Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6617
Peer-review started: December 20, 2021
First decision: January 25, 2022
Revised: February 9, 2022
Accepted: May 5, 2022
Article in press: May 5, 2022
Published online: July 6, 2022
Processing time: 185 Days and 19.3 Hours
Cryptococcal osteomyelitis is a bone infection caused by cryptococcus. As an opportunistic infection, bone cryptococcosis usually occurs in patients with immunodeficiency diseases or in those undergoing immunosuppressive therapy and often displays characteristics of disseminated disease. Isolated cryptococcal osteomyelitis is extremely unusual in immunocompetent person. The pathogenic fungus often invades vertebrae, femur, tibia, rib, clavicle, pelvis, and humerus, but the ulna is a rare target.
A 79-year-old woman complaining of chronic pain, skin ulceration and a sinus on her right forearm was admitted, and soon after was diagnosed with cryptococcal osteomyelitis in the right ulna. Unexpectedly, she was also found to have apparently normal immunity. After treatment with antifungal therapy combined with surgery debridement, the patient’s osteomyelitis healed with a satisfactory outcome.
Although rare, cryptococcal osteomyelitis should be considered in the differential diagnosis of osteolytic lesions even in immunocompetent patients, and good outcomes can be expected if early definitive diagnosis and etiological treatment are established.
Core Tip: Cryptococcal osteomyelitis often occurs in immunocompromised patients and usually involves vetebrae, femur, tibia, rib, clavicle, pelvis. Here we report a case of isolated cryptococcal osteomyelitis in the ulna in an immunocompetent elderly woman, which is extremely rare. She was timely diagnosed and treated, and achieved good clinical outcome. Although rare, cryptococcal osteomyelitis should be considered in the differential diagnosis of osteolytic lesions even in immunocompetent patients.
- Citation: Ma JL, Liao L, Wan T, Yang FC. Isolated cryptococcal osteomyelitis of the ulna in an immunocompetent patient: A case report. World J Clin Cases 2022; 10(19): 6617-6625
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6617.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6617
Cryptococci belong to the basidiomycete subfamily of fungi. To date, there are at least 37 types of cryptococci, but only two of them are known to cause human disease, namely cryptococcus neoformans and cryptococcus gattii[1,2]. Cryptococcus neoformans has a global distribution and is found in the droppings of some birds, such as pigeons and chickens[3]. Cryptococcus neoformans commonly invades immunocompromised hosts, but sometimes also invades immunocompetent hosts[4-6]. It is often transmitted to humans via inhalation to the lung from the environment and causes cryptococcal pneumonia[7]. The central nervous system is another common site of cryptococcal infection[8]. Bone tissue involvement accounts for only 5% to 10% of all disseminated cryptococcosis cases[9]. Cryptococcal osteomyelitis occurring in immunocompetent persons is rare, especially in the ulna[10,11]. Here we present a case of isolated cryptococcal osteomyelitis of the ulna in an apparently immunocompetent patient.
A 79-year-old woman presented with a 2-mo history of pain and a 1-mo history of skin ulceration on her right forearm. The pain was exacerbated by limb movement.
Two months previously, the patient attended a local hospital and underwent X-rays which showed osteolytic lesions involving the mid-lower part of the right ulna with an internal fixation device for an olecranon fracture that had healed. The patient did not receive any specific treatment. One month ago, a skin ulcer appeared with purulent exudation, which was about the size of a soybean. The patient was referred to our hospital for further treatment.
Two years ago, she underwent surgery due to a fracture of the right ulna olecranon in a local hospital, soon after the wound healed well and limb function recovered to nearly normal level until onset of the present disease.
The patient was a farmer with normal physique. Her medical history showed no immune abnormalities or long-term use of steroids. She also denied personal and family history of hepatitis B, tuberculosis or acquired immune deficiency syndrome, diabetes or hypertension, respiratory, cardiovascular or neuropsychiatric diseases.
The patient’s vital signs were normal and stable. No abnormalities in the lung or central nervous system were found on physical examination. At the mid-lower part of the right forearm a 3 cm × 2 cm chronic wound was observed with granulation tissue and purulent discharge, and a sinus deep into the bony surface of the ulna was noted (Figure 1).
Laboratory examinations showed a normal white blood cell count, but an increased percentage of neutrophils (80.6%), slightly elevated erythrocyte sedimentation rate (66 mm) and high-sensitivity C-reactive protein (74.26 mg/L) levels.
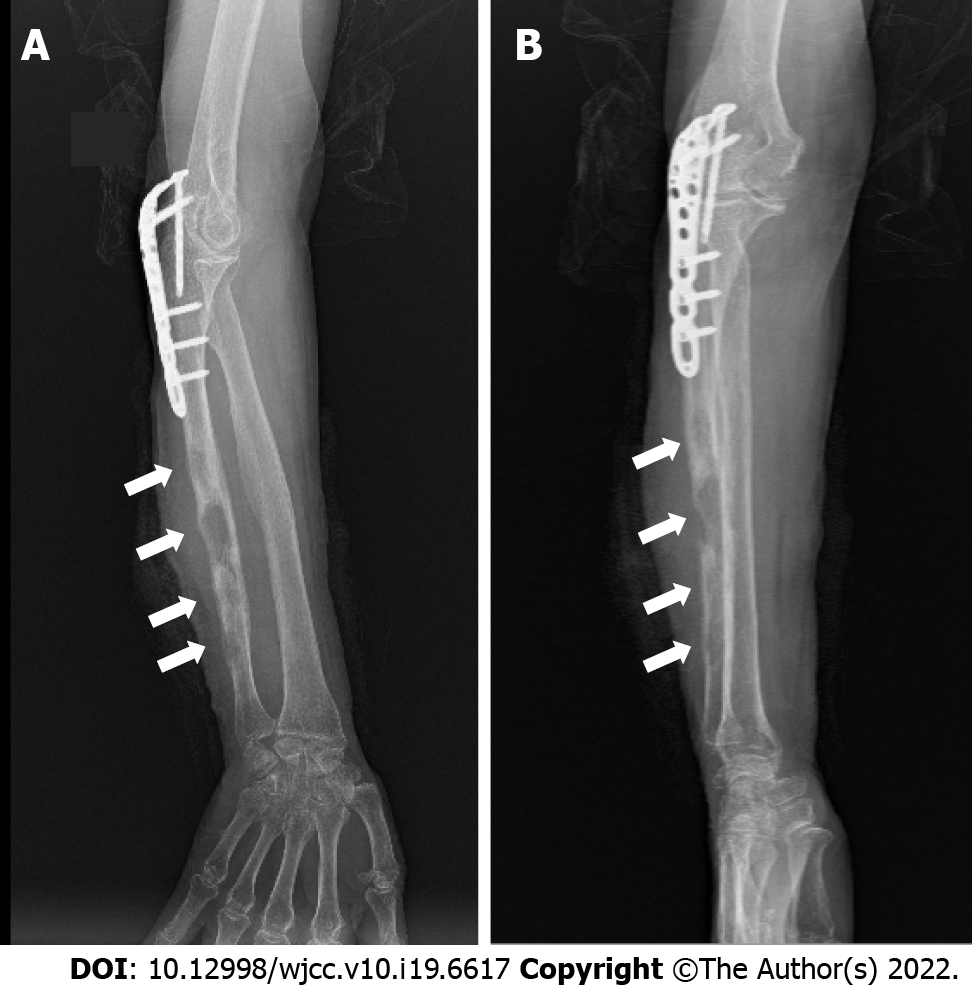
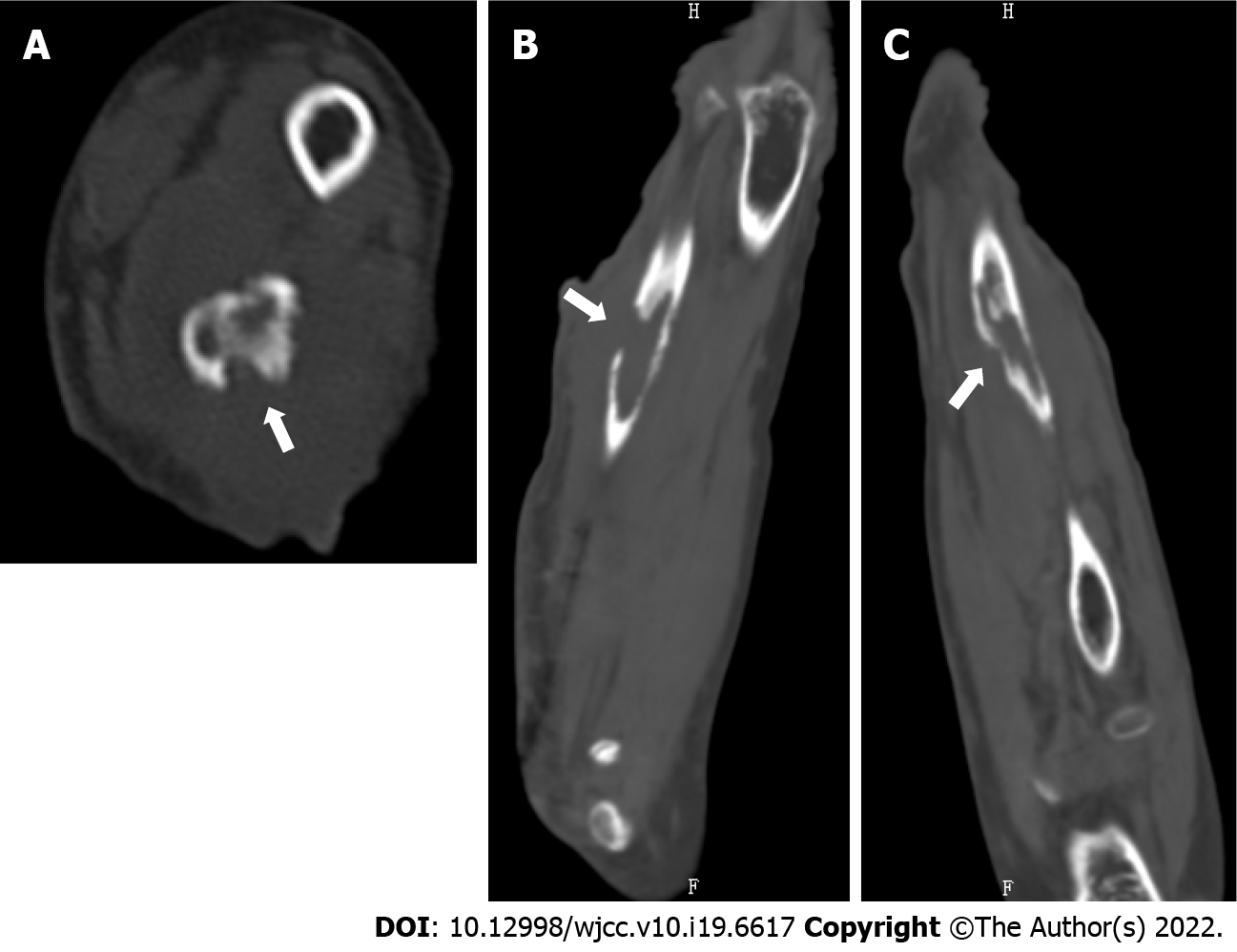
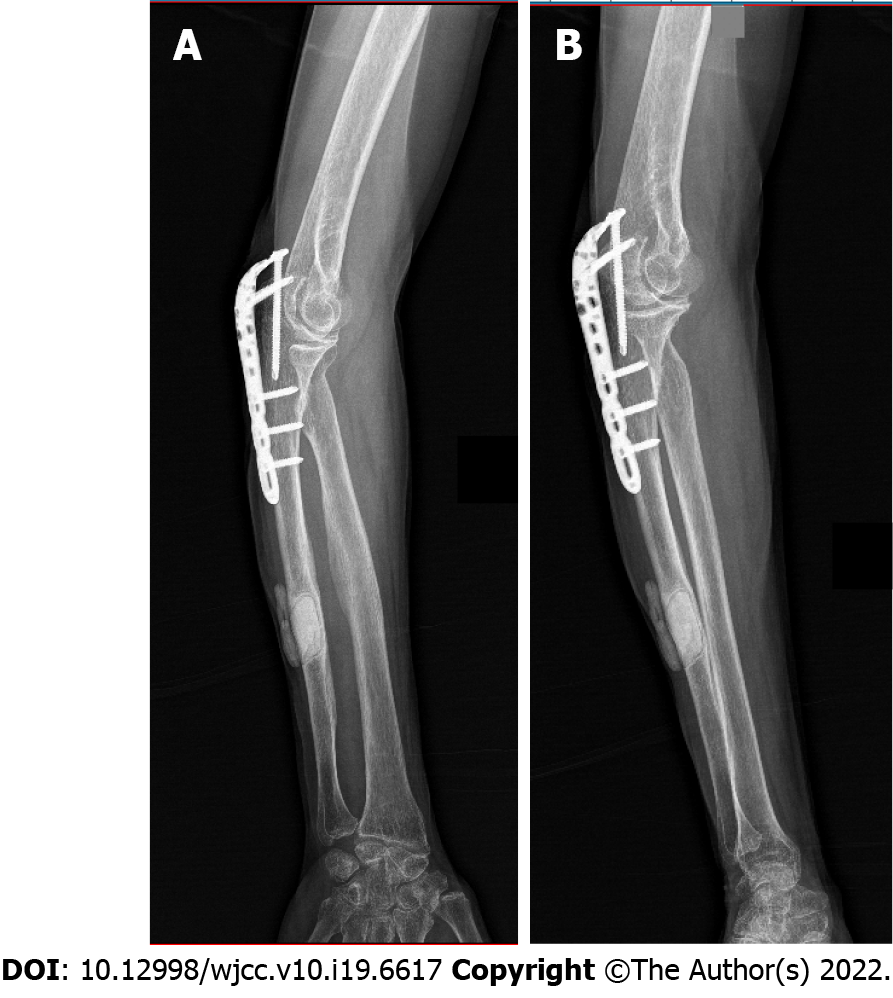
The patient’s chest X-ray was normal. Radiographs of the right forearm revealed multiple irregular and different sized osteolytic lesions with little periosteal reaction around the diaphyseal bone at the mid-distal shaft of the ulna; however, the internal fixation of the proximal segment of the ulna showed no signs of loosening (Figure 2A and B). A computed tomography (CT) scan demonstrated the largest osteolytic lesion in the mid-distal portion of the right ulna, measuring 2.9 cm × 1.2 cm × 4.2 cm (Figure 3A-C).
Pyogenic osteomyelitis was initially diagnosed given the findings on physical examination, laboratory investigations, and radiographs. The purulent exudate from the wound sinus was obtained for microscopy (Gram stain), bacterial and fungal culture, and antibiotic sensitivity. The results demonstrated growing yeast which was identified as cryptococcus neoformans. Multidisciplinary expert consultation excluded concomitant infection in the lung or central nervous system due to no associated symptoms and signs.
The patient was admitted to our hospital. Serum cryptococcal latex agglutination antigen tests and blood bacterial and fungal culture were additionally performed and both were negative. Cerebrospinal fluid was not examined as lumbar puncture was refused by the patient. There was no evidence of human immunodeficiency virus (HIV), hepatitis B, tuberculosis, sarcoidosis, diabetes mellitus. Peripheral blood T-lymphocyte subsets examination revealed normal CD4+ percentage (30.87%), CD8+ percentage (21.08%), and CD4/CD8 (1.46), but slightly decreased total T-lymphocyte percentage (53.24%) and count (603/μL), and slightly decreased CD4+ count (350/μL). In addition, increased B-lymphocyte percentage (23.89%), and natural killer (NK) cell percentage (20.50%) were observed. CT scan of the head demonstrated no inflammatory lesions.
The diagnosis of cryptococcal osteomyelitis of the right ulna was finally determined based on the clinical manifestations, imaging findings, etiology, and histopathology.
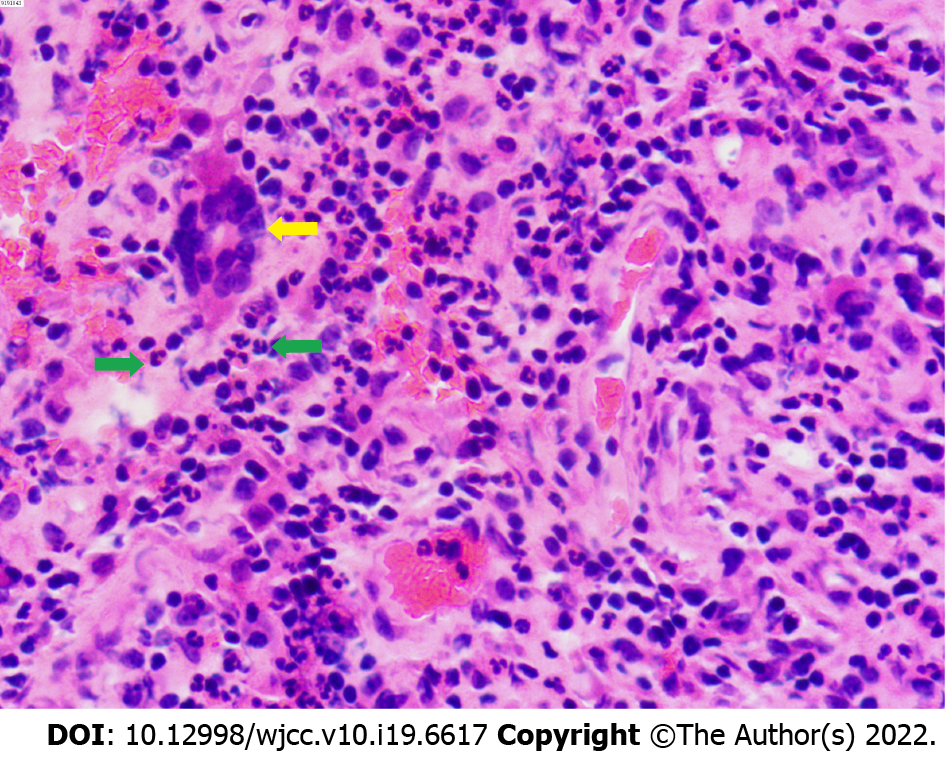
According to culture and drug sensitivity results, the patient was immediately treated with fluconazole 200 mg intravenously (IV) twice a day. Surgical debridement was also performed, pus and infected tissues were also collected for further culture and drug sensitivity, and necrotic bone, sinus, and inflammatory granulation tissues were completely removed for histopathology analysis. The wound was irrigated with normal saline, hydrogen peroxide and iodophor (Figure 4), and the bone defect space was filled with an appropriate amount of bone cement mixed with 80 mg of gentamycin and 25 mg of amphotericin B, then closed with one-stage suturing. The second culture confirmed the pathogen was cryptococcus neoformans. Histopathology supported chronic osteomyelitis (Figure 5). The patient was treated with fluconazole 200 mg IV twice a day for 3 d after surgery. On the 4th day, antifungal treatment was shifted to voriconazole 200 mg IV twice a day given the outcome of minimum inhibitory concentrations (4 for fluconazole vs ≤ 0.125 for voriconazole) from the second culture and sensitivity analysis.
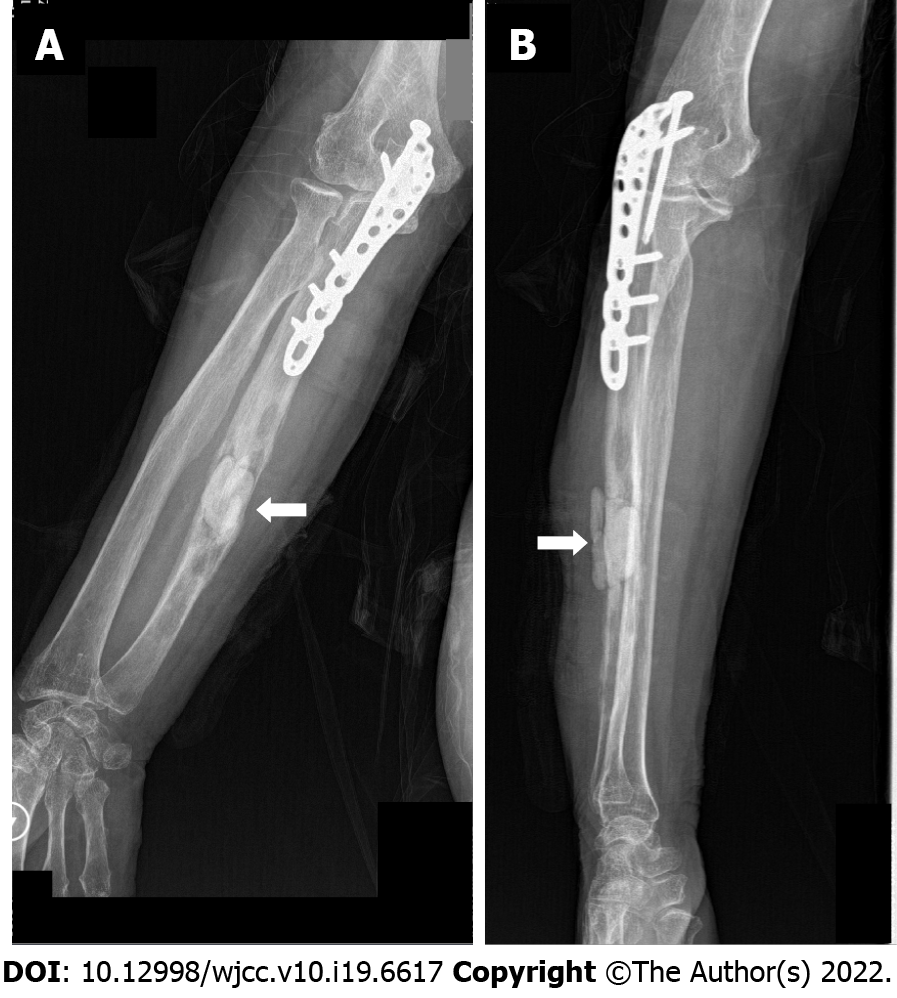
Postoperatively, the patient’s temperature was normal. Wound drainage was sampled again for culture which was later reported to be negative. An X-ray after surgery showed that the defect area of the right ulna was filled with amphotericin B-loaded cement (Figure 6A and B). On the 6th day after surgery, the patient was discharged with voriconazole 200 mg orally twice a day. One months later, in consideration of the patient’s economic condition the antifungal was switched to fluconazole 400 mg orally once a day due to decreased values of blood inflammatory markers.
Three months after surgery, the wound healed rather well (Figure 7), and an X-ray showed that the osteolytic lesions were reduced and blurred (Figure 8A and B). Ten months after surgery, X-ray revealed that the osteomyelitis had healed (Figure 9A and B). Liver and kidney functions were periodically monitored and were found to be normal.
Bone cryptococcosis is an opportunistic infection occurring mostly in immunocompromised patients with HIV infection, malignancy, solid organ transplant, connective tissue disease, and immunosuppressive therapy[12,13]. The rate of cryptococcosis occurring in immunocompetent persons is described as merely 1/100000[14]. Cryptococcal osteomyelitis mostly involves vertebrae, femur, tibia, rib, clavicle, pelvis, and humerus[15]. The ulna is a rare target. As far as we know ulna osteomyelitis due to cryptococci has been reported in only two cases, one was associated with sarcoidosis, and the other was associated with systemic lupus erythematosus[16,17]. There are two origins of cryptococcal osteomyelitis: hematogenous dissemination, and direct inoculation. In the former, the fungus spreads from primary lung source to colonize bone sites and induces infection. The latter often results due to a history of direct repetitive trauma and has been described in only four cases[18]. The present case was speculated probably to be the result of hematogenous dissemination based on (1) local swelling prior to skin ulceration and sinus formation; (2) multiple non-contiguous osteolytic lesions in the ulna; and (3) no history of direct repetitive trauma at the local infected site.
We did not find any detailed investigations in literatures as to why and how cryptococcal osteomyelitis occurs in immunocompetent patients. Basically, the occurrence of infection generally depends on pathogens virulence surpassing host immunity, but host immune status seems more crucial in cryptococcosis[14]. The present patient was found to have a slightly decreased total T-lymphocyte percentage and count, in addition to a decreased CD4+ count, but normal CD4+ and CD8+ percentage, also normal CD4/CD8, plus increased B-lymphocyte and NK cell percentage were noted. However, there are still some unclear issues in this case: Where the primary infection located? why cryptococcal osteomyelitis occurred in the mid-distal segment of the ulna but not in the proximal segment where surgery was previously undertaken?
Skeletal cryptococcosis is still a diagnostic and therapeutic challenge. Most patients present with non-specific clinical manifestations namely soft tissue swelling, pain, and tenderness, some develop skin ulceration or sinus formation[17]. Radiological findings often reveal irregular osteolytic lesions with little or no periosteal reaction, which are similar to infection with Mycobacterium tuberculosis, bacteria or malignancy[17]. Radiographic evidence often incurs a delay in the diagnosis as these features usually lag behind the clinical findings by weeks or months[19]. Specific examinations, including antigen detection, culture and histopathology, are critical for the diagnosis[20]. There is no consensus on standardized treatment for cryptococcal osteomyelitis although the Infectious Disease Society of America (IDSA) has published guidelines[21]. According to these guidelines, surgery should be performed for persistent or refractory fungal bone infection. With regard to drug treatment, the IDSA recommend amphotericin B in combination with flucytosine as induction therapy followed by consolidation and maintenance therapy with fluconazole for disseminated cryptococcosis. However, direct fluconazole treatment (400 mg or 6 mg/kg per day orally for 6-12 mo) could also be considered for isolated cryptococcal osteomyelitis in immunocompetent patients without central nervous system involvement. The duration of antifungal drug treatment should be evaluated according to clinical symptoms, imaging, and serum cryptococcal antigen[22]. Diagnosis in the present case was confirmed by twice following culture, and antifungal treatment was administered based on the results of drug sensitivity testing. In view of the requirement for accelerating local infection control and limb function recovery, surgical debridement was also performed. To date, cryptococcal osteomyelitis in this patient has healed well and her clinical symptoms and signs have completely disappeared.
Isolated cryptococcal osteomyelitis is clinically rare in immunocompetent patients. Nevertheless, it should be considered in the differential diagnosis of osteolytic lesions. Special fungal examinations and culture should be performed for definite diagnosis, and early administration of antifungal therapy can achieve better clinical outcomes.
We thank the patient for her permission to share the case information.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dam TT, Vietnam; Ho CM, Taiwan S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Maziarz EK, Perfect JR. Cryptococcosis. Infect Dis Clin North Am. 2016;30:179-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 464] [Article Influence: 51.6] [Reference Citation Analysis (0)] |
| 2. | Kwon-Chung KJ, Fraser JA, Doering TL, Wang Z, Janbon G, Idnurm A, Bahn YS. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harb Perspect Med. 2014;4:a019760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 350] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 3. | Warkentien T, Crum-Cianflone NF. An update on Cryptococcus among HIV-infected patients. Int J STD AIDS. 2010;21:679-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Jain K; Mruthyunjaya, Ravishankar R. Cryptococcal abscess and osteomyelitis of the proximal phalanx of the hand. Indian J Pathol Microbiol. 2011;54:216-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Delat R, Laheri V. Bifocal Cryptococcal Osteomyelitis in an Immunocompetent Male. J Orthop Case Rep. 2016;6:17-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Zainal AI, Wong SL, Pan KL, Wong OL, Tzar MN. Cryptococcal osteomyelitis of the femur: a case report and review of literature. Trop Biomed. 2011;28:444-449. [PubMed] |
| 7. | Wood L, Miedzinski L. Skeletal cryptococcosis: Case report and review of the literature. Can J Infect Dis. 1996;7:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Chayakulkeeree M, Perfect JR. Cryptococcosis. Infect Dis Clin North Am. 2006;20:507-544, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 274] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 9. | Chen WA, Emory CL, Graves BR. Disseminated Cryptococcal Osteomyelitis to the Hand in an Immunosuppressed Lymphoma Patient. J Hand Surg Am. 2018;43:291.e1-291.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Sang J, Yang Y, Fan Y, Wang G, Yi J, Fang W, Pan W, Xu J, Liao W. Isolated iliac cryptococcosis in an immunocompetent patient. PLoS Negl Trop Dis. 2018;12:e0006206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Qadir I, Ali F, Malik UZ, Umer M. Isolated cryptococcal osteomyelitis in an immunocompetent patient. J Infect Dev Ctries. 2011;5:669-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Joo HS, Ha JK, Hwang CJ, Lee DH, Lee CS, Cho JH. Lumbar Cryptococcal Osteomyelitis Mimicking Metastatic Tumor. Asian Spine J. 2015;9:798-802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Al-Tawfiq JA, Ghandour J. Cryptococcus neoformans abscess and osteomyelitis in an immunocompetent patient with tuberculous lymphadenitis. Infection. 2007;35:377-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 14. | Jain D, Najjar M, Azher Q, Bachuwa G. Cryptococcal sternal osteomyelitis in a healthy woman: a review of Cryptococcus neoformans. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Corral JE, Lima S, Quezada J, Samayoa B, Arathoon E. Cryptococcal osteomyelitis of the skull. Med Mycol. 2011;49:667-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Chleboun J, Nade S. Skeletal cryptococcosis. J Bone Joint Surg Am. 1977;59:509-514. [PubMed] |
| 17. | Medaris LA, Ponce B, Hyde Z, Delgado D, Ennis D, Lapidus W, Larrison M, Pappas PG. Cryptococcal osteomyelitis: a report of 5 cases and a review of the recent literature. Mycoses. 2016;59:334-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Zhou HX, Lu L, Chu T, Wang T, Cao D, Li F, Ning G, Feng S. Skeletal cryptococcosis from 1977 to 2013. Front Microbiol. 2014;5:740. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Chang WC, Tzao C, Hsu HH, Chang H, Lo CP, Chen CY. Isolated cryptococcal thoracic empyema with osteomyelitis of the rib in an immunocompetent host. J Infect. 2005;51:e117-e119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Adiwardana NS, Morás JA, Bernardo LL, Klautau GB, Queiroz W, Vidal JE. Chronic skull osteomyelitis due to Cryptococcus neoformans: first case report in an HIV-infected patient. Braz J Infect Dis. 2018;22:499-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, Harrison TS, Larsen RA, Lortholary O, Nguyen MH, Pappas PG, Powderly WG, Singh N, Sobel JD, Sorrell TC. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis. 2010;50:291-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1988] [Cited by in RCA: 1798] [Article Influence: 119.9] [Reference Citation Analysis (0)] |
| 22. | Zhang Y, Yu YS, Tang ZH, Zang GQ. Cryptococcal osteomyelitis of the scapula and rib in an immunocompetent patient. Med Mycol. 2012;50:751-755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |