Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6679
Peer-review started: January 5, 2022
First decision: January 18, 2022
Revised: February 10, 2022
Accepted: May 8, 2022
Article in press: May 8, 2022
Published online: July 6, 2022
Processing time: 169 Days and 15.7 Hours
Retroperitoneal bronchogenic cyst (RBC) is an extremely rare developmental abnormality. Most are benign tumors but malignant transformation is possible. Because of their anatomical position, RBCs are easily misdiagnosed as adrenal or pancreatic solid tumors on radiological evaluation. Here, we report a case of RBC, review the literature, and summarize some important features.
A 49-year-old woman was incidentally found to have a retroperitoneal tumor during a physical examination. Enhanced computed tomography and laboratory evaluations, including routine blood examination, blood biochemistry, 24-h urine 17 ketones, 17 hydroxyls, adrenocortical hormone, serum potassium concentration, serum amylase, lipase, and epithelial tumor markers, revealed a moderate density, 54 mm × 40 mm mass with a clear boundary near the left adrenal gland. The were no abnormalities in the blood and urine values. Because the patient had a history of hypertension and the location of the mass was adjacent to the adrenal gland, it was initially diagnosed as a left adrenal tumor and was resected by retroperitoneal laparoscopy. However, the pathological examination after surgery confirmed it to be a bronchogenic cyst.
Retroperitoneal laparoscopic surgery can be prioritized for symptomatic RBC patients. Conservative treatment is feasible for selected patients.
Core Tip: Retroperitoneal bronchogenic cyst (RBC) is a very rare congenital abnormality. It is usually a benign lesion but may become malignant. It primarily occurs at 20-60 years of age, with no sex difference. Most RBCs occur on the left side of the abdomen. Imaging is often nonspecific, and the diagnosis is usually confirmed by histopathology. Magnetic resonance imaging is more useful than computed tomography, endocrinological evaluation is necessary, and retroperitoneal laparoscopic surgery is a priority for patients with symptoms. Conservative treatment is effective in selected patients, but malignant transformation, infection, and bleeding must first be ruled out.
- Citation: Gong YY, Qian X, Liang B, Jiang MD, Liu J, Tao X, Luo J, Liu HJ, Feng YG. Retroperitoneal tumor finally diagnosed as a bronchogenic cyst: A case report and review of literature. World J Clin Cases 2022; 10(19): 6679-6687
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6679.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6679
Retroperitoneal bronchogenic cysts (RBCs) are rare retroperitoneal tumors. Most bronchogenic cysts occur in the thoracic cavity but are rare occurrences in the retroperitoneum. They consist of respiratory epithelium, smooth muscle, cartilage, and mixed serous and mucous glands. The cysts are filled with high-viscosity, protein-rich mucus. Patients usually have no symptoms or have only mild abdominal pain. Most RBCs are found incidentally during an examination for another disease. Bronchogenic cysts originate in the foregut, form at about 3-7 wk of embryonic development, and are usually benign. Miller et al[1] reported the first case of a RBC in 1953. With increasing attention to health and awareness of the value of physical examination, more and more RBCs have been found, especially in patients in developing countries. However, most clinicians even in developed areas are not familiar with RBC. We used the keywords "bronchogenic cyst AND (adrenal OR retroperitoneal OR subdiaphragmatic)" to search for related articles in PubMed. Only 80 articles have been published to date, including 4 that could not be obtained as full-text publications.
A tumor was found in the left retroperitoneum during a routine follow-up examination.
The patient reported having no feelings of discomfort prior to entering our hospital, nor any weight loss or cachexia caused by the inability to eat.
The patient had a history of brain surgery for a ruptured intracranial aneurysm 6 mo previously. She had no other relevant medical history other than a 6-year history of hypertension that was controlled by amlodipine besylate tablets.
The patient revealed that there was no special personal and family history.
The patient's body temperature was 36.6 ºC, and she reported having no fever for more than 1 mo before presentation. Her blood pressure was 124/86 mmHg, and there was no shortness of breath. There was no percussion pain in the costovertebral angle on either side, and no abdominal tenderness, rebound pain, nor other positive signs.
Routine blood examination did not find any obvious abnormal results other than a slightly low plasma albumin level.
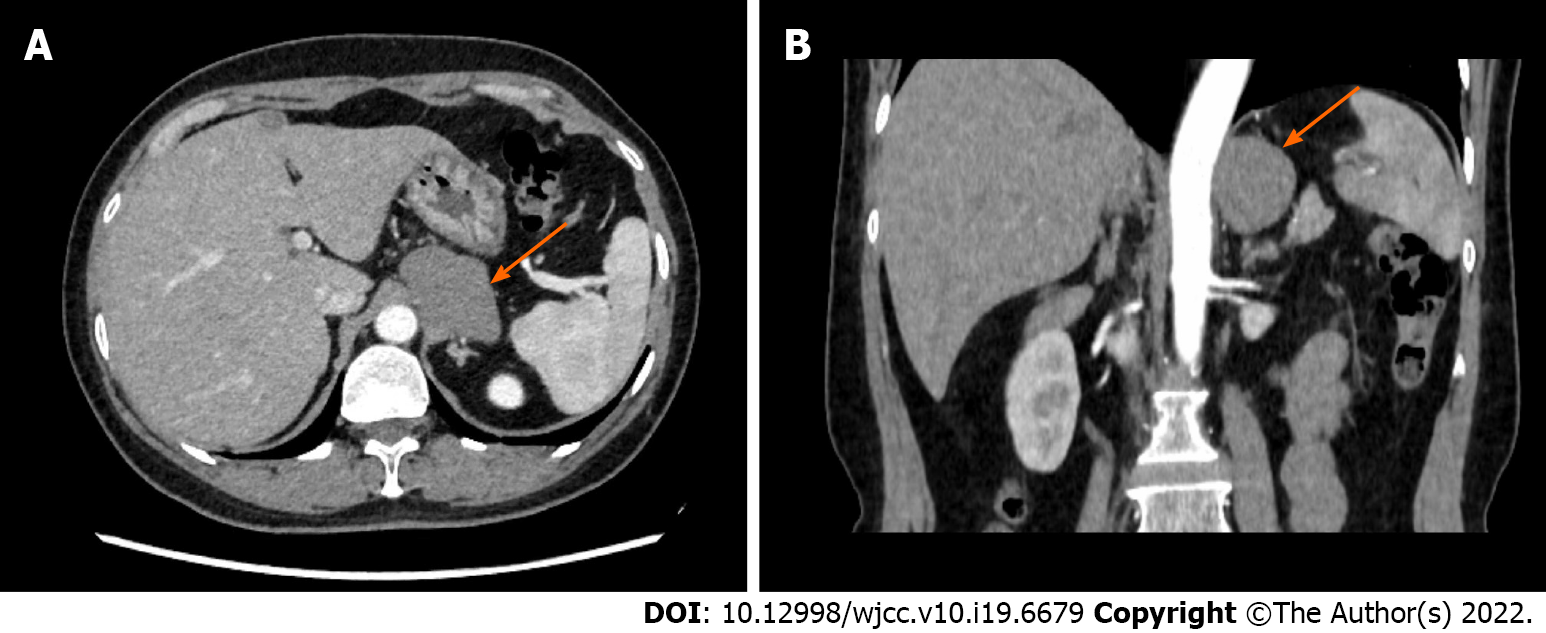
Contrast-enhanced computed tomography (CT) revealed an oval, 54 mm × 40 mm cystic, moderate-density mass near the left adrenal gland. It showed a clear boundary and a uniform density of 85 HU (Figure 1).
The patient’s findings for 24-h urine, 17 ketones, 17 hydroxyls, adrenocortical hormone, serum potassium concentration, serum amylase, lipase, and epithelial tumor markers, as well as endocrinological results were normal.
RBC.
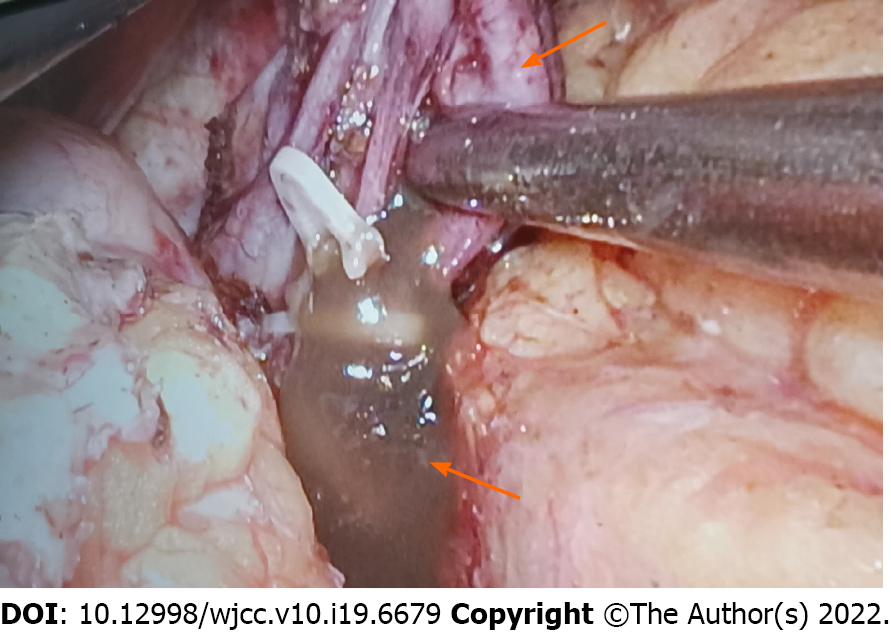
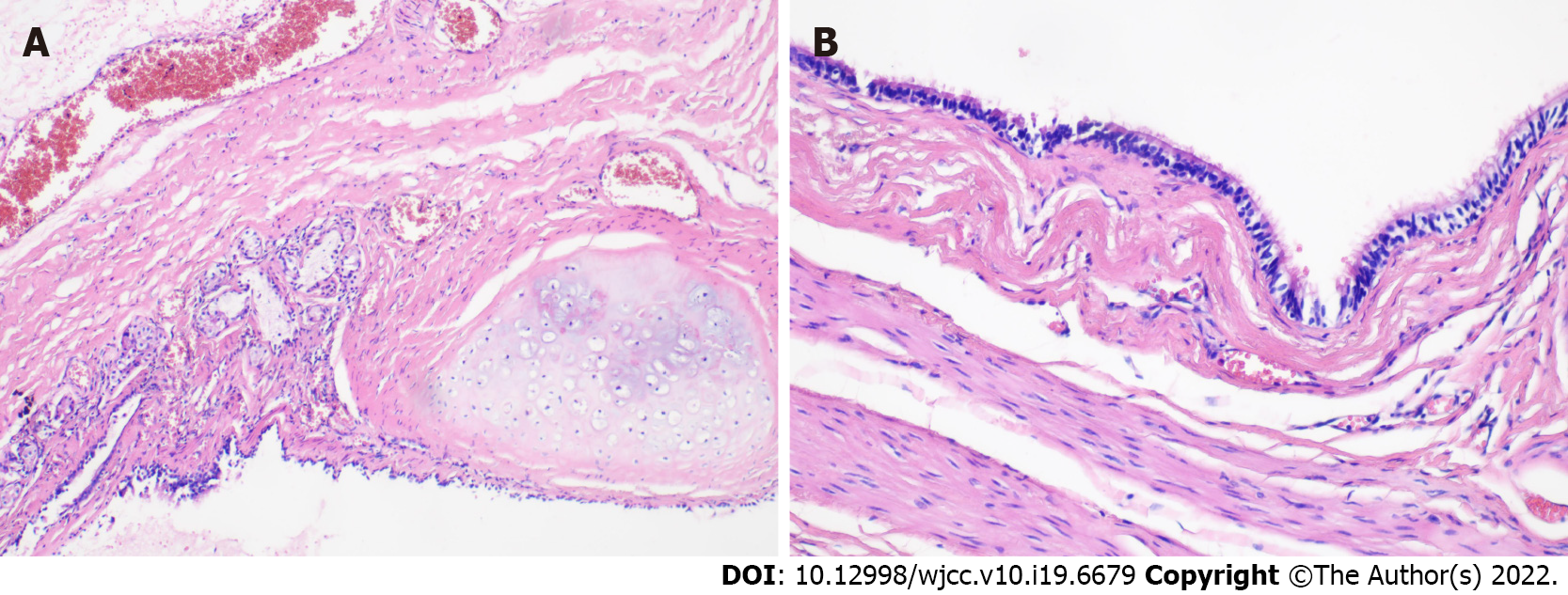
As we were not sure whether the tumor was benign or malignant, and to avoid the possibility of a malignant tumor and further growth, we performed a retroperitoneal laparoscopic exploration. With the patient placed in the right oblique position, laparoscopy found a mass of about 54 mm × 40 mm with a cystic appearance. The base was located in the upper part of the medial branch of the left adrenal gland, behind the pancreas. It adhered to the pancreas and surrounding tissues. The cyst ruptured unexpectedly in the process of being dissociated and it released some of its contents, which appeared as a brown jelly-like substance (Figure 2). We immediately applied negative pressure drainage to suck out the contents of the cyst to prevent spreading. After the cyst was completely removed, we examined the surrounding adjacent tissue and found no obvious changes. Postoperative pathological examination showed respiratory epithelium, smooth muscle, cartilage, and mucous glands (Figure 3), consistent with an RBC.
The patient was discharged from the hospital on the 4th day after operation. After follow-up of more than 6 mo, the tumor did not recur and the patient did not have any tumor-related symptoms. The patient did not receive further treatment.
RBCs arise from abnormal development of the foregut in the early stage of embryonic development. Sumiyoshi et al[2], Swanson et al[3], and Reichelt et al[4] described the connection of the abdominal cavity and thoracic cavity by pericardial ducts at about 3-7 wk of gestation, and the development of the ventral or dorsal part of the foregut developed into the tracheobronchial tree and esophagus. Bronchogenic cysts usually occur in the lungs or the posterior mediastinum[5,6]. With the formation of the diaphragm, some dysplastic tracheobronchial trees may be cut off, forming ectopic bronchogenic cysts under the diaphragm[7,8]. Another hypothesis is that RBCs originate from abnormal differentiation of abdominal foregut-derived cysts[9]. Pluripotent differentiated primordial cells from the ventral foregut migrate to the abdomen, where they differentiate into bronchogenic cysts containing cartilage or esophageal and gastrointestinal cysts with different characteristics[10].
The prevalence of bronchogenic cysts in the general population is estimated to range from 1/42000 to 1/68000[11]. It is higher in men than in women, with a male:female ratio of 4:1[12]. About 86% of bronchogenic cysts occur in the mediastinum and lungs[13]. RBCs are very rare, accounting for only 0.03% of all cases[5]. Our search of the published literature found a total of 80 articles published in English. A total of 86 cases were described (48% in men and 52% in women). The age at diagnosis ranged from prenatal to 75 years[14-17]. The average age at diagnosis was 39 ± 16 years and 82% were diagnosed in patients between 20 years and 60 years of age.
Most RBCs described in the literature appeared to the left of the midline, accounting for almost 78% of cases. This is similar to the 82% reported by Liang et al[18] that were found within a triangle behind the stomach, defined by the midline, splenic vein, spleen, and diaphragm. Given the location, it is possible that during embryonic development, the caudal primitive foregut is related to the counterclockwise transposition of the midgut from left to right, while the exfoliated germ remains on the left side[19]. In addition, in the 3rd week of embryonic development, the development of the liver hinders abnormal sprouting of the tracheobronchial tree, and it enters the diaphragm[20]. About 73% of the bronchogenic cysts on the left are near the left adrenal gland. Bronchogenic cysts near the right adrenal gland accounted for about 12% of the reports. There is only one reported case of a bilateral bronchogenic cyst surrounding both adrenal glands[21] and two cases on the inferior midline of the diaphragm or in front of the abdominal aorta[22,23]. Bronchogenic cysts located around the pancreas account for about 10% of the reported cases, and an interesting case occurred in the left iliac fossa[24]. The average diameter of the RBCs in published reports was 5.8 cm, with a maximum diameter of about 20 cm in a case reported by Mirsadeghi et al[25]. We did not find a correlation of tumor size with age.
Bronchogenic cysts are usually not symptomatic unless they are accompanied by a secondary infection, perforation, bleeding, or compression of the adjacent organs[26]. Bronchogenic cysts that occur in the chest may be accompanied by retrosternal pain, dysphagia, cough, fever, and hemoptysis[16]. RBCs are located close to the adrenal glands, kidney, pancreas, or gastrointestinal tract, and may be accompanied by upper abdominal pain, digestive tract symptoms (nausea, vomiting), and back pain.
In our review of the 86 previously reported RBCs, about 48% were not symptomatic, and were incidental finding during a physical examination conducted for an unrelated reason. About 46% were accompanied by waist or abdominal pain or discomfort that was most likely caused by increased cyst volume and compression of adjacent organs, which is different from the percentage reported by Liang et al[18]. Six cases were accompanied by digestive tract symptoms, five by back pain, four by varying degrees of weight loss, and one by a secondary infection associated with the cyst[27]. One case was accompanied by a urinary tract infection, but it was not clear whether the infection was associated with the cyst[7]. Doggett et al[28] reported pheochromocytoma-like symptoms in a 44-year-old patient with cyst compression of the adrenal gland, but our review found that RBCs rarely caused adrenal hypofunction, Cushing syndrome, or pheochromocytoma. Most patients with a history of hypertension had no significant decrease in their blood pressure after relief of the compression.
It is often difficult to diagnose RBCs by imaging examinations. Ultrasonography is not useful, especially if the fluid density within the cyst is high. In most cases, CT and magnetic resonance imaging (MRI) are more useful. In our case, CT showed a nearly round, well-defined, low-density homogeneous mass with no significant enhancement after injection of contrast medium (Figure 1). Most RBCs are unilocular, but irregularly shaped septal cysts have been reported[25,29]. The fluid within RBCs is usually rich in protein and mucus, and they produce a low-density shadow on CT. The cyst density has been reported to range from 6-100 HU, varying with the protein content[6,17]. The CT performance varies according to differences in the other components of the fluid in the capsule. Bleeding, infection, or calcification in the cyst are seen as a high-density shadow with uneven density[19,30-32], and increased bleeding or a high-protein content make it easy to mistake the RBC for a solid or cystic solid tumor[30,33].
MRI is more valuable in the diagnosis of RBCs. Cysts with serous fluids and a low protein concentration have a low signal intensity on T1-weighted images and enhanced signal intensity on T2-weighted images[13,34,35], but most RBCs contain a thick protein solution and have high signal intensity on both T1- and T2-weighted images[31]. In addition, fat-suppressed T1-weighted images can be used to distinguish bronchogenic cysts from malignant masses like teratomas and dermoid cysts[36-38]. Duan et al[39] and Fiorelli et al[40] have shown that Technetium (99mTc)-methoxyisobutylisonitrile (commonly known as MIBI) is involved in the transport of P-glycoprotein and that P-protein is highly expressed in malignant tumors; consequently, 99mTc-MIBI-single-photon emission computed tomography (commonly known as SPECT) can be used to differentiate benign from malignant tumors. Yoon et al[41] and Brient et al[42] found that RBCs have no fluorodeoxyglucose uptake, which can be used to evaluate the degree of infection or the malignant changes of RBCs.
As RBCs do not have specific clinical characteristics, none of the previously reported cases have been accurately diagnosed before surgery or an invasive procedure. A preoperative differential diagnosis would help clinicians to choose the most appropriate treatment. About 73% of RBCs are found around the left adrenal gland, and adrenal tumors are usually considered as the initial diagnosis. If the mass is located around the adrenal gland, then serum potassium, 24-h urinary cortisol, cortisol, and basal serum adrenocorticotropic hormone levels can exclude Cushing syndrome. Urinary catecholamine and plasma norepinephrine can detect the presence of a pheochromocytoma[34]. If the lesion is located around the pancreas, serum amylase and lipase levels must be determined. Cassiani et al[43] reported elevated serum amylase (119 U/L) in a patient with endoscopic ultrasound guided fine-needle biopsy. That patient was eventually diagnosed with an RBC, but RBCs usually do not cause an increase in serum amylase. Except for 1 case with serum carbohydrate antigen (CA)19-9 and carcinoembryonic antigen (CEA) levels higher than 1200 U/mL[1], no significant increase of tumor markers has been reported. We believe that the levels of tumor markers such as CA19-9, β-human chorionic gonadotropin, a-fetoprotein, and CEA are of value in determining whether retroperitoneal masses are malignant.
Jannasch et al[44] described the histology of 15 cases of RBCs, which included involvement of respiratory epithelium (100%), hyaline cartilage (73%), smooth muscle (80%), and serous or bronchogenic glands (93%), and without immature components, atypia, or tumor necrosis. Microscopically, the inner surface of RBCs is pseudostratified ciliated columnar epithelium, with a small number of goblet cells. The cyst wall is comprised of dense fibrous connective tissue with lymphatic plasma cell infiltration and partial calcification[45]. Other components include tiny arteries, veins, capillaries, nerves, and rare smooth muscle fibers[28]. Our case had histological features characteristic of bronchogenic cysts, including respiratory epithelium, smooth muscle, cartilage, and mucous glands. Most often, the fluid within the RBC capsule is thick mucus, rich in protein. Calcium deposits have been reported[46,47] but are very rare.
The majority of retroperitoneal tumors are malignant[48], and although there are cases of malignant transformation of RBCs[49], they are generally benign. In addition to RBCs, other retroperitoneal benign tumors include fibromatosis, lipomas, angiolipomas, and leiomyomas. The differential diagnosis should include cystic teratoma, bronchopulmonary sequestration, cystic lymphangioma, mucinous cysta
In addition to adrenocortical or medullary tumors, RBCs should be differentiated from cystic teratoma, bronchopulmonary sequestration, and esophageal cysts. Mature cystic teratoma often occurs in the midline[50] and most bronchogenic cysts are located to the left of the midline. If there is low attenuated fat in the cyst and calcification of the cyst wall on CT, then cystic teratoma is more likely[33]. Cystic teratomas include bronchogenic tissue derived from endoderm and other tissues derived from mesoderm and ectoderm. RBCs do not have those structures[29]. Bronchopulmonary sequestration consists of differentiated lung parenchyma, bronchus, and pleural tissue[8,50] that can be easily differentiated from RBCs. Esophageal cysts have two layers of smooth muscle, often with squamous epithelium and no cartilage[8,29].
Preoperative diagnosis of RBC is difficult. Before obtaining pathological or histological results, if malignant tumors cannot be excluded, surgical treatment is recommended to make a clear diagnosis, relieve symptoms, and prevent complications. Retroperitoneal laparoscopic surgery[51], laparoscopic surgery[52], and open surgery[16] have been proven to be safe and effective. There is no evidence that either transabdominal or retroperitoneal approaches are more advantageous[44]. Retroperitoneal approaches may reduce pain, but the choice of surgical methods or approaches should be based on the clinician's preference. If the patient's physical condition permits, the preoperative diagnosis can be completed by fine-needle aspiration[16,53]. If the biopsy results are consistent with bronchogenic cysts, conservative treatment is also feasible if the patient is asymptomatic and the cyst has a small diameter.
We found that the diameter of cysts in reports of patients with lumbar and abdominal pain was 6 cm, while the diameter of cysts in patients without pain was 4 cm (Table 1). Although fine-needle aspiration biopsy is considered safe, it can lead to malignant cell spread and false-negative results[54]. When patients choose conservative treatment, they must be informed that their symptoms may worsen as the diameter of the tumor increases, although the increase is generally very slow. Brient et al[42] reported a patient diagnosed with an RBC without surgical treatment who remained stable after 3 years of follow-up.
| With waist and abdominal pain, n = 38 | Without waist and abdominal pain, n = 45 | P value | |
| Cyst size in cm | 6.0 (4-8.1) | 4.0 (3.2-5.3) | 0.006 |
RBCs are a benign developmental abnormality with the possibility of malignant transformation. At least half of the patients have no obvious symptoms. If present, the typical clinical symptoms are abdominal pain and gastrointestinal reactions. Endocrinological examination is usually not specific, and MRI is superior to CT. Typical histological findings include respiratory epithelium, smooth muscle, cartilage, and mucous glands. Fine-needle biopsy can be helpful for a definite diagnosis. Conservative treatment is feasible for selected patients. We recommend that RBCs with no symptoms and less than 4 cm in size be treated conservatively. Symptomatic cysts larger than 4 cm can be treated by surgery, and those larger than 6 cm should be surgically removed regardless of whether the patient has symptoms or not. Three surgical methods — retroperitoneal laparoscopic surgery, laparoscopic surgery, and open surgery — have been used successfully.
The authors thank Dr. Cai X and Dr. Ran C for their assistance with literature searching and checking of the results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dayan D, Israel; Lin F, China S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Miller RF, Graub M, Pashuck ET. Bronchogenic cysts; anomalies resulting from maldevelopment of the primitive foregut and midgut. Am J Roentgenol Radium Ther Nucl Med. 1953;70:771-785. [PubMed] |
| 2. | Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Swanson SJ 3rd, Skoog SJ, Garcia V, Wahl RC. Pseudoadrenal mass: unusual presentation of bronchogenic cyst. J Pediatr Surg. 1991;26:1401-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Reichelt O, Grieser T, Wunderlich H, Möller A, Schubert J. Bronchogenic cyst. A rare differential diagnosis of retroperitoneal tumors. Urol Int. 2000;64:216-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Menke H, Röher HD, Gabbert H, Schweden F. Bronchogenic cyst: a rare cause of a retroperitoneal mass. Eur J Surg. 1997;163:311-314. [PubMed] |
| 6. | Runge T, Blank A, Schäfer SC, Candinas D, Gloor B, Angst E. A retroperitoneal bronchogenic cyst mimicking a pancreatic or adrenal mass. Case Rep Gastroenterol. 2013;7:428-432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Cetinkurşun S, Oztürk H, Celasun B, Sakarya MT, Sürer I. Isolate abdominal bronchogenic cyst: a case report. Eur J Pediatr Surg. 1997;7:103-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Haddadin WJ, Reid R, Jindal RM. A retroperitoneal bronchogenic cyst: a rare cause of a mass in the adrenal region. J Clin Pathol. 2001;54:801-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Coselli MP, de Ipolyi P, Bloss RS, Diaz RF, Fitzgerald JB. Bronchogenic cysts above and below the diaphragm: report of eight cases. Ann Thorac Surg. 1987;44:491-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 72] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Yamamoto E, Nakayama H, Ozaki N, Kitamura Y, Funatsuka M, Ueda M, Chikugo K, Hirata A, Kurashina A, Kuratsuka H, Nakagawa M, Nagaoka S. Laparoscopically resected foregut cyst adjacent to the right adrenal gland. Diagn Ther Endosc. 1998;5:53-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Sanli A, Onen A, Ceylan E, Yilmaz E, Silistreli E, Açikel U. A case of a bronchogenic cyst in a rare location. Ann Thorac Surg. 2004;77:1093-1094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Pujary K, Pujary P, Shetty R, Hazarika P, Rao L. Congenital cervical bronchogenic cyst. Int J Pediatr Otorhinolaryngol. 2001;57:145-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Liu HS, Li SQ, Cao ZL, Zhang ZY, Ren H. Clinical features and treatment of bronchogenic cyst in adults. Chin Med Sci J. 2009;24:60-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Lahey FH, Eckerson EB. RETROPERITONEAL CYSTS. Ann Surg. 1934;100:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Bagolan P, Bilancioni E, Nahom A, Trucchi A, Inserra A, Neri M, Spina V, Giorlandino C. Prenatal diagnosis of a bronchogenic cyst in an unusual site. Ultrasound Obstet Gynecol. 2000;15:66-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Maly T, Mihal V, Michalkova K, Tichy T, Neoral C, Zonca P. Retroperitoneal bronchogenic cyst: prenatal diagnosis of cystoid formation, its progression and surgery. Bratisl Lek Listy. 2014;115:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Terry NE, Senkowski CK, Check W, Brower ST. Retroperitoneal foregut duplication cyst presenting as an adrenal mass. Am Surg. 2007;73:89-92. [PubMed] |
| 18. | Liang MK, Yee HT, Song JW, Marks JL. Subdiaphragmatic bronchogenic cysts: a comprehensive review of the literature. Am Surg. 2005;71:1034-1041. [PubMed] |
| 19. | Wen Y, Chen W, Chen J, He X. Retroperitoneal bronchogenic cyst resembling an adrenal tumor: two case reports and literature review. J Int Med Res. 2020;48:300060520925673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 20. | Kohno M, Namura K, Fujikawa A, Sawada T, Oota J, Moriyama M. [A case of retroperitoneal bronchogenic cyst treated by laparoscopic surgery]. Hinyokika Kiyo. 2013;59:359-361. [PubMed] |
| 21. | Cao DH, Zheng S, Lv X, Yin R, Liu LR, Yang L, Huang Y, Wei Q. Multilocular bronchogenic cyst of the bilateral adrenal: report of a rare case and review of literature. Int J Clin Exp Pathol. 2014;7:3418-3422. [PubMed] |
| 22. | Herek D, Erbiş H, Kocyigit A, Yagci AB. Retroperitoneal Bronchogenic Cyst Originating from Diaphragmatic Crura. Indian J Surg. 2015;77:1397-1398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Amendola MA, Shirazi KK, Brooks J, Agha FP, Dutz W. Transdiaphragmatic bronchopulmonary foregut anomaly: "Dumbell" bronchogenic cyst. AJR Am J Roentgenol. 1982;138:1165-1167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Subramanian JB, K S S, Selvarangam S. A case report- retroperitoneal bronchogenic cyst in relation to the hindgut. Int J Surg Case Rep. 2020;75:140-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Mirsadeghi A, Farrokhi F, Fazli-Shahri A, Gholipour B. Retroperitoneal bronchogenic cyst: a case report. Med J Islam Repub Iran. 2014;28:56. [PubMed] |
| 26. | Başoğlu M, Karabulut K, Özbalcı GS, Aykun N, Çamlıdağ İ, Güngör BB, Kefeli M. Laparoscopic resection of retroperitoneal bronchogenic cyst clinically presenting as adrenal cyst. Turk J Surg. 2018;1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Tadokoro T, Misumi T, Itamoto T, Nakahara H, Matsugu Y, Ikeda S, Oshita A, Hotta R, Miguchi M, Chogahara I, Nishikawa S, Hiroi S, Nishisaka T. Retroperitoneal Bronchogenic Cyst Resected by Single-Incision Laparoscopic Surgery in an Adolescent Female: A Case Report. Asian J Endosc Surg. 2022;15:206-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Doggett RS, Carty SE, Clarke MR. Retroperitoneal bronchogenic cyst masquerading clinically and radiologically as a phaeochromocytoma. Virchows Arch. 1997;431:73-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 29. | Onol FF, Baytekin F, Dikbas O, Ergönenç T, Tanidir Y. A retroperitoneal bronchogenic cyst mimicking adrenal tumour in an adult: is differential diagnosis truly possible? J Clin Pathol. 2009;62:187-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Wang SE, Tsai YF, Su CH, Shyr YM, Lee RC, Tsai WC, Li FY, Chen TH, Wu CW, Lui WY. Retroperitoneal bronchogenic cyst mimicking pancreatic cystic lesion. J Chin Med Assoc. 2006;69:538-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Kim EY, Lee WJ, Jang KT. Retroperitoneal bronchogenic cyst mimicking a pancreatic cystic tumour. Clin Radiol. 2007;62:491-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Qingyu J, Xiaolong L, Ruohan Z, Licong M, Zhichao T, Qingwei C, Yuan W, Ying Z. Computed tomography helps pre-operative evaluation before laparoscopic resection of retroperitoneal bronchogenic cyst: A case report. J Minim Access Surg. 2021;17:95-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Hwang HY. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004;24:1353-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 241] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 34. | Govaerts K, Van Eyken P, Verswijvel G, Van der Speeten K. A bronchogenic cyst, presenting as a retroperitoneal cystic mass. Rare Tumors. 2012;4:e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Ingu A, Watanabe A, Ichimiya Y, Saito T, Abe T. Retroperitoneal bronchogenic cyst: a case report. Chest. 2002;121:1357-1359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Buckley JA, Siegelman ES, Birnbaum BA, Rosato EF. Bronchogenic cyst appearing as a retroperitoneal mass. AJR Am J Roentgenol. 1998;171:527-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 37. | Murakami R, Machida M, Kobayashi Y, Ogura J, Ichikawa T, Kumazaki T. Retroperitoneal bronchogenic cyst: CT and MR imaging. Abdom Imaging. 2000;25:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 38. | Tong HX, Liu WS, Jiang Y, Liu JU, Zhou JJ, Zhang Y, Lu WQ. Giant retroperitoneal bronchogenic cyst mimicking a cystic teratoma: A case report. Oncol Lett. 2015;9:2701-2705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Duan XY, Wang JS, Liu M, Guo YM. Technetium-99m-hexakis-2-methoxyisobutylisonitrile scintigraphy and multidrug resistance-related protein expression in human primary lung cancer. Ann Nucl Med. 2008;22:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Fiorelli A, Rambaldi P, Accardo M, Santini M. Malignant transformation of bronchogenic cyst revealed by 99mTc-MIBI-SPECT. Asian Cardiovasc Thorac Ann. 2012;20:347-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Yoon YR, Choi J, Lee SM, Kim YJ, Cho HD, Lee JW, Jeon YS. Retroperitoneal Bronchogenic Cyst Presenting Paraadrenal Tumor Incidentally Detected by (18)F-FDG PET/CT. Nucl Med Mol Imaging. 2015;49:69-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Brient C, Muller C, Cassagneau P, Taieb D, Sebag F, Henry JF. A retroperitoneal bronchogenic cyst. J Visc Surg. 2012;149:e361-e363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Cassiani J, Crinò SF, Manfrin E, Rivelli M, Gabbrielli A, Guglielmi A, Pedrazzani C. Endoscopic Ultrasound Through-the-Needle Biopsy for the Diagnosis of an Abdominal Bronchogenic Cyst. Clin Endosc. 2021;54:767-770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 44. | Jannasch O, Büschel P, Wodner C, Seidensticker M, Kuhn R, Lippert H, Mroczkowski P. Retroperitoneoscopic and laparoscopic removal of periadrenally located bronchogenic cysts--a systematic review. Pol Przegl Chir. 2013;85:706-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Paik SS, Jang KS, Han HX, Oh YH, Lee KG, Choi D. Retroperitoneal bronchogenic cyst mimicking pancreatic pseudocyst in a patient with colorectal cancer. J Gastroenterol Hepatol. 2005;20:802-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | O'Neal PB, Moore FD, Gawande A, Cho NL, King EE, Moalem J, Ruan D. Bronchogenic cyst masquerading as an adrenal tumor: a case of mistaken identity. Endocr Pract. 2012;18:e102-e105. [PubMed] [DOI] [Full Text] |
| 47. | Hisatomi E, Miyajima K, Yasumori K, Okamura H, Nonaka M, Watanabe J, Muranaka T, Mori H. Retroperitoneal bronchogenic cyst: a rare case showing the characteristic imaging feature of milk of calcium. Abdom Imaging. 2003;28:716-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Inaba K, Sakurai Y, Umeki Y, Kanaya S, Komori Y, Uyama I. Laparoscopic excision of subdiaphragmatic bronchogenic cyst occurring in the retroperitoneum: report of a case. Surg Laparosc Endosc Percutan Tech. 2010;20:e199-e203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 49. | Sullivan SM, Okada S, Kudo M, Ebihara Y. A retroperitoneal bronchogenic cyst with malignant change. Pathol Int. 1999;49:338-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 50. | Matsubayashi J, Ishida T, Ozawa T, Aoki T, Koyanagi Y, Mukai K. Subphrenic bronchopulmonary foregut malformation with pulmonary-sequestration-like features. Pathol Int. 2003;53:313-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 51. | Chung JM, Jung MJ, Lee W, Choi S. Retroperitoneal bronchogenic cyst presenting as adrenal tumor in adult successfully treated with retroperitoneal laparoscopic surgery. Urology. 2009;73:442.e13-442.e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 52. | Cai Y, Guo Z, Cai Q, Dai S, Gao W, Niu Y, Li G, Zhang Y. Bronchogenic cysts in retroperitoneal region. Abdom Imaging. 2013;38:211-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 53. | Obando J, Merkle E, Bean SM. A retroperitoneal bronchogenic cyst. Clin Gastroenterol Hepatol. 2009;7:A24-Ae1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 54. | Andersson R, Lindell G, Cwikiel W, Dawiskiba S. Retroperitoneal bronchogenic cyst as a differential diagnosis of pancreatic mucinous cystic tumor. Dig Surg. 2003;20:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |