Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6496
Peer-review started: May 6, 2021
First decision: October 16, 2021
Revised: October 26, 2021
Accepted: May 8, 2022
Article in press: May 8, 2022
Published online: July 6, 2022
Processing time: 414 Days and 2.4 Hours
Achromobacter species-associated endophthalmitis is rare and may present as either acute or chronic postoperative endophthalmitis. Delayed-onset Achromobacter species endophthalmitis appearing in acute presentation that develops more than several months after cataract surgery is very rare. Intraocular lens (IOL) removal is commonly recommended to treat Achromobacter species endophthalmitis, which is based on previous studies. Here, we report the results of surgery without IOL removal when treating patients with delayed-onset postoperative Achromobacter species endophthalmitis that developed in an acute form.
Three patients visited our ophthalmology clinic due to visual impairment that began 2-3 d earlier. They had undergone cataract surgery 5-18 mo prior. Best-corrected visual acuity of the diseased eye was between counting fingers at 30 cm to non-light perception. They showed conjunctival injection, inflammation in the anterior chamber (cell reaction 4+) and hypopyon formation. The patients were diagnosed with infectious endophthalmitis and immediately underwent pars plana vitrectomy, anterior chamber irrigation and intravitreal injection of ceftazidime and vancomycin. Before fluid infusion, a vitreous specimen was obtained. In all cases, the IOLs were not removed. Achromobacter species was detected on vitreous specimen culture. After surgery, the vitreous opacity decreased gradually and there was little retinal damage. At 1 mo after treatment, the best-corrected visual acuity had improved to 20/50 and 20/40.
Delayed onset postoperative endophthalmitis caused by Achromobacter species can appear in an acute form. All patients responded well to early vitrectomy and administration of empirical antibiotics including ceftazidime. There was no need for IOL removal during surgery.
Core Tip: Postoperative Achromobacter species endophthalmitis is rare, and it was reported that surgical treatment with intraocular lens (IOL) removal was necessary for the treatment. We experienced three cases of a very rare and unique form of Achromobacter species endophthalmitis which appeared in an acute presentation and developed more than several months after cataract surgery. Early vitrectomy with antibiotics treatment including ceftazidime resulted in a favorable prognosis. There was no need to remove the IOL unlike in previous reports. In cases of delayed onset of postoperative endophthalmitis in the acute form, Achromobacter species has to be considered as the causative strain. In these cases, the IOL removal may not be needed.
- Citation: Kim TH, Lee SJ, Nam KY. Delayed-onset endophthalmitis associated with Achromobacter species developed in acute form several months after cataract surgery: Three case reports. World J Clin Cases 2022; 10(19): 6496-6500
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6496.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6496
Endophthalmitis is sight-threatening intraocular inflammation that may be caused by an infectious organism. Postoperative endophthalmitis is generally classified as acute or chronic (with delayed-onset specification). Acute endophthalmitis is defined as infection within 6 wk after surgery whereas chronic endophthalmitis is defined as infection 6 wk or more after surgery[1]. Chronic endophthalmitis has been reported in approximately 16.7% to 33.3% of all endophthalmitis cases[2]. Approximately 41% to 63% of postoperative chronic infectious endophthalmitis cases are associated with Propionibacterium species[3]. Generally, chronic endophthalmitis shows an indolent form of inflammation.
Achromobacter species are aerobic Gram-negative rods that are distributed widely in nature; some of these species are associated with opportunistic infection[4]. Achromobacter species-associated endophthalmitis is uncommon and may present as either acute or chronic postoperative endophthalmitis. The chronic form has been reported relatively more frequently than acute endophthalmitis[5]. Delayed-onset Achromobacter species endophthalmitis appearing in acute presentation that develops more than several months after cataract surgery is very rare. Here, we report on three cases of delayed postoperative infectious endophthalmitis caused by Achromobacter species appearing in an acute form and the surgical results.
Three patients visited our ophthalmology clinic due to a visual impairment and pain.
Case 1: The patient is a 52-year-old female and the symptoms had begun 2-3 d earlier.
Case 2: The patient is a 72-year-old female and the symptoms had begun 2-3 d earlier.
Case 3: The patient is an 86-year-old female and the symptoms had begun 2-3 d earlier.
Case 1: The patient had undergone cataract surgery 18 mo prior.
Case 2: The patient had undergone cataract surgery 5 mo prior.
Case 3: The patient had undergone cataract surgery 6 mo prior.
Case 1 and case 2 had diabetes mellitus and case 1 had non-proliferative diabetic retinopathy. None of the patients had a trauma history.
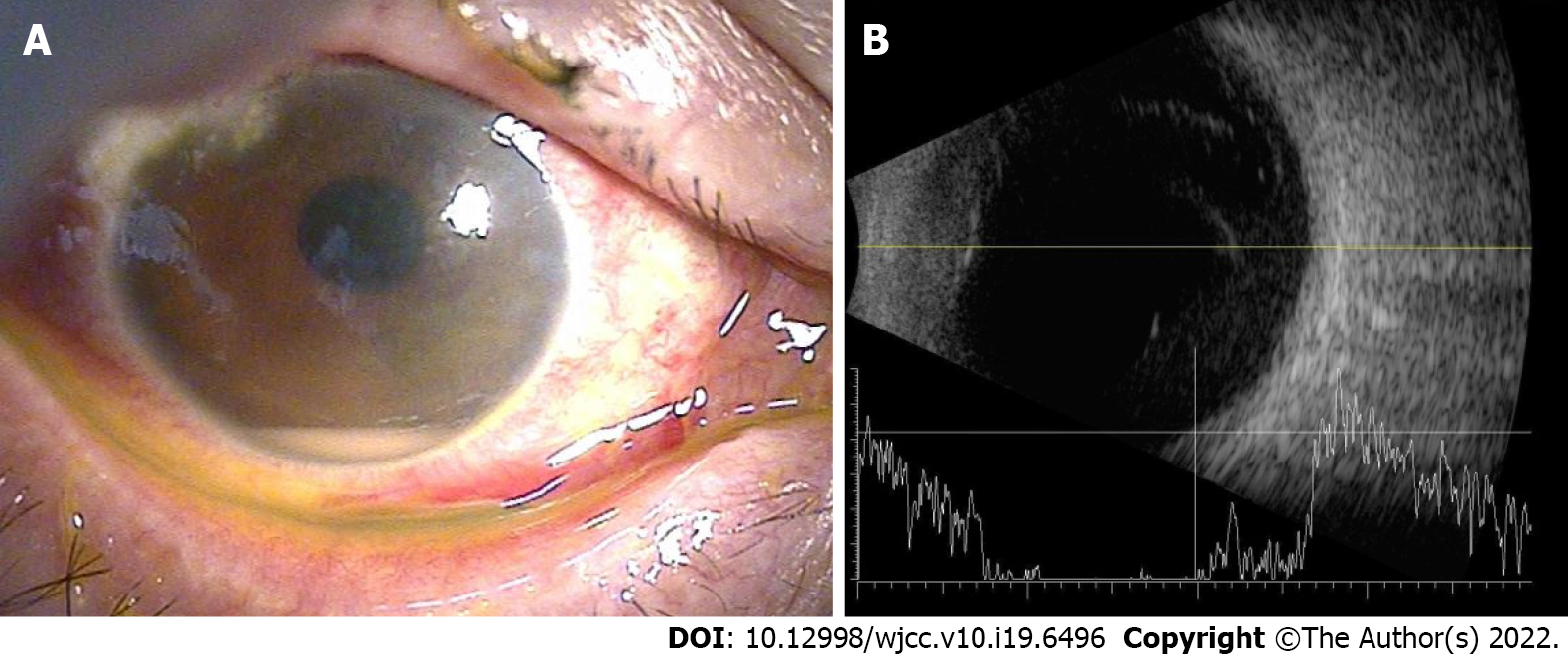
Best-corrected visual acuity of the diseased eye was between counting fingers at 30 cm to non-light perception. They all presented with conjunctival injection, inflammation in the anterior chamber (cell reaction 4+) and hypopyon formation. No leaks from a corneal or conjunctival wound were evident. There were no obvious plaques in the capsule. The retina was not visualized due to vitreous opacity (Figure 1). There was no evidence of systemic infection.
There were no special abnormalities except for mild leukocytosis.
B-scan ultrasonography showed vitreous opacity.
All of the patients were suspected of having infectious endophthalmitis.
They all underwent immediate pars plana vitrectomy, anterior chamber irrigation and intravitreal injection of ceftazidime (Tazime, Hanmi Pharm. Co., Seoul, South Korea; 2 mg/0.1 mL) and vancomycin (Hanomycin, Samjin Pharm. Co., Seoul, South Korea; 1 mg/0.1 mL). Before fluid infusion, a vitreous specimen was obtained. Cases 2 and 3 also received dexamethasone disodium phosphate (Yuhan dexamethasone disodium phosphate injection; Yuhan Corp., Seoul, South Korea; 500 μg/0.1 mL). In all cases, the intraocular lens (IOL) was not removed. After surgery, moxifloxacin 5% eye solution (Vigamox 0.5%, Novartis, Basel, Switzerland) was administered hourly and fortified topical antibiotics (vancomycin 50 mg/mL, ceftazidime 50 mg/mL) were administered every 2 h. Also, a topical steroid, loteprednol etabonate 5 mg/mL (Lotemax sterile ophthalmic suspension 0.5%, Bausch & Lomb, South Asia Inc., Gangnam-gu, South Korea) or prednisolone acetate 10 mg/mL (Pred-forte eyedrops, Allergan, Korea Ltd., Seoul, South Korea) were administered. Intravenous moxifloxacin hydrochloride 436.8 mg/250 mL (Avelox, Chong Kun Dang Pharm. Co., Seodaemun-gu, South Korea) was administered daily.
Achromobacter species were detected in vitreous specimen cultures. After surgery, hypopyon and vitreous opacity decreased gradually and there was little retinal damage. At 1 mo after treatment, the best-corrected visual acuity had improved to a level between 20/50 and 20/40. There has been no recurrence to date as of 12 mo after the vitrectomy in all cases.
Achromobacter species are aerobic Gram-negative rods that are distributed widely in nature. Some Achromobacter species have been associated with opportunistic infections in immunocompromised patients[4]. Our cases had no apparent association with an immunocompromised state despite two of the patients having diabetes mellitus.
Endophthalmitis associated with Achromobacter species is rare and may assume an acute form or chronic indolent presentation. The latter has been reported more frequently than the acute form[5]. The acute form of delayed-onset Achromobacter species endophthalmitis that develops several months after cataract surgery is very rare with only a few reports[6,7]. For the three cases of Achromobacter species-associated endophthalmitis of the current study, the inflammation developed 5-18 mo after cataract surgery and the condition resembled acute postoperative endophthalmitis. Symptoms developed suddenly with severe inflammation in the anterior chamber and hypopyon were observed.
Swart et al[7] reported that endophthalmitis caused by Achromobacter species is resistant to conservative treatments such as intravitreal antibiotic injection and anterior chamber irrigation and these treatments may result in chronic inflammation. Accordingly, they strongly recommended surgical treatment for Achromobacter-associated endophthalmitis.
Emergency vitrectomies were performed for all of our cases and empirical intravitreal vancomycin and ceftazidime, as well as topical and intravenous broad-spectrum antibiotics were administered. In a previous susceptibility study, all Achromobacter strains had resistance to aminoglycosides and most had resistance to quinolones. Reddy et al[8] suggested that ceftazidime and amikacin are the antibiotics of choice for the management of Achromobacter xylosoxidans ocular infection. Our microorganism susceptibility tests showed that the Achromobacter species are sensitive to ceftazidime and levofloxacin. The prognosis was favorable and the patients did not relapse. The early surgical approach with ceftazidime injection may be the reason for the favorable results of our cases.
For the chronic post-operative endophthalmitis, IOL removal is usually recommended. The major cause of chronic postoperative endophthalmitis is Propionibacterium acnes which is known for its chronic, indolent form of inflammation and a temporary response to corticosteroid therapy. Because Propionibacterium acnes endophthalmitis is thought to be caused by sequestration of the organism between the IOL optic and the posterior capsule, many studies have reported the necessity of capsule and IOL removal to ensure eradication of the infection source[9]. For the same reasons, in the previous reports of chronic or delayed onset Achromobacter species endophthalmitis, IOLs were removed during the surgical treat
In conclusion, we report three cases of delayed post-operative infectious endophthalmitis caused by Achromobacter species that presented as acute endophthalmitis rather than the chronic indolent form. Early vitrectomy with empirical antibiotics treatment including ceftazidime resulted in a favorable prognosis. There was no need to remove the IOL, unlike previous reports. In cases of delayed onset postoperative endophthalmitis in the acute form that occurs several months after intraocular surgery, Achromobacter species must be considered as the causative strain. In these cases, IOL removal may not be needed. However, prospective studies with more patients are required to elucidate the optimal treatment modality.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dai Q, China S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Johnson MW, Doft BH, Kelsey SF, Barza M, Wilson LA, Barr CC, Wisniewski SR. The Endophthalmitis Vitrectomy Study. Relationship between clinical presentation and microbiologic spectrum. Ophthalmology. 1997;104:261-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 111] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Shrader SK, Band JD, Lauter CB, Murphy P. The clinical spectrum of endophthalmitis: incidence, predisposing factors, and features influencing outcome. J Infect Dis. 1990;162:115-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 163] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Maalouf F, Abdulaal M, Hamam RN. Chronic postoperative endophthalmitis: a review of clinical characteristics, microbiology, treatment strategies, and outcomes. Int J Inflam. 2012;2012:313248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Spear JB, Fuhrer J, Kirby BD. Achromobacter xylosoxidans (Alcaligenes xylosoxidans subsp. xylosoxidans) bacteremia associated with a well-water source: case report and review of the literature. J Clin Microbiol. 1988;26:598-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Weissgold DJ, Kirkpatrick B, Iverson M. Acute postoperative Alcaligenes xylosoxidans endophthalmitis. Retina. 2003;23:578-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Villegas VM, Emanuelli A, Flynn HW Jr, Berrocal AM, Miller D, Kao AA, Dubovy SR, Alfonso E. Endophthalmitis caused by Achromobacter xylosoxidans after cataract surgery. Retina. 2014;34:583-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Swart J, Völker-Dieben HJ, Reichert-Thoen JW. Alcaligenes xylosoxidans endophthalmitis 8 mo after cataract extraction. Am J Ophthalmol. 1999;127:345-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Reddy AK, Garg P, Shah V, Gopinathan U. Clinical, microbiological profile and treatment outcome of ocular infections caused by Achromobacter xylosoxidans. Cornea. 2009;28:1100-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Deramo VA, Ting TD. Treatment of Propionibacterium acnes endophthalmitis. Curr Opin Ophthalmol. 2001;12:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |