Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6548
Peer-review started: October 11, 2021
First decision: March 14, 2022
Revised: March 18, 2022
Accepted: May 14, 2022
Article in press: May 14, 2022
Published online: July 6, 2022
Processing time: 256 Days and 3.9 Hours
Laparoscopic cholecystectomy (LC) and laparoscopic common bile duct exploration (LCBDE) has been widely used for management of gallbladder and common bile duct (CBD) stones. Post-operative clip migration is a rare com
A 59-year-old female was admitted to hospital because of fever and acute right upper abdominal pain. She has a history of LC and had a LCBDE surgery 2 mo ago. Physical examination revealed tenderness in the upper quadrant of right abdomen. Computed tomography scan demonstrated a high-density shadow at the distal CBD, which was considered as migrated clips. The speculation was confirmed by endoscopic retrograde cholangiopancreatography examination, and two displaced Hem-o-lok clips were removed with a stone basket. No fever or abdominal pain presented after the operation. In addition to the case report, literature regarding surgical clip migration after laparoscopic biliary surgery was reviewed and discussed.
Incidence of postoperative clip migration may be reduced by using clips properly and correctly; however, new methods should be explored to occlude cystic duct and vessels. If a patient with a past history of LC or LCBDE presents with features of sepsis and recurrent upper quadrant pain, clip migration must be considered as one of the differential diagnosis.
Core Tip: Surgical clip migration is a rare complication of laparoscopic biliary surgery. Herein, we report a case of Hem-o-lok clip migration into the common bile duct after laparoscopic cholecystectomy and laparoscopic common bile duct exploration operation which were removed by a basket in endoscopic retrograde cholangiopancreatography. Furthermore, literature regarding clip migration post-laparoscopic biliary surgery were reviewed. We suggest that the incidence of postoperative clip migration may be reduced by using clips properly and correctly; however, new methods should be explored to occlude cystic duct and vessels.
- Citation: Liu DR, Wu JH, Shi JT, Zhu HB, Li C. Hem-o-lok clip migration to the common bile duct after laparoscopic common bile duct exploration: A case report. World J Clin Cases 2022; 10(19): 6548-6554
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6548.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6548
Gallbladder stone combined with common bile duct (CBD) stone is a common disease in developed countries, with a prevalence ranging from 8% to 18%[1]. Laparoscopic cholecystectomy (LC) and laparoscopic common bile duct exploration (LCBDE) are widely used procedures for the treatment of cholelithiasis combined with choledocholithiasis. Clearly dissecting the Carlo’s triangle and properly closing the cystic artery and cystic duct are the key steps of this surgery. Hem-o-lok clips are commonly used to ligate gallbladder blood vessels and cystic ducts. Complications of LCBDE include bile leakage, stone recurrence, infection, bleeding, and postoperative clip migration.
Postoperative clip migration is a rare but well-established complication of laparoscopic biliary surgery. The clip may migrate to CBD[2-12], T-tube sinus wall[11,13], duodenum[8,14], or the pulmo
A 59-year-old woman presented to the emergency department of our hospital complaining of fever and right upper abdominal pain for 3 d.
The patient’s symptoms started 3 d ago with fever and acute right upper abdominal pain, which had worsened in the last 24 h.
The patient had a history of LC and LCBDE surgery 2 mo ago.
The patient has no personal and family history.
The patient’s temperature was 38.9 °C, heart rate was 93 bpm, respiratory rate was 18 breaths per minute, blood pressure was 105/60 mmHg, and oxygen saturation in room air was 99%. Physical examination revealed that the abdomen was soft, but tenderness was present in the right upper quadrant of abdomen without rebound tenderness.
Laboratory examination showed aspartate aminotransferase 639 U/L, alanine aminotransferase 681 U/L, and total bilirubin 74 μmol/L. Blood routine examination showed a white cell count of 16.1 × 109/L, a neutrophil percentage of 89%, and a hemoglobin of 135 g/L.
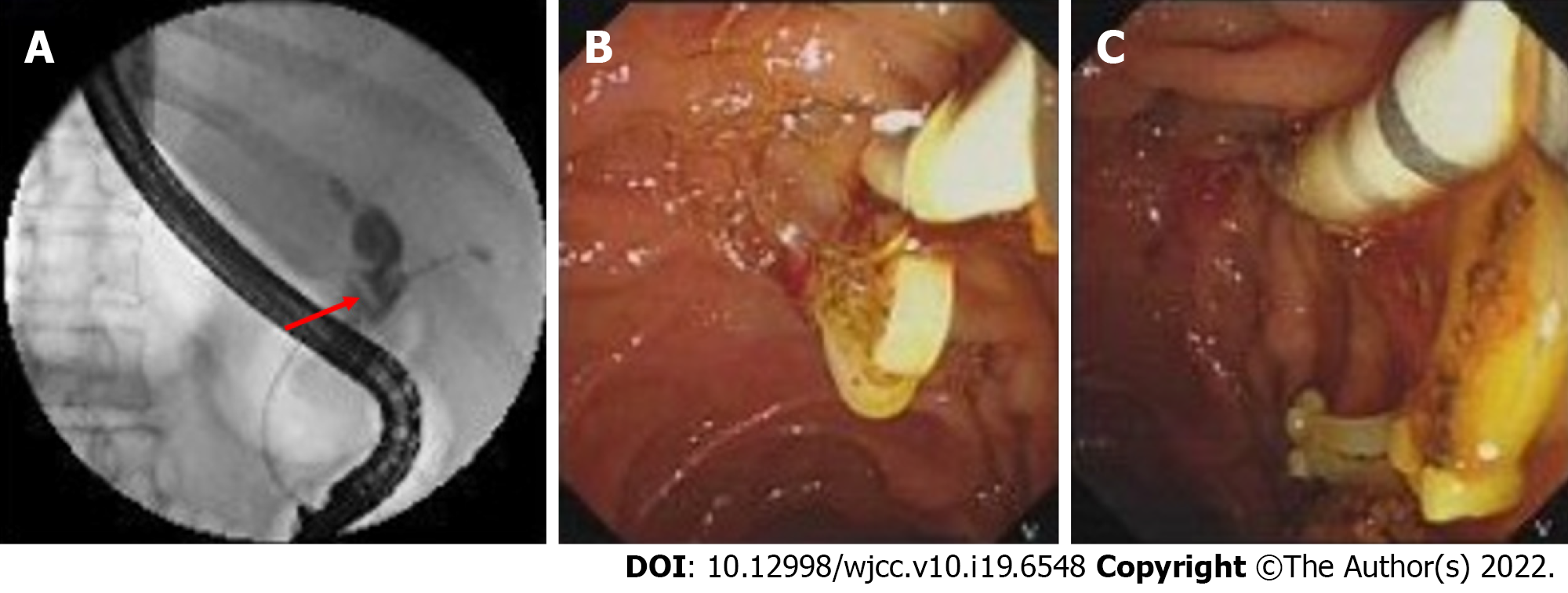
Computed tomography scan demonstrated a slightly dilated common bile duct with a high-density shadow at the distal CBD, which was considered as migrated clips (Figure 1). Therefore, endoscopic retrograde cholangiopancreatography (ERCP) was performed, which confirmed that Hem-o-lok clips migrated into the CBD (Figure 2A).
Acute cholangitis caused by migrated Hem-o-lok clips applied in the LC and LCBDE surgery.
Two displaced Hem-o-lok clips were removed by stone basket after sphincterotomy through ERCP (Figure 2B and C).
No fever or abdominal pain was presented after the operation, and the patient was discharged 3 d later in a stable condition. There was no abdominal pain, jaundice, abdominal pain, or other discomfort during the follow-up period.
Choledocholithiasis is a common disease, with an incidence increasing year by year. Comparing to open surgery, the LCBDE is safe, effective, minimally invasive, and has an faster recovery rate[16]. Advances in laparoscopy have made LC and LCBDE a widely accepted strategy for patients with gallstones and choledocholithiasis. In our practice, the Carlo's triangle was initially dissected to expose cystic duct and cystic artery, and they were separated and clipped with three and one Hem-o-lok clips, respectively. Secondly, the CBD was exposed, and the anterior aspect wall of CBD was cut with electroacupuncture 1 cm below the confluence of cystic duct and CBD, and the cholesterol crystals were removed by basket under direct view. Thirdly, a 24# Silicone T-tube was placed into the CBD, which was then sutured with a 4-0 Vicryl. Finally, the gallbladder was resected using electroacupuncture, and T-tube was set on the right abdominal through the incision of rectus abdominis. Postoperative clip migration is a rare complication of laparoscopic cystic and biliary operation, which has been occasionally presented as case report. Migrated clips in the bile duct may function as a nidus for gallstone formation, leading to biliary obstruction, acute pancreatitis, duodenal ulcer, biliary-colonic fistula, and subdiaphragmatic abscess. Any type of surgical clip has a risk of migration. If a patient with a history of receiving LC or LCBDE presents with features of recurrent upper quadrant pain, with or without sepsis or liver function test derangement, clip displacement must be considered as one of the differential diagnosis.
We searched through MEDLINE, PubMed, Scopus, Web of Science, Google Scholar, and the CNKI databases using the keywords ’clip migration and laparoscopic cholecystectomy (LC) or clip migration and laparoscopic common bile duct exploration (LCBDE)’ from 1990 to 2021. A total of 14 articles including 36 cases about clip migration after LC or LCBDE have been reported[2-15] (Table 1). Twenty-five cases received LC and LCBDE (69.4%) and 11 cases received LC (30.6%) as previous laparoscopic surgery. The age of patients ranged from 31-years-old to 83-years-old. Symptoms occurred from 1 mo to 7 years after laparoscopic surgery. Nineteen patients remained asymptomatic that were mainly diagnosed by choledochoscopy through T-tube sinus tract. The most common manifestations due to clip migration were abdominal pain, fever, and jaundice, which were similar to those of non-iatrogenic choledocholithiasis. In 27 cases, the clips wedged into the CBD (75%), while the clips became a part of T-tube sinus in 6 cases (16.7%) and the clips migrated into duodenum in 2 cases (5.6%). The types of clips include Hem-o-lok (61.1%), metallic (16.7%), and absorbable (8.3%). Initial treatment included removing clips by basket in ERCP, endoscopic removal, and observation, while surgical treatment was required in 6 cases.
| Ref. | Case number | Age in yr | Sex | Operation | Clips | Migrated site | Duration of migration in mo | Finding approach | Clinical manifestation | Treatment |
| Raoul et al[2], 1992 | 4 | 34-65 | F | LC | NA | CBD | 5-10 | NA | Abdominal pain, fever, jaundice | Removed by ERCP |
| Alberts et al[3], 1999 | 1 | 52 | M | LC + LCBDE | Metallic clips | CBD | 24 | CT | Abdominal pain | Removed by ERCP |
| Ammann et al[15], 2000 | 1 | 32 | F | LC + laparotomy | Metallic clips | Pulmonary artery | 18 | CT | Dyspnea | NA |
| Wang et al[13], 2009 | 2 | 42-73 | NA | LC + LCBDE | Metallic clips | T-tube sinus | 1 | Found in drainage bag | Asymptomatic | Drained by T-tube |
| Wang et al[13], 2009 | 1 | 42-73 | NA | LC + LCBDE | Metallic clips | Wall of T-tube sinus | 1 | T-tube choledochoscopy | Asymptomatic | Observation |
| Liu et al[4], 2012 | 8 | 35-76 | 6 M2 F | LC + LCBDE | H | CBD | 2-3 | T-tube choledochoscopy | Asymptomatic | Removed by choledochoscopy |
| Tsai et al[5], 2013 | 1 | 66 | F | LC | NA | CBD | 84 | CT | Abdominal pain, fever | Removed by ERCP |
| Seyyedmajidi et al[14], 2013 | 1 | 41 | F | LC | H | Duodenum | 8 | EDG | Abdominal pain | Removed by grasping forceps |
| Rawal[6], 2016 | 1 | 38 | F | LC | Metallic clips | CBD | 4 | Ultrasonography | Abdominal pain, fever, jaundice | Removed by ERCP |
| Qu et al[7], 2017 | 1 | 54 | F | LC + LCBDE | H | CBD | 12 | MRCP | Abdominal pain | Removed by ERCP |
| Zheng et al[8], 2018 | 1 | NA | M | LC + LCBDE | H | Duodenum | 4 | EDG | Abdominal pain | Observation |
| Zheng et al[8], 2018 | 2 | NA | NA | LC + LCBDE | H | CBD | 27, 50 | NA | Jaundice | Laparotomy operation |
| Zheng et al[8], 2018 | 3 | NA | NA | LC + LCBDE | Absorbable clips | CBD | 6 | T-tube choledochoscopy | Asymptomatic | Removed by choledochoscopy |
| Barabino et al[9], 2019 | 1 | 65 | M | LC | H | CBD | 3 | CT | Fever and abdominal pain | Roux-en-Y choledochojejunostomy |
| Roh et al[10], 2019 | 1 | 65 | M | LC | H | CBD | 13 | CT | Abdominal pain and fever | Removed by ERCP |
| Pang et al[11], 2019 | 3 | 31-83 | F | LC + LCBDE | H | Wall of T-tube sinus | 3-6 | T-tube choledochoscopy | Asymptomatic | Removed by choledochoscopy |
| Pang et al[11], 2019 | 1 | 61 | F | LC | H | CBD | NA | Ultrasound | Jaundice, abdominal pain | Roux-en-Y choledochojejunostomy |
| Pang et al[11], 2019 | 1 | 72 | F | LC + LCBDE | H | CBD | 18 | CT | Abdominal pain | Laparotomy bile duct exploration |
| Pang et al[11], 2019 | 1 | 64 | F | LC + LCBDE | H | CBD | 4 | T-tube cholangiography | Jaundice, fever | PTBD and stent implantation |
| Kihara et al[12], 2021 | 1 | 80 | M | LC | H | CBD | 36 | CT + MRCP | Asymptomatic | Laparoscopic bile duct resection and reconstruction |
The mechanism of postoperative clip migration remains controversial; however, some possible hypotheses of pathogenesis were suggested. Firstly, inappropriate application of surgical clips, including improper placement of clips and incomplete closure of cyst duct may lead to the formation of biloma, which would be reabsorbed later into the bile duct and leave the clips behind[2]. Secondly, the compression of clips to the bile duct wall caused by the surrounding structures or a pulled cystic duct during operation may result in clip corroding into the lumen of CBD[17]. Additionally, the number of clips used in surgery is also an important factor[5,18]. Thirdly, bile leakage caused by an intraoperative bile tract injury and the subsequent inflammation make surrounding tissues brittle, which may induce clips to invade into the biliary tract through the incision of CBD mechanically[17]. In addition, the pressure exerted from abdominal organ movements accelerates the process of clip migration[10,18]. Finally, the rejection response by the immune system to clips as a foreign body may also contribute to the displacement of surgical clips[4].
In order to reduce the incidence of postoperative clip migration, all technical factors in surgery should be considered. During the operation, the relationship of Calot’s triangle should be carefully confirmed, and the placement of surgical clips should not be too close to the CBD; the number of clips should be minimized, and unnecessary surgical procedures should be avoided, such as the blind application of clips to control bleeding[19]. It has also been suggested that the risk of postoperative clip migration can be lowered by using absorbable clips when compared with non-absorbable clips; however, reports about absorbable clip migration still exists[4,8], including a report by Cetta et al[20], which suggested that absorbable clips could also cause postoperative clip migration and be a nidus of stone formation. Furthermore, new vessel and duct sealing technologies such as a Harmonic scalpel can be applied as an alternative to clips in laparoscopic operation. The Harmonic scalpel is well accepted as a reasonable alternative for closure of cystic duct, which occupies the advantages of shorter operation time, fewer complications, and avoiding clip migration[21].
In summary, although postoperative clip migration is rare, it is a well-recognized phenomenon and cannot be ignored. Any type of surgical clip has a risk of displacement. Using clips properly and correctly, as well as exploring new methods to occluded cystic duct may help to reduce the incidence of postoperative clip migration. If patients with a past history of LC with or without CBD exploration present with features of sepsis and recurrent upper quadrant pain, with or without derangement of liver function test, clip migration may be considered as one of the differential diagnoses.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hori T, Japan; Kumar A, India A-Editor: Liu X S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Manes G, Paspatis G, Aabakken L, Anderloni A, Arvanitakis M, Ah-Soune P, Barthet M, Domagk D, Dumonceau JM, Gigot JF, Hritz I, Karamanolis G, Laghi A, Mariani A, Paraskeva K, Pohl J, Ponchon T, Swahn F, Ter Steege RWF, Tringali A, Vezakis A, Williams EJ, van Hooft JE. Endoscopic management of common bile duct stones: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2019;51:472-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 463] [Cited by in RCA: 373] [Article Influence: 62.2] [Reference Citation Analysis (0)] |
| 2. | Raoul JL, Bretagne JF, Siproudhis L, Heresbach D, Campion JP, Gosselin M. Cystic duct clip migration into the common bile duct: a complication of laparoscopic cholecystectomy treated by endoscopic biliary sphincterotomy. Gastrointest Endosc. 1992;38:608-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Alberts MS, Fenoglio M, Ratzer E. Recurrent common bile duct stones containing metallic clips following laparoscopic common bile duct exploration. J Laparoendosc Adv Surg Tech A. 1999;9:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Liu Y, Ji B, Wang Y, Wang G. Hem-o-lok clip found in common bile duct after laparoscopic cholecystectomy and common bile duct exploration: a clinical analysis of 8 cases. Int J Med Sci. 2012;9:225-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Tsai CH, Tsai MC, Lin CC. Unusual cause of abdominal pain after laparoscopic cholecystectomy. Gastroenterology. 2013;144:e8-e9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Rawal KK. Migration of Surgical Clips into the Common Bile Duct after Laparoscopic Cholecystectomy. Case Rep Gastroenterol. 2016;10:787-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Qu JW, Wang GY, Yuan ZQ, Li KW. Hem-o-lok Clips Migration: An Easily Neglected Complication after Laparoscopic Biliary Surgery. Case Rep Surg. 2017;2017:7279129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Zheng Y, Wang Y, Bai X, Liu D, Li F. Letter to the editor on "The cystic duct and artery were clipped using a clip applier". Nonmetal clip migration after laparoscopic cholecystectomy. Asian J Surg. 2018;41:585-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Barabino M, Luigiano C, Piccolo G, Pellicano R, Polizzi M, Giovenzana M, Santambrogio R, Pisani Ceretti A, Andreatta E, Palamara MA, Giacobbe G, Consolo P, Opocher E. Hem-o-Lok clip migration into the duodenum after laparoscopic digestive surgery: a systematic review. Minerva Chir. 2019;74:496-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Roh YJ, Kim JW, Jeon TJ, Park JY. Common bile duct stone development due to a Hem-o-lok clip migration: a rare complication of laparoscopic cholecystectomy. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Pang L, Yuan J, Zhang Y, Wang Y, Kong J. Clip-stone and T clip-sinus: A clinical analysis of six cases on migration of clips and literature review from 1997 to 2017. J Minim Access Surg. 2019;15:192-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Kihara Y, Takeda Y, Ohmura Y, Katsura Y, Shinke G, Ikeshima R, Katsuyama S, Kawai K, Hiraki M, Sugimura K, Masuzawa T, Takeno A, Hata T, Murata K. Migration of non-absorbable polymer clips in hepato-biliary-pancreatic surgery: a report of four cases. Surg Case Rep. 2021;7:183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Wang YL, Zhang GY, Wang L, Hu SY. Metallic clip migration to T-tube sinus tract after laparoscopic choledochotomy. Acta Chir Belg. 2009;109:242-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Seyyedmajidi M, Hosseini SA, Hajiebrahimi S, Vafaeimanesh J. Hem-o-Lok Clip in the First Part of Duodenum after Laparoscopic Cholecystectomy. Case Rep Gastrointest Med. 2013;2013:251634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Ammann K, Kiesenebner J, Gadenstätter M, Mathis G, Stoss F. Embolism of a metallic clip: an unusual complication following laparoscopic cholecystectomy. Dig Surg. 2000;17:542-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Grubnik VV, Tkachenko AI, Ilyashenko VV, Vorotyntseva KO. Laparoscopic common bile duct exploration versus open surgery: comparative prospective randomized trial. Surg Endosc. 2012;26:2165-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Kitamura K, Yamaguchi T, Nakatani H, Ichikawa D, Shimotsuma M, Yamane T, Takahashi T. Why do cystic duct clips migrate into the common bile duct? Lancet. 1995;346:965-966. [PubMed] |
| 18. | Chong VH, Chong CF. Biliary complications secondary to post-cholecystectomy clip migration: a review of 69 cases. J Gastrointest Surg. 2010;14:688-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 79] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Yang CP, Cao JL, Yang RR, Guo HR, Li ZH, Guo HY, Shao YC, Liu GB. Efficacy of electrocoagulation in sealing the cystic artery and cystic duct occluded with only one absorbable clip during laparoscopic cholecystectomy. J Laparoendosc Adv Surg Tech A. 2014;24:72-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Cetta F, Baldi C, Lombardo F, Monti L, Stefani P, Nuzzo G. Migration of metallic clips used during laparoscopic cholecystectomy and formation of gallstones around them: surgical implications from a prospective study. J Laparoendosc Adv Surg Tech A. 1997;7:37-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Kavlakoglu B, Pekcici R, Oral S. Verification of clipless closure of cystic duct by harmonic scalpel. J Laparoendosc Adv Surg Tech A. 2010;20:591-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |