematoma (SIEDH) requires a combined supra-infratentorial craniotomy. We analyzed the morphological characteristics of the squamous part of the occipital bone (SOB) and found that the operative angle for the SIEDH was negatively correlated with the angle of the SOB. These morphological characteristics of the SOB make it possible to treat SIEDH with a single supratentorial craniotomy. Based on the above findings, we used a single supratentorial craniotomy to treat SIEDH, and achieved satisfactory results.
- Citation: Li RC, Guo SW, Liang C. Modified surgical method of supra- and infratentorial epidural hematoma and the related anatomical study of the squamous part of the occipital bone. World J Clin Cases 2022; 10(2): 477-484
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/477.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.477
Supra- and infratentorial acute epidural hematoma (SIEDH) is a common posterior cranial fossa epidural hematoma located at the inner surface of the squamous part of the occipital bone (SOB)[1-3]. Most SIEDHs are caused by direct violence to the occipital bone due to traffic accidents and falls[4-6]. The traditional surgical method requires a tedious combined supra-infratentorial craniotomy to evacuate the SIEDH[2,7,8]. However, the SOB does not present as a single straight plane, but bends at an angle around the external occipital protuberance (EOP) and the superior nuchal lines, which divide the SOB into the supra-and infratentorial areas, respectively[9]. As the angle of the SOB (ASOB) is less than 180, there is an operative angle for the SIEDH (OAS) from the supra- to infratentorial epidural space by a single supratentorial craniotomy.
In this study, the ASOB and the OAS were analyzed quantitatively. An illustrative case example is presented to demonstrate the technique nuances of the modified surgical method.
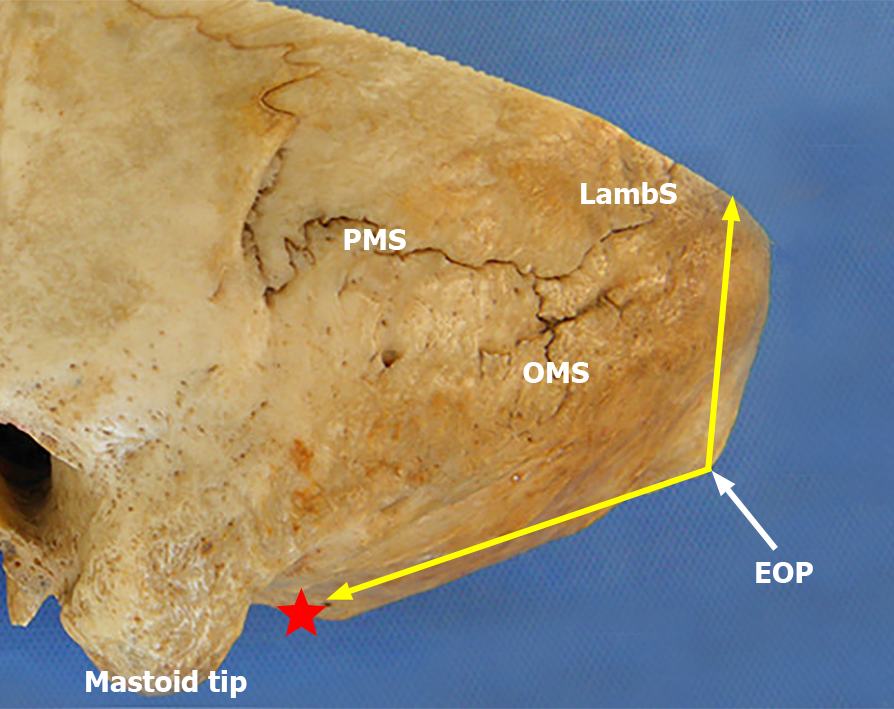
The SOB is located above the posterior edge of the foramen magnum and articulates with the parietal bone at the lambdoid suture (LambS). The EOP, with the superior nuchal lines radiated laterally from it, is situated at the central part of the external surface of the SOB and divides the SOB into superior and inferior parts. The two parts form an angle with the EOP at the vertex (schematic representation in Figure 1).
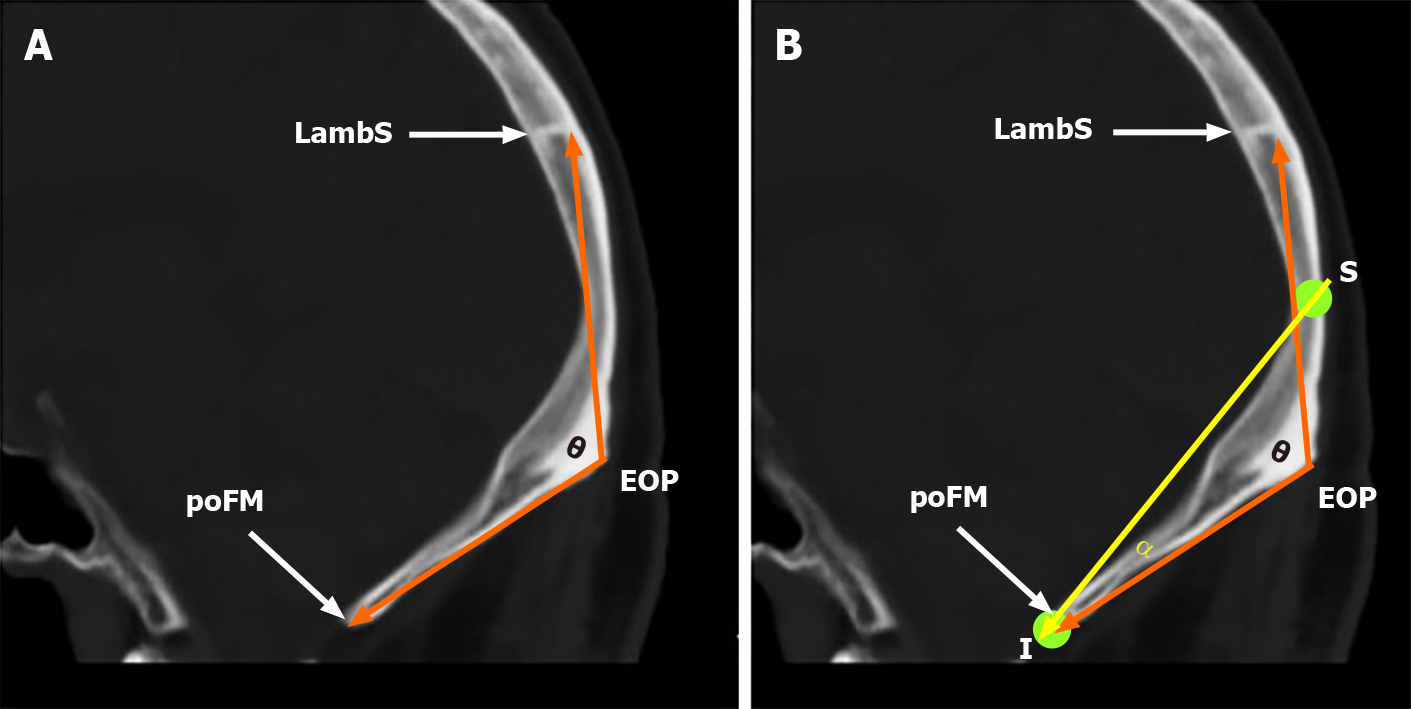
On the median sagittal plane of the computed tomography (CT) scan, the ASOB was defined by two lines: One is from the EOP to the LambS, and the other is from the EOP to the posterior edge of the foramen magnum (poFM) (Figure 2A).
On the median sagittal plane of the CT scan, an angle was defined to analyze the OAS quantitatively. The OAS was determined by two intersecting lines with the vertex located at the poFM. The first line passes from the midpoint between the EOP and the LambS to the poFM, while the second line passes from the EOP to the poFM (Figure 2B). Theoretically, the OAS can represent the surgical freedom for clearance of the SIEDH from the supra- to infratentorial epidural space by a single supratentorial craniotomy. Mathematically, the greater the OAS is, the bigger the operative corridor is.
The skull CT scans of 32 adult patients (16 males and 16 females, aged from 18 to 65 years) were collected in the Neurosurgical Department of Xi’an Jiaotong University from January 1, 2019 to January 31, 2020. These patients included 22 cases of intracranial aneurysms and 8 cases of acoustic schwannomas. The ASOB and OAS were measured on the median sagittal plane of the CT scans and the data were analyzed statistically.
A total of 8 patients with SIEDH were surgically treated from July 1, 2017 to March 31, 2020. These patients consisted of 6 males and 2 females, aged from 23 to 49 years (mean 32.5 ± 10.5 years). Seven cases were admitted following traffic accidents and 1 case following a fall injury. Three of these patients had occipital and frontal lobe contusion and laceration. The admission Glasgow Coma Score (GCS) was 9 points in 3 cases, 10 points in 4 cases and 11 points in 1 case (median 10 points).
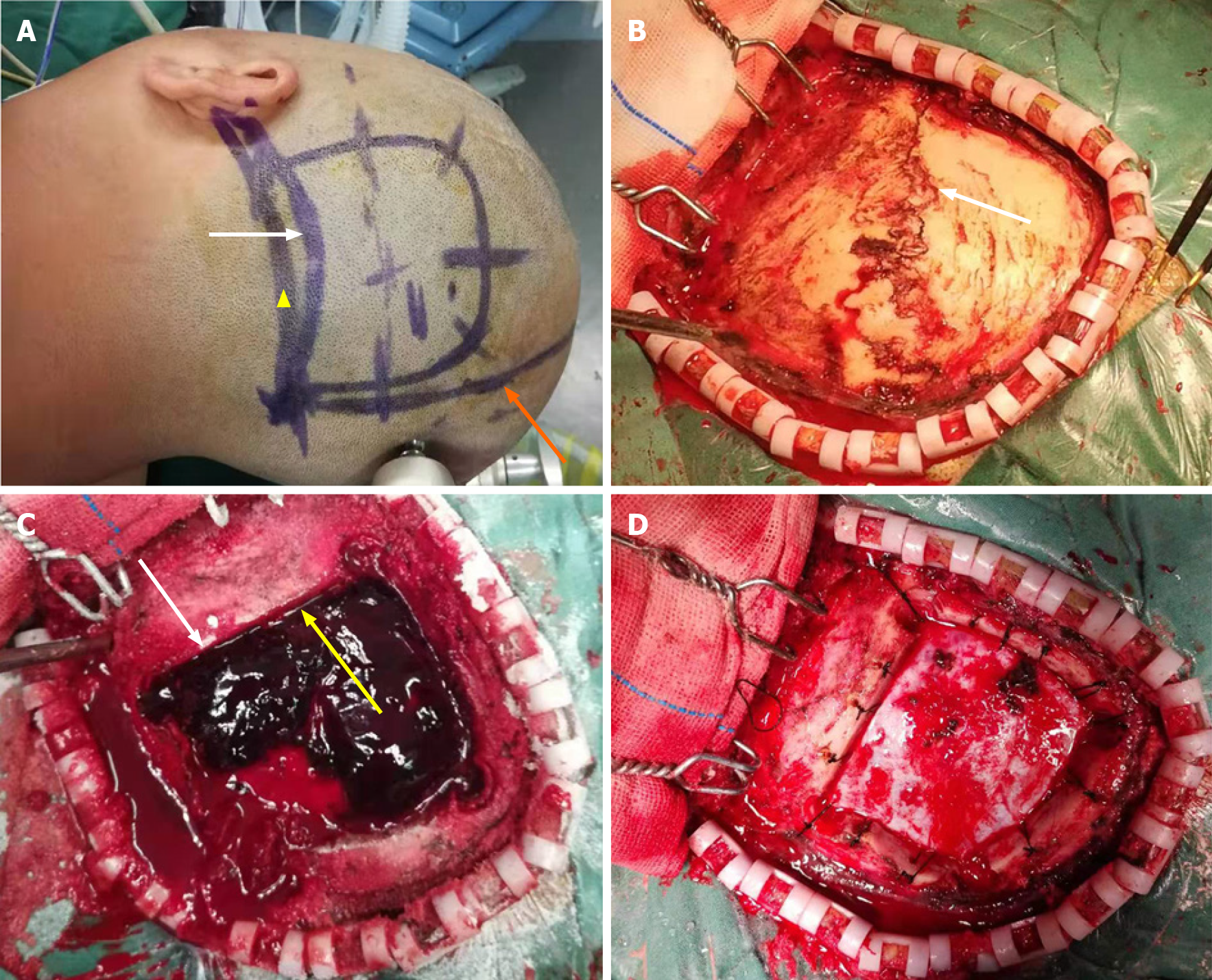
After general anesthesia, the patients were positioned laterally with the head fixed by a Mayfield head frame (Integra LifeSciences Corporation, Cincinnati, OH, United States). According to the location of the hematoma, a unilateral occipital skin flap was incised and the boundary of the bone flap was defined by 4 Lines: The midline, the lateral edge of the hematoma, the upper edge of the hematoma and the lower margin of the transverse sinus (Figure 3). Four bony holes were drilled using the Medtronic high-speed drill (Medtronic, Minneapolis, MN, United States) at the corners of the bone flap, and a supratentorial craniotomy was completed. Subsequently, the supratentorial part of the SIEDH was gradually removed by suction and forceps. When the dura mater was exposed, the bleeding arteries on the dura were immediately electrocoagulated. In the transverse sinus region, the hematoma was carefully evacuated and a gelatin sponge was used to stop the bleeding from the sinus. The inferior part of the SIEDH was then explored and evacuated. Finally, the dura mater was carefully suspended at the edge of the craniectomy and the bone flap was fixed in situ.
The Shapiro-Wilk test was used to analyze the normality of the data, and Levene’s test was used to analyze the homogeneity of variance. The t-test was used for comparisons between the two groups when the data were in accordance with normal distribution and homogeneity of variance, otherwise the Rank sum test was used. A two-tailed P < 0.05 indicated statistical significance. All statistics were performed with R version 4.0.2.
The ASOB of male patients was smaller than that of female patients (118.4 ± 4.7 vs 130.4 ± 5.1), while the OAS of males was greater than that of females (15.1 ± 1.8 vs 12.8 ± 2.0). These data are shown in Table 1. These results indicated that the smaller the ASOB was, the greater the OAS was.
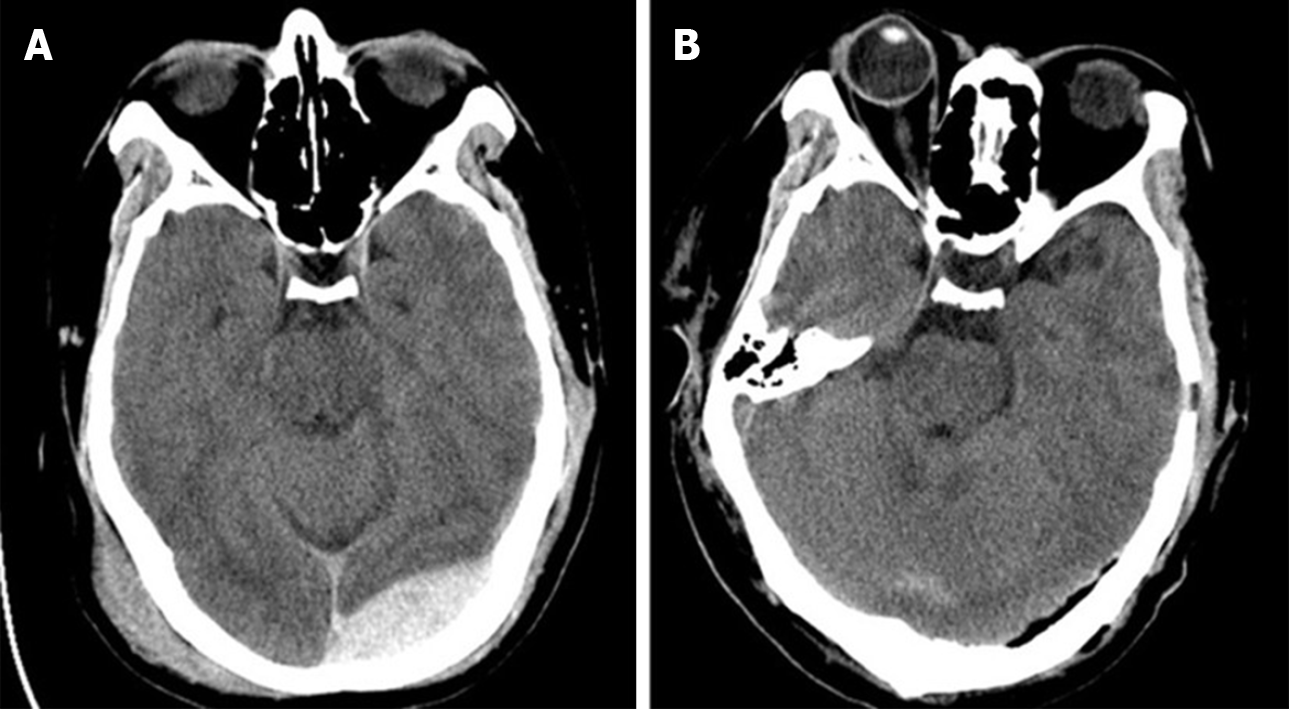
A skull CT examination was performed within 24 h postoperatively. The SIEDH was totally removed in all 8 cases. The postoperative GCS scores were 10 in 4 cases, 11 in 2 cases, 12 in 1 case and 13 in 1 case 72 h after surgery. The median score was 10.5, which was significantly higher than that before surgery (Table 2). Postoperatively, one patient developed pneumonia which was cured by antibiotic treatment within 2 wk. Intracranial infection, subcutaneous effusion and cerebrospinal fluid leakage were not observed.
A 29-year-old man was admitted to hospital 3 h after a traffic accident. The admission GCS score was 10. The CT examination revealed a left SIEDH and scalp hematoma (Figure 4A). Surgical treatment was carried out according to the method described above. Intraoperatively, a linear fracture of the occipital bone extended from the LambS to the mastoid (Figure 3B), which was the source of the epidural hematoma. The hematoma covering the transverse sinus area separated the dura from the inner surface of the skull, which created a surgical corridor from supratentorial to infratentorial (Figure 3C). The hematoma was completely cleared, which was confirmed by a postoperative CT scan (Figures 3D and 4B). The bone flap was perfectly reset and fixed without any obvious bone defects (Figure 4B).
The SIEDH, which traverses the transverse sinus from the supa- to inferior tentorial, represents 11%-64% of all posterior fossa epidural hematomas[2,3,6]. Due to potential severe brain edema due to compression on the transverse sinus by the hematoma, some scholars have suggested aggressive surgical treatment even if the hematoma volume is small[6-8]. Traditionally, a combined supra-inferior craniotomy was recommended. The supratentorial bone flap was reset at the end of surgery, while the infratentorial bone, in the suboccipital area, was removed. The purpose of the traditional method was to maximize exposure of the hematoma and thoroughly remove it[8,10]. However, the combined supra-inferior craniotomy has the following disadvantages: Firstly, it requires the cutting of multi-layer muscles in the suboccipital area, which can be time-consuming and increase blood loss; secondly, a suboccipital craniotomy is often accompanied by a subsequent large bone defect[11]. To avoid a large bone defect in the suboccipital area, Wang and Guoping[7] recommended a single supratentorial craniotomy to remove the SIEDH. Their research showed that this technique led to efficient total evacuation of the SIEDH.
Therefore, based on the anatomical characteristics of the SOB, this study theoretically demonstrated the feasibility of single supratentorial craniotomy in the treatment of SIEDH.
According to Rhoton's research, the occipital bone is divided into a SOB part located above and behind the foramen magnum, a basal part situated in front of the foramen magnum, and paired condylar parts located lateral to the foramen magnum[9,12]. The SOB extends from the foramen magnum inferiorly to the LambS superiorly. The EOP and the superior nuchal lines divide the SOB into superior and inferior parts which locate up and down to the transverse sinus, respectively. The inferior part of the SOB is also called the suboccipital area with a rough outer surface which serves as the site of attachment of numerous muscles including the trapezius, sternocleidomastoid, splenius capitis and semispinalis muscles, etc.[9].
In this study, we found that the superior and inferior parts of the SOB were not located in one plane but were connected at an intersection angle (ASOB). The ASOB in males was smaller than that in females (118.4 ± 4.7 vs 130.4 ± 5.1). As the ASOB was less than 180 in both males and females, when elevating the dura, there was an operative corridor for evacuation of the SIEDH from the supratentorial to infratentorial epidural space in a single supratentorial craniotomy. The OAS was used to analyze this operative corridor quantitatively and the study revealed that the OAS in males was greater than that in females (15.1 ± 1.8 vs 12.8 ± 2.0). These results indicated that the smaller the ASOB is, the greater the OAS is. These anatomical morphological characteristics are extremely important for modification of the surgical method.
Intraoperatively, we performed a single craniotomy above the transverse sinus. After the supratentorial part of the SIEDH had been cleared, the dura of the transverse sinus was often found to be peeled off from the inner surface of the skull. In the 8 cases included in this study, all the infratentorial part of the SIEDHs were explored and removed completely. This modified surgical method of the single supratentorial craniotomy omitted the tedious steps of infratentorial craniotomy and its complications were also avoided.
However, the number of cases in this study was relatively small, and there were no cases with transection or laceration of the transverse sinus. In such situations, the combination of supra-inferior tentorial craniotomy should be performed to control the abundant bleeding through a greater range of exposure[13].
The SOB does not present as a single straight plane but bends at an angle around the EOP and the superior nuchal lines, and the smaller the ASOB was, the larger the OAS was. These morphological characteristics of the SOB make it possible to evacuate the SIEDH from the supra- to infratentorial epidural space by a single supratentorial craniotomy.
Traditional surgical treatment of the supra- and infratentorial acute epidural hematoma (SIEDH) requires a combined supra-infratentorial craniotomy.
To modify the surgery method according to the results of anatomical research.
To analyze the morphological characteristics of the squamous part of the occipital bone (SOB) and introduce a single supratentorial craniotomy for SIEDH.
Skull computed tomography scan data from 32 adult patients were collected. The angle of the SOB (ASOB) and the operative angle for the SIEDH (OAS) were measured and analyzed.
For males, the ASOB was 118.4 ± 4.7 and the OAS was 15.1 ± 1.8; for females, the ASOB was 130.4 ± 5.1 and the OAS was 12.8 ± 2.0. The smaller the ASOB was, the larger the OAS was. Based on the anatomical study, a single supratentorial craniotomy was performed in 8 patients with SIEDH, and the SIEDH was completely removed.
The single supratentorial craniotomy for SIEDH is reliable and effective.
It is hoped that the results of this study can improve the efficiency of surgical treatment of SIEDH.
We thank Professor Wang Y, the Department of Anatomy of Medical College of Xi’an Jiaotong University, for providing radiological data for this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Soliman MAR S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Karasu A, Sabanci PA, Izgi N, Imer M, Sencer A, Cansever T, Canbolat A. Traumatic epidural hematomas of the posterior cranial fossa. Surg Neurol. 2008;69:247-51; dicussion 251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Aji YK, Apriawan T, Bajamal AH. Traumatic Supra- and Infra-tentorial Extradural Hematoma: Case Series and Literature Review. Asian J Neurosurg. 2018;13:453-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Kırcelli A, Özel Ö, Can H, Sarı R, Cansever T, Elmacı İ. Is the presence of linear fracture a predictor of delayed posterior fossa epidural hematoma? Ulus Travma Acil Cerrahi Derg. 2016;22:355-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Winter RC. Posterior Fossa Epidural Hematoma. Pediatr Emerg Care. 2015;31:808-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Koç RK, Paşaoğlu A, Menkü A, Oktem S, Meral M. Extradural hematoma of the posterior cranial fossa. Neurosurg Rev. 1998;21:52-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Malik NK, Makhdoomi R, Indira B, Shankar S, Sastry K. Posterior fossa extradural hematoma: our experience and review of the literature. Surg Neurol. 2007;68:155-8; discussion 158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Xiaoyu W, Guoping L. Surgical treatment of supra- and infratentorial epidural hematoma. Turk Neurosurg. 2013;23:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Nasi D, Iaccarino C, Romano A, De Bonis P, Farneti M, Servadei F, Ghadirpour R. Surgical management of traumatic supra and infratentorial extradural hematomas: our experience and systematic literature review. Neurosurg Rev. 2020;43:893-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Rhoton AL Jr. The far-lateral approach and its transcondylar, supracondylar, and paracondylar extensions. Neurosurgery. 2000;47:S195-S209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 146] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Jang JW, Lee JK, Seo BR, Kim SH. Traumatic epidural haematoma of the posterior cranial fossa. Br J Neurosurg. 2011;25:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Kobayashi T, Miyakoshi N, Abe T, Kikuchi K, Abe E, Shimada Y. Hydrocephalus after foramen magnum decompression for Chiari I malformation successfully treated with the aspiration of pseudomeningocele: a case report. J Med Case Rep. 2019;13:243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Rhoton AL Jr. The foramen magnum. Neurosurgery. 2000;47:S155-S193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 61] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Hayashi T, Kameyama M, Imaizumi S, Kamii H, Onuma T. Acute epidural hematoma of the posterior fossa--cases of acute clinical deterioration. Am J Emerg Med. 2007;25:989-995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |