Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.397
Peer-review started: February 21, 2021
First decision: July 18, 2021
Revised: July 20, 2021
Accepted: December 9, 2021
Article in press: December 9, 2021
Published online: January 14, 2022
Processing time: 324 Days and 17.3 Hours
Muscle fatigue is a problem in rehabilitation, particularly in elderlies and patients with motor neuron diseases. There are high contradictions in the effectiveness of the used methods to decrease muscle fatigue during rehabilitation. They mainly concentrate on increasing rest periods, decreasing training load, or using an ascending intensity of manner of exercise. The training should focus on the newly discovered sensory system of muscle fatigue because of the important role of the sensory system in driving the motor system. Thus, this editorial provides insight on using proprioceptive training to enhance the sensory system of muscle fatigue.
Core Tip: Muscle fatigue is a major problem in rehabilitation. This editorial suggests the use of proprioceptive training in the management of muscle fatigue because it directly trains the sensory system of muscle fatigue which is the proprioceptors. This will enable the body to sense muscle fatigue and well respond to it. In addition, proprioceptive training can normalize and increase the firing rate of motor neurons through the renormalization of presynaptic inhibition and Ia muscle afferents. This could assist in increasing the number of calcium ions into the sarcoplasmic reticulum and skeletal muscles.
- Citation: Mohamed A. New trends in treatment of muscle fatigue throughout rehabilitation of elderlies with motor neuron diseases. World J Clin Cases 2022; 10(2): 397-400
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/397.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.397
Muscle fatigue is considered one of the most common problems that can decrease the effectiveness of any rehabilitation program, particularly in elderlies[1] and patients with motor neuron diseases (MNDs)[2]. Muscle fatigue in elderlies and MNDs mainly arises because of long-standing abnormalities in the neuromuscular system. These abnormalities include abnormal signals from α-motor neurons to muscles, abnormal actin-myosin links, abnormal signals from the motor cortex to α-motor neurons, abnormal motor cortex stimulation-contraction coupling in the muscle, abnormal signals from the motor cortex to α-motor neurons, and depletion of adenosine triphosphate (ATP) and calcium ions (Ca+2). Besides, aging causes an alteration in muscle fibers (type I muscle fibers usually change to type II) which raises the incidence of muscle fatigue throughout any physical activity. Also, MNDs cause atrophic alterations with denervation in muscle fibers. Accordingly, elderlies with MNDs usually experience more alterations in muscle fibers because of the blend of aging and MNDs[1,2].
There are high contradictions in the literature on the effectiveness of used methods to decrease muscle fatigue during rehabilitation. Current interventions established to lessen muscle fatigue during the rehabilitation have mainly concentrated on increasing rest periods, decreasing the load during training, or using an ascending manner of exercise intensity as a try to recuperate muscle force to permit more quantity of calcium ions and ATP[3-5]. In contrast, other studies have demonstrated that leveling exercise intensity or gradual increasing of participation in exercise has little effect in decreasing the incidence of muscle fatigue[6,7].
Thus, the treatment of muscle fatigue should be changed to help these patients and decrease the incidence of muscle fatigue. Muscle fatigue is considered a protective mechanism of our body to prevent injury. To initiate this protective mechanism, there are specific receptors in the human body that feel the start of muscle fatigue. These receptors have been demonstrated to include mechanoreceptors and metaboreceptors. Mechanoreceptors have a superior role over metaboreceptors in detecting muscle fatigue. These mechanoreceptors are similar receptors of proprioception. There is strong evidence that proprioception is much less functioning in both elderlies and patients with MNDs, which increases the assumption that decreased mechanoreceptors function and increased incidence of muscle fatigue are closely connected[1,2].
The function and sensitivity of mechanoreceptors can be boosted both morphologically and neurologically by proprioceptive exercise[8-10]. Increasing signals of mechanoreceptors increase α-motor neuron firing rate[8-10]. Thus, it is truthful to assume that including proprioceptive exercise in rehabilitation can decline the incidence of muscle fatigue. The key role of proprioceptive exercise to decrease the incidence of muscle fatigue includes that proprioceptive exercise can decrease the abnormality in the firing rate of motor neurons through the renormalization of presynaptic inhibition and Ia muscle afferents. This normalization of motor neuron firing rates could assist in increasing the number of calcium ions into the sarcoplasmic reticulum and skeletal muscles. This mechanism significantly helps to improve muscle performance and decrease the incidence of muscle fatigue. Also, normalization of α-motoneurons firing rates can increase the acetylcholine amount at the neuromuscular junction to cross the synaptic cleft and leads to depolarization of the muscle cell membrane. This depolarization triggers high numbers of voltage-gated sodium channels over the muscle membrane and causes initiation of the action potential leading to an increase in the number of calcium ions into the sarcoplasmic reticulum and skeletal muscles[1,2].
Another conceivable effect of proprioceptive exercise in decreasing muscle fatigue is that it can improve oxygen supply, oxidative capacity of contracting muscles, and the amount of ATP, which are important to prevent muscle fatigue. Stimulation of skeletal muscle mechanoreceptors, mainly muscle spindles, can increase the heart rate which consequently increases the respiratory rate and oxygen saturation in blood flow. The oxygen utilization by a body organ equals the amount of blood flow timed by the arterial-venous O2 variance (Fick principle). Consequently, increasing arterial-venous O2 variance can enhance the muscle utilization of serum oxygen and its oxidative capacity and cell mitochondrial activity which helps to reduce the rate of muscle fatigue[1,2].
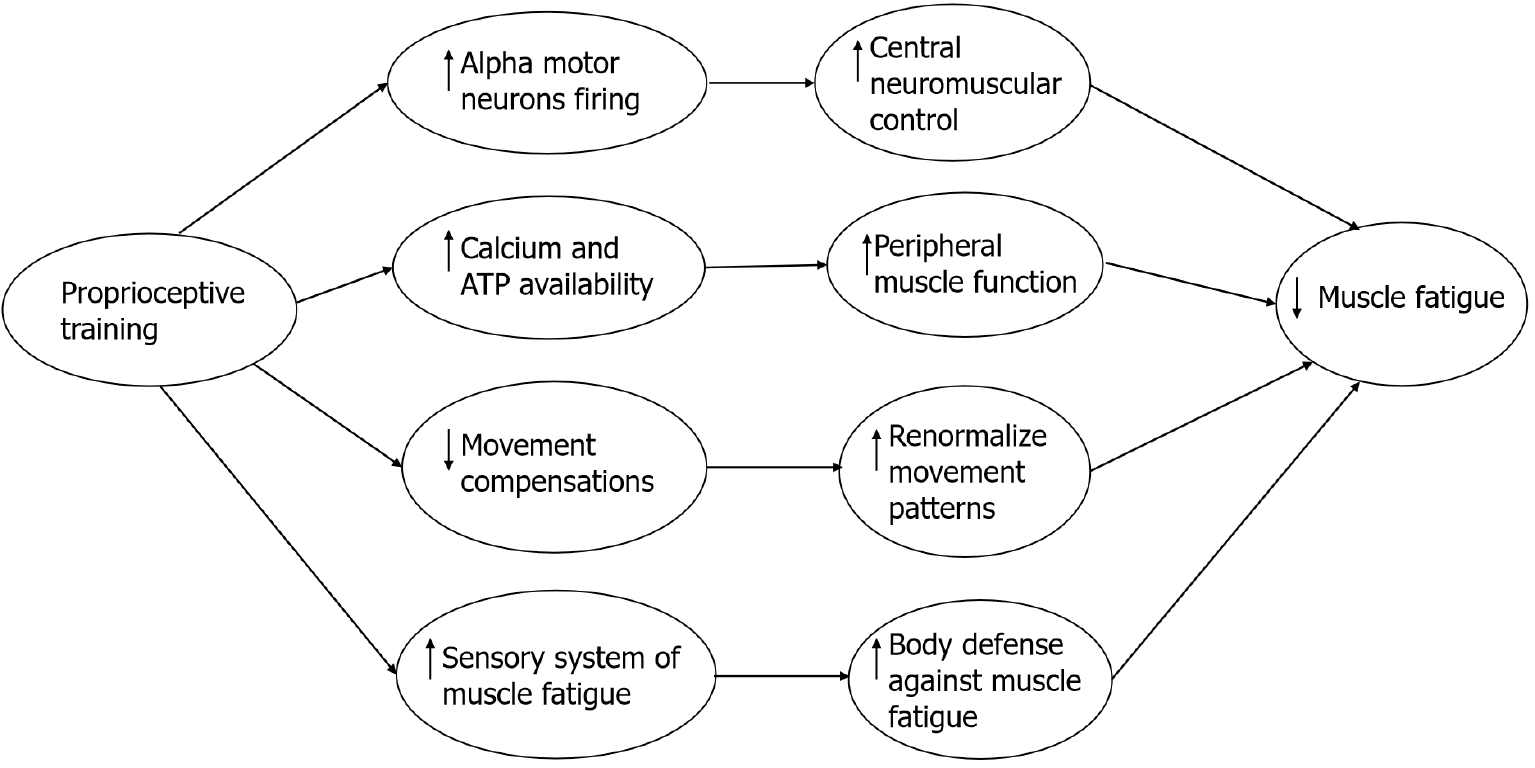
Proprioceptive exercise can also affect the consequences of muscle fatigue in elderlies with MNDs. Muscle fatigue usually leads to movement and gait compensations. Proprioceptive exercise helps to correct any abnormal motor control and yields further coordinated movements with less effort due to its role in driving motor commands. Proprioceptive exercise causes morphological adjustments in muscle spindles themselves through adjusting sensory and proprioceptive signals coming from the working muscle leading to major plastic adjustments in the central nervous system and motor commands[8,10]. The possible mechanisms of enhancing muscle fatigue by proprioceptive training is illustrated in Figure 1.
The treatment of muscle fatigue, particularly in elderlies with MNDs, should be more investigated to produce more decrease in the rate of muscle fatigue. Proprioceptive exercise could be a valuable addition to any rehabilitating method performed to decrease muscle fatigue due to its role in refining α-motor neuron firing rates, elevating calcium ions into neuromuscular junctions, correcting abnormal motor commands, and adjusting movement compensations frequently arising with muscle fatigue in elderlies with MNDs.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Peng BG, Płaszewski M S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR
| 1. | Mohamed AA. Can Proprioceptive Training Enhance Fatigability And Decrease Progression Rate Of Sarcopenia In Seniors? Curr Rheumatol Rev. 2020;16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Mohamed AA. Can Proprioceptive Training Reduce Muscle Fatigue in Patients With Motor Neuron Diseases? Front Physiol. 2019;10:1243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Nogueira DV, Silva SB, de Abreu LC, Valenti VE, Fujimori M, de Mello Monteiro CB, Tortoza C, Ribeiro W, Lazo-Osório RA, Tierra-Criollo CJ. Effect of the rest interval duration between contractions on muscle fatigue. Biomed Eng Online. 2012;11:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Dennett AM, Peiris CL, Shields N, Prendergast LA, Taylor NF. Moderate-intensity exercise reduces fatigue and improves mobility in cancer survivors: a systematic review and meta-regression. J Physiother. 2016;62:68-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 116] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 5. | Wallman KE, Morton AR, Goodman C, Grove R, Guilfoyle AM. Randomised controlled trial of graded exercise in chronic fatigue syndrome. Med J Aust. 2004;180:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 123] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 6. | Oh SM, Bae WK, Choo SR, Kim HT, Kim HH, Lee SH, Jeong HS. Relationship between Changes in Fatigue and Exercise by Follow-Up Period. Korean J Fam Med. 2016;37:78-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Black CD, O'connor PJ, McCully KK. Increased daily physical activity and fatigue symptoms in chronic fatigue syndrome. Dyn Med. 2005;4:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Mohamed A, Jan Y-K, El Sayed WH, El Wanis MEA, Yamany AA. Dynamic Scapular Recognition Exercise Improves Scapular Upward Rotation and Shoulder Pain and Disability in Patients with Adhesive Capsulitis: A Randomized Controlled Trial. J Man Manip Ther. 2020;28:146-158. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Mohamed AA, Jan YK. Effect of Adding Proprioceptive Exercise to Balance Training in Older Adults with Diabetes: A Systematic Review. Curr Diabetes Rev. 2020;16:327-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Alawna M, Mohamed AA. Short-term and long-term effects of ankle joint taping and bandaging on balance, proprioception and vertical jump among volleyball players with chronic ankle instability. Phys Ther Sport. 2020;46:145-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |