Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6428
Peer-review started: October 27, 2021
First decision: March 11, 2022
Revised: March 26, 2022
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: July 6, 2022
Processing time: 239 Days and 19.9 Hours
Large gastric persimmon stones are generally resistant to standard endoscopic treatments. We applied an alternative endoscopic method using a hand-made snare for the treatment of large gastric phytobezoars.
To explore the clinical efficacy of a self-made wire loop snare to treat giant gastric persimmon stones.
A retrospective study evaluated the clinical data of 38 patients with gastroliths admitted to Taihe Hospital in Shiyan City, Hubei Province, China, between March 2015 and October 2020. The patients were divided into observation (n = 23) and control (n = 15) groups. Patients in the observation group were treated with self-made wire loop snares for lithotripsy, and patients in the control group were treated with traditional foreign body forceps, snares, injection needles, and other tools. Successful stone removal, treatment time, and hospital stay were compared.
The average operating time was significantly shorter (P < 0.001) in the observation group (53.4 min) than that in the control group (172.8 min). The average hospital stay of the observation group (5.4 d) was significantly shorter (P < 0.001) than that in the control group (10.3 d). Successful one-time treatment was significantly more frequent (P < 0.001) in the observation group (87%) than in the control group (7%).
Self-made guidewire loop snares were successfully used to treat gastrolithiasis, and were significantly more effective than foreign body forceps, snares, and other traditional methods.
Core tip: Endoscopic therapy is the first choice for gastrolithiasis. The commonly used method is cutting gastroliths into small pieces and then taking them out with foreign body forceps, snares, injection needles, and net baskets. However, these tools have insurmountable defects, such as cumbersome operation times and must be entered repeatedly, increasing the risk of damage to the patient’s throat and esophagus, and has higher treatment costs. Since October 2016, our team has treated gastric persimmon stones with self-made snares. In this study, the advantages and disadvantages of self-made snares will be analyzed and compared with those of traditional tools.
- Citation: Xu W, Liu XB, Li SB, Deng WP, Tong Q. Self-made wire loop snare successfully treats gastric persimmon stone under endoscopy. World J Clin Cases 2022; 10(19): 6428-6436
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6428.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6428
Gastrolithiasis is a condition caused by ingestion of plants, hair, or minerals, such as calcium carbonate, barium, and bismuth that cannot be digested[1] and condense to form foreign bodies, or bezoars, commonly in the stomach[2]. The incidence of gastroliths is low, with an endoscopic detection rate of approximately 0.31%[3]. Gastric bezoars can be divided into phytobezoars, animal gastroliths, medicinal gastroliths, and mixed gastroliths[4]. Phytobezoars, are the most common, account for more than 90% and have various individual causes, such as eating large amounts of fiber-rich foods, gastric dysfunction, and anatomical factors, including stenosis, diverticuli, and tumor-induced gastrointestinal obstruction[5,6].
In China, phytobezoars are often caused by eating persimmons, hawthorns, and black dates. Gastric persimmon stones are the most common gastroliths, and they are usually large and difficult to treat[7,8]. The risk factors for gastrolith occurrence include a history of gastric surgery, drinking alcohol, high blood pressure, diabetes, hypothyroidism, trichotillomania, anxiety, autumn and winter seasons, and residing in areas rich in hawthorns and persimmons[3,5]. The symptoms may include gastric outlet obstruction, abdominal pain, bloating, nausea, and vomiting[9]. Endoscopically, the condition often manifests as peptic ulcer, erosive gastritis, duodenitis, and reflux esophagitis[5]. Common complications include gastric ulcer, gastric perforation, and intestinal obstruction[9,10].
Endoscopic surgery is the preferred treatment for gastrolithiasis[10], and it commonly involves lithotripsy for cutting gastroliths into small pieces that are subsequently removed with foreign body forceps, snares, injection needles, net baskets, dual knives, electric snares, and guidewires[11]. Those tools have disadvantages such as operation times that are prolonged or difficult because of repeated entry and the risk of damage to the patient’s throat and esophagus. A long operating time increases pain, and has high treatment costs[12]. Foreign body forceps that can be easily used to remove gastric persimmon stones have recently been introduced, but the equipment is expensive and most medical institutions have not purchased them. Hence, their use is currently limited[1].
Since October 2016, our team has treated gastric persimmon stones with self-made snares. In this study, the advantages and disadvantages of self-made snares were evaluated and compared with traditional tools.
This retrospective study collected the clinical data of patients with gastrolithiasis diagnosed by gastroscopy at the Digestive Endoscopy Center of Taihe Hospital, Shiyan City, Hubei Province, China between March 2015 and October 2020. The enrolled patients were divided into an observation group (n = 23) and a control group (n = 15). The patients in the observation group underwent endoscopic lithotripsy between October 2016 October 2020 with self-made guidewire loop snares. The patients in the control group were treated between March 2015 and September 2016 by lithotripsy with traditional foreign body forceps, snares, or injection needles. The study protocol was reviewed and approved by Taihe Hospital’s Ethics Committee, and written consent was obtained from all patients who participated. The study was conducted following the ethical guidelines of the Helsinki Declaration.
Inclusion criteria: Patients with a history of eating persimmons, evaluated by gastroscopy, computed tomography (CT), magnetic resonance imaging (MRI), and other modalities, and finally diagnosed with gastrolithiasis that involved large gastric persimmon stones of > 4 cm in diameter, were assessed for study inclusion. Study enrollment required gastroscopy showing successful removal of the persimmon stone from the stomach and the absence of residue. The study participants were considered cured and discharged.
Exclusion criteria: Patients with stones that were not persimmon stones, persimmon stones < 4 cm diameter, not treated endoscopically, with intestinal obstruction, gastric perforation, and other complications, lost to follow-up or with incomplete data, and those not considered appropriate for inclusion by the investigators were excluded.
Clinical information: Patient sex, age, underlying diseases, main clinical symptoms, size and location of the gastric persimmon stones, and other endoscopy findings (e.g., peptic ulcer, reflux esophagitis), number of gastroscopy procedures, average operation time, and average hospital stay were included in the analysis.
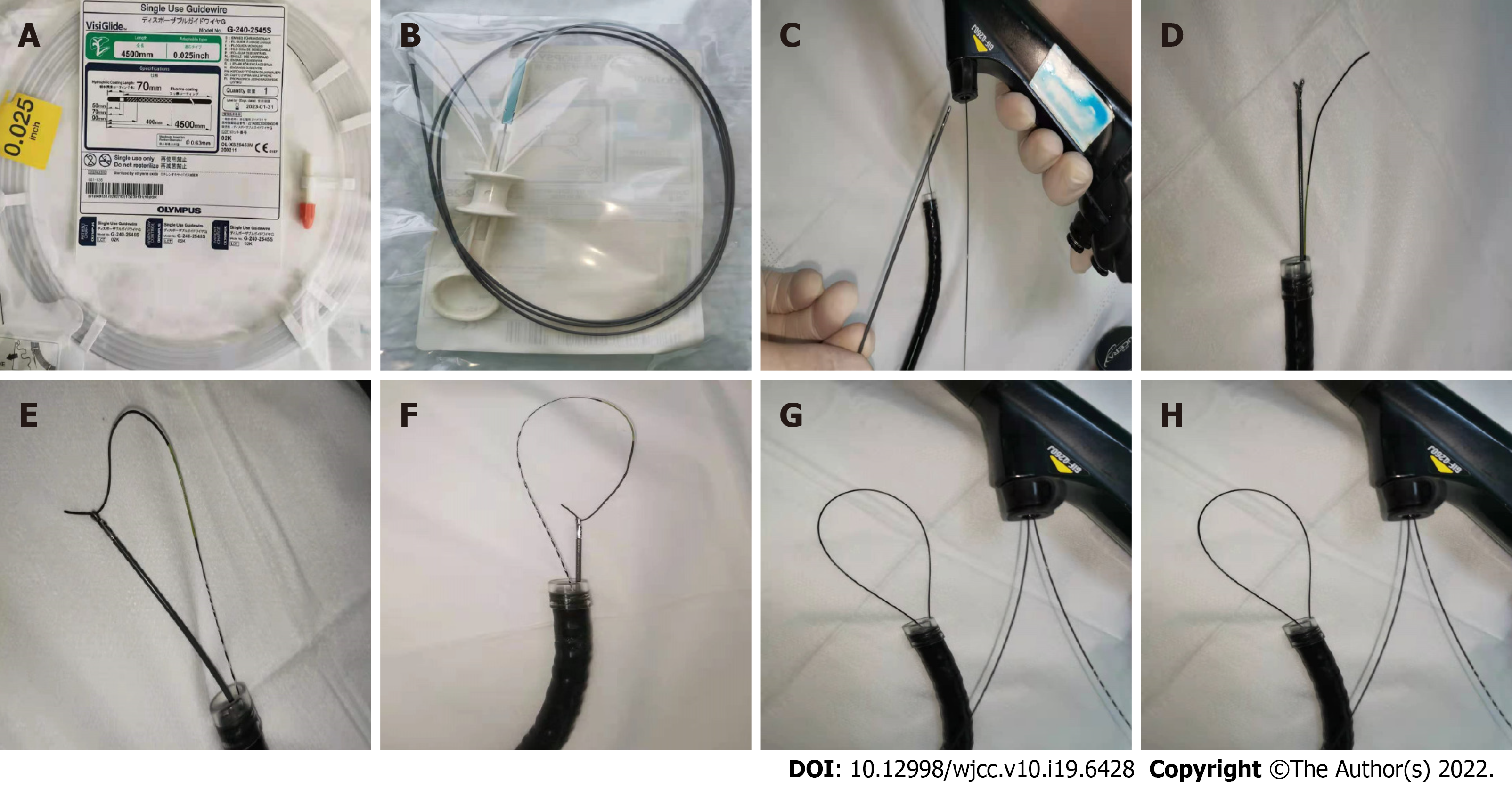
A 0.025-inch diameter guidewire (Single-Use Guidewire; Olympus, Tokyo, Japan) (Figure 1A) was inserted into the biopsy tunnel of the gastroscope operation site and passed through the end of the gastroscope lens. An ultrafine endoscopic biopsy forceps (FB-231K; Olympus) (Figure 1B) was inserted into the biopsy channel. A transparent cap was placed on the front end of the gastroscope. The guidewire was passed through the lateral orifice at the head end of the biopsy forceps. The biopsy forceps were closed to clamp the guidewire, and the force was controlled to prevent the guidewire from detaching during traction or damage to the guidewire because of excessive force. The biopsy forceps were pulled back until the guidewire was pulled out from the biopsy channel. During the procedure, the guidewire was delivered into the biopsy channel synchronously to maintain an “O” shape of the guidewire loop snare extending out of the biopsy channel. Guidewire loop snares of different diameters were prepared (Figure 1C–H).
Preoperative preparation: At 48 h before surgery, the patients in both groups were instructed to drink 100–200 mL of Coca-Cola once every 6 h. At 12 h before surgery, they began fasting. The patient was anesthetized with 10 mg intramuscular anisodamine, 10 mg intravenous diazepam, and 50 mg intramuscular pethidine.
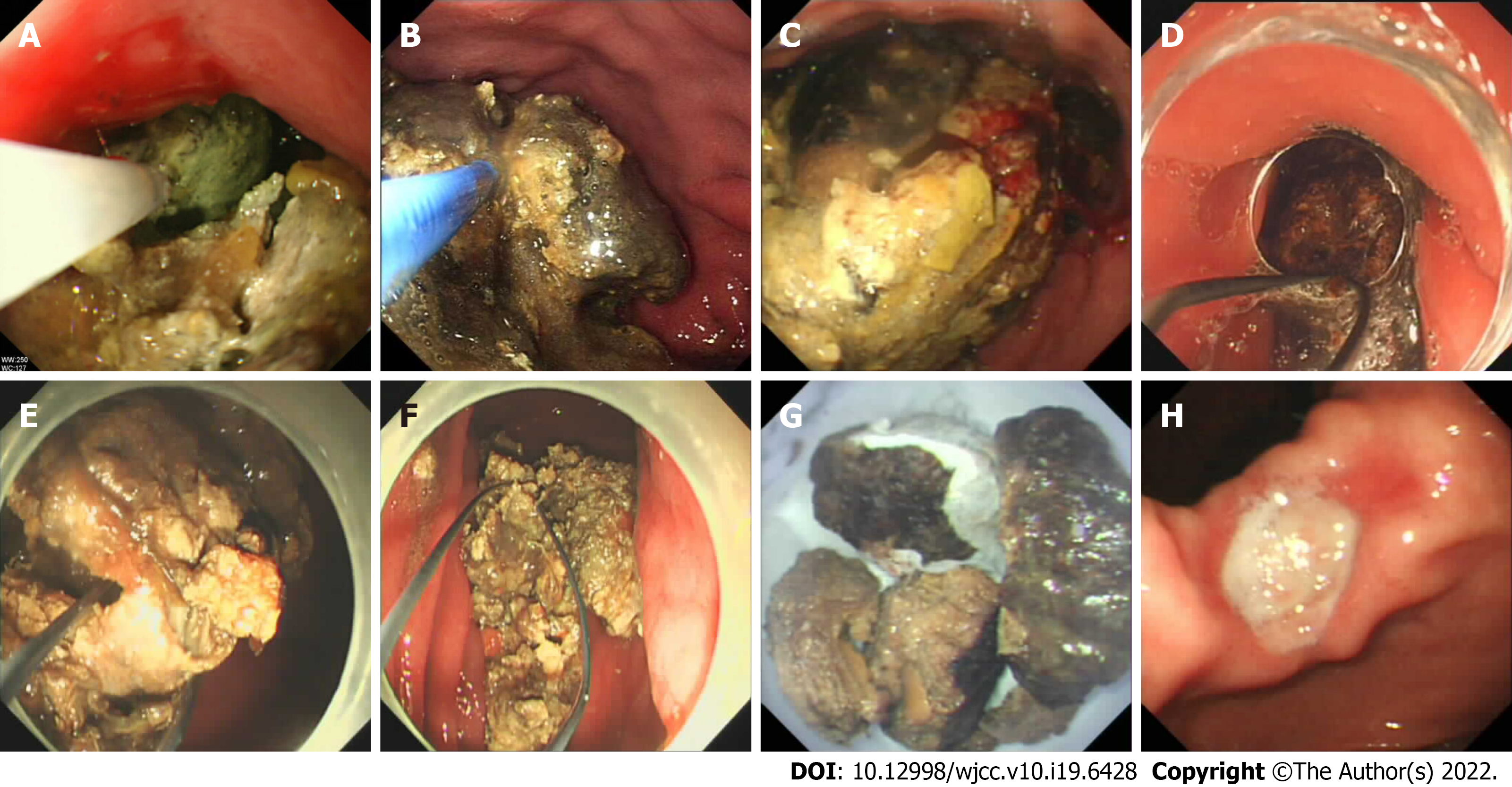
Control group: A transparent cap was installed on the front end of the gastroscope and introduced to the stomach with the endoscope. The persimmon stone was gradually mashed, layer by layer, with foreign body forceps (FG-44NR-1; Olympus) (Figure 2A), snares (NOE342216-C; Olympus) (Figure 2B), and injection needles (NM-4L-1; Olympus) (Figure 2A and B). A wire basket was used to remove large pieces, and smaller pieces were discharged from the intestines. After treatment, the patients were instructed to consume Coca-Cola orally, following the same routine as the above. After surgery, patients were instructed to fast for 48 h after receiving gastroscopy. When residues were found, the above method for lithotripsy treatment was conducted and repeated until the persimmon stone completely disappeared.
Observation group: Before treatment, a self-made wire loop snare was used to install a transparent cap (D-201; Olympus) on the front end of the gastroscope (GIF260; Olympus). Both ends of the guidewire were tightened, and the guidewire loop on the lens end was retracted into the transparent cap. The endoscope entered the stomach. After the persimmon stone was found, the guidewire was positioned so that the diameter of the loop at the lens end was larger than the diameter of the persimmon stone. The persimmon stone was held and positioned in the greater curvature of the stomach. One end of the guidewire (A) of the operating part was fixed, the other end of the guidewire (B) was tightened. After the side of the guidewire was embedded in the persimmon stone, the B end was fixed and the A end was tightened. The guidewire was embedded on the other side of the persimmon stone. At that stage, the persimmon stone was divided into two parts. The procedures were repeated until the gastroliths were cut into small pieces with diameters ≤ 1.5 cm (Figure 2C–H). They smoothed the intestine, facilitated the removal of the cut gastrolith, and prevented intestinal obstruction. When the diameter of a gastric persimmon stone was extremely large, the surgery was performed in several steps to prevent repeated access to the endoscope that reduced the risk of throat, esophagus, and stomach wall damage, and the risk of anesthesia. After completing the treatment, fasting was continued, but the patients were instructed to drink 100–200 mL Coca-Cola every 6 h. After 48 h, gastroscopy was performed to determine whether persimmon stones remained in the stomach and lithotripsy was repeated if residues were found.
The statistical analysis was performed with SPSS software (version 22.0; IBM Corp., Armonk, NY, United States). Categorical variables were reported as numbers and percentages (%). Between-group differences were compared with χ2 tests. Continuous variables were reported as means ± SD, and between-group differences were compared by t-tests. P < 0.05 was considered statistically significant.
The characteristics of the 38 patients included in the study are shown in Table 1. The observation group included 23 cases, with a median age of 63 (31–79) years and 74% males. The control group included 15 cases, with a median age of 58 (22–61) years and 67% females. The age and sex composition of the two groups and the presence of abdominal pain, abdominal distension, and vomiting were similar. Differences in melena and histories of hypertension, diabetes, coronary heart disease, and partial gastrectomy were not statistically significant.
| Variable | Observational group, n = 23 | Control group, n = 15 | Stats | P value |
| Male sex | 17 (73.9) | 10 (66.7) | 0.013 | 0.91 |
| Median age (yr), mean (range) | 63 (31–79) | 58 (22–61) | 2.30 | 0.49 |
| Main complaint | ||||
| Epigastric pain | 23 (100) | 14 (93.3) | 0.048 | 0.83 |
| Distention | 12 (52.1) | 8 (53.3) | 0.005 | 0.94 |
| Vomiting | 5 (21.7) | 3 (20.0) | 0.017 | 0.90 |
| Melena | 2 (8.7) | 2 (13.3) | 0.203 | 0.65 |
| Comorbidity | ||||
| Hypertension | 21 (91.3) | 11 (73.3) | 1.061 | 0.30 |
| Diabetes mellitus | 6 (26.1) | 2 (13.3) | 0.287 | 0.59 |
| Coronary heart disease | 8 (34.8) | 2 (13.3) | 1.190 | 0.28 |
| History of partial gastrectomy | 3 (13.0) | 1 (6.7) | 0.007 | 0.93 |
| Gastric phytobezoars location | 1.022 | 0.80 | ||
| Funds | 4 (17.4) | 3 (20.0) | – | – |
| Body | 11 (47.8) | 9 (60.0) | – | – |
| Antrum | 5 (21.7) | 2 (13.3) | – | – |
| Gastric remnant | 3 (13.0) | 1 (6.7) | – | – |
| Phytobezoar longest diameter in cm, mean ± SD (range) | 5.6 ± 1.7 (4–9) | 5.5 ± 1.4 (4–8) | 0.190 | 0.721 |
| Other endoscopic findings | 0.394 | 0.941 | ||
| Gastric ulcer | 18 (78.3) | 11 (73.3) | – | – |
| Duodenal ulcer | 2 (8.7) | 1 (6.7) | – | – |
| Reflux esophagitis | 2 (8.7) | 1 (6.7) | – | – |
| Other1 | 3 (13.0) | 3 (20) | – | – |
| Number of passes | 36.212 | < 0.001 | ||
| 1 | 20 | 1 | – | – |
| 2 | 3 | 2 | – | – |
| 3 | 0 | 7 | – | – |
| 4 | 0 | 4 | – | – |
| 5 | 0 | 1 | – | – |
| Operating time in min | 53.4 ± 7.2 | 172.8 ± 13.5 | 35.536 | < 0.001 |
| Hospital stay in d | 5.4 ± 1.2 | 10.3 ± 1.8 | 10.095 | < 0.001 |
The locations of gastric persimmon stones in the two groups were similar. In the observation group, 11 (47.8%) were in the gastric corpus, four (17.4%) in the gastric fundus, five (21.7%) in the gastric antrum, and three (13.0%) in the remnant stomach. In the control group, nine (60.0%) stones were in the gastric corpus, three (20.0%) in the gastric fundus, two (13.3%) were in the gastric antrum, and one (6.7%) in the remnant stomach. The persimmon stones in the two groups were similar in size—between 4 and 9 (5.6 ± 1.7) cm in the observation group and 4 and 8 (5.5 ± 1.4) cm in the control group.
The frequencies of digestive tract complications of persimmon stones were similar in both study groups. Concurrent stomach ulcers had the highest incidence (78.3% vs 73.3%), followed by duodenal ulcers (8.7% vs 6.7%) and esophagitis (8.7% vs 6.7%), The differences were not significant. During gastroscopy, a small number of patients were found to have other diseases, such as pyloric obstruction and gastric cancer.
The 23 patients in the observation group were treated by endoscopic lithotripsy using self-made guidewire loop snares. Before discharge, all gastroliths had been emptied through the gastroscope and finally discharged through the intestine. The treatment success rate was 100%. In the 15 control group patients, traditional tools were used for lithotripsy or stone removal, with seven being treated with snares and wire baskets, three with snares and foreign-body forceps, three with injection needles and foreign-body forceps, and two with injection needles and wire baskets. No gastric stones were found before discharge. The success rate of the treatment was also 100%. In the observation group, the first treatment was successful in 20 patients, and three patients needed a second treatment. In the control group, the first treatment was successful in only one patient. Two patients required a second treatment, seven required three treatments, four required four treatments, and one required five treatments. The one-time treatment success rate of the observation group was significantly higher than that of the control group (86.96% vs 6.67%, P < 0.001).
The average operating time of the observation group was significantly lower than that of the control group (53.4 min vs 172.8 min), and the average hospital stay was significantly shorter than that of the control group (5.4 d vs 10.3 d, P < 0.001).
Patients with subtotal gastrectomy, vagus nerve amputation, or gastroparesis syndrome are prone to gastrolithiasis, which may be associated with factors like low gastric acid, gastric emptying disorder, and pyloric dysfunction that lead to conditions in which undigested food remains in the stomach for a long time[1]. In our study, 21.0% (8/38) of the patients had diabetes and 10.5% (4/38) had a history of gastric surgery, indicating that the formation of gastroliths was associated with physiological disorders of the stomach.
Gastrolithiasis is most often caused by eating the flesh of persimmons or dried persimmons, which contain highly astringent tannic acid, pectin, and other substances. In the presence of gastric acid, they combine with food proteins to form water-insoluble tannins that are deposited in the stomach and then bind to nondigestible plant fibers to form gastric stones[4]. Friction of the gastric stones against the stomach wall stimulates secretion of gastric acid, while the weight of the stones compresses the stomach wall. The formation of stones can lead to avascular necrosis of local tissues, gastric mucosal erosion, ulcers, bleeding, and perforation. Repeated stimulation can cause pyloric scar stenosis[8]. If a diagnosis of gastrolithiasis is confirmed, then the patient should be actively treated. Gastric ulcers are the most common complication of gastrolithiasis, with an incidence rate of approximately 60%–70%[8], which is consistent with the 63.2% (24/38) in this study. The results indicate that the upper digestive tract should be carefully evaluated after successful stone removal, especially the stomach, to check whether there are some other lesions.
Treatment of plant-based gastroliths include stone dissolution, endoscopy, and surgery. Litholytic treatments include sodium bicarbonate solution and a variety of protease preparations that can soften, shrink or dissolve gastric stones as a single treatment, or as an auxiliary treatment before and after endoscopic treatment[13]. If drugs and endoscopy are not effective, patients need surgery. The use of Coca-Cola to treat gastroliths is a simple and easy solution that was first reported by Ladas et al[14] in 2002. Subsequent studies have reported the dissolution and disappearance of gastroliths by drinking or nasogastric feeding of Coca-Cola[15]. Multiple injections of Coca-Cola into the gastrolith have been performed to make the gastrolith soft enough for mechanical crushing[15]. Gastrolith fragments can be quickly disintegrated using Coca-Cola. The ingredients in Coca-Cola that dissolve plant-based gastroliths and the dissolution mechanism are currently unclear. The effect may depend upon the acidification of gastric contents by Coca-Cola, which has a pH of 2.6, and the release of CO2 bubbles that fragment gastroliths[14].
Endoscopic mechanical lithotripsy is the primary method of treating large gastroliths. It involves the use of foreign body forceps, three-jaw forceps, injection needles, snares, net baskets, and other tools to cut gastroliths into small pieces under the direct view of the gastroscope. The pieces are then taken out or discharged through the intestines. Some hospitals use lasers or high-frequency electric lithotripsy simultaneously[1,13]. We used self-made wire loop snares to crush the stones mechanically. The treatment efficiency was significantly improved compared with controls, and the mean number of gastroscopy treatments for successful removal decreased from 3.13 to 1.13. The mean procedure time decreased by 119.4 min, and hospital stay decreased by 4.9 d.
Commercially available snares currently have small diameters and cannot completely surround stones to complete the cutting, and must be combined with foreign body forceps, injection needles, and other instruments. After the surface of the persimmon stone has been crushed, repeated cutting makes the persimmon stone smaller, but in this study, the operating time was long, and the treatment efficiency was low. Moreover, repeated access to the lens increases the risk of damage to the throat, esophagus, and stomach wall tissues. The snare wire is easily deformed during the cutting process[16]. In the control group, the patients needed three to five lithotripsy treatments to be cured, which increased the cost of treatment. The size of the self-made guidewire loop snare was adjustable, the persimmon stone was completely covered, cut into two pieces, then repeatedly cut into countless small pieces, and finally discharged through the intestine. In all 23 patients in the observation group, we cut the persimmon stone into countless small pieces, and during one procedure in 20 patients. Gastroscopy performed on the next day found that persimmon stones were completely removed from the stomach. Compared with traditional tools, the self-made guidewire loop snares significantly shortened the endoscopic lithotripsy time, reduced equipment-associated damage, shortened the hospital stay, and saved medical costs.
We have several points of experience with this technology: (1) Before surgery, 48 h of drinking Coca-Cola softened the surface of the persimmon stone, and thus made it easier to trap the persimmon stone with for the guidewire loop snare[15]. The softened persimmon stones were then easy to cut. Fasting and drinking Coca-Cola were recommended after lithotripsy, rechecking was performed by gastroscopy after 24 h; (2) Before lithotripsy, a transparent cap was placed on the front end of the gastroscope, and while cutting the persimmon stone, damage to the lens by the stone was prevented by maintaining a certain distance between it and the lens. This procedure ensured a clear endoscope lens for the entire operation; (3) While cutting the stone, the plastic-coated guidewire repeatedly rubbed against the stone, promoted peeling, and facilitated the operation. Using a bare guidewire with no plastic coating on the surface is recommended; (4) Before trapping the persimmon stone, the gastric cavity was filled with gas to ensure that the gastric mucosal folds were not trapped behind the stone in the blind area of the visual field. However, excessive inflation can cause cardia mucosal tears and postoperative abdominal distension. After the persimmon stone was trapped, it was moved to determine whether the snare had trapped the gastric mucosa; (5) In the cutting process, tightening one end of the guidewire after the other was better than simultaneously tightening both ends. When cutting was almost complete, the force needed to tighten the guidewire was reduced. When a miss was felt, tightening of the guidewire was stopped. This step prevented the guidewire loop from being pulled into the biopsy forceps and damaging the lens and the forceps; and (6) Intestinal obstruction was prevented by cutting the persimmon stones into small pieces with widths of less than 1.5 cm. In 23 patients, small pieces of persimmon stones were safely discharged through the intestines, and no intestinal obstructions occurred.
However, the study had some limitations. The sample size was small, and the retrospective design did not allow controlling for factors that could confound the comparison. A prospective randomized controlled study with a larger sample size is needed to verify the safety and effectiveness of these self-made wire loop snares.
Self-made guidewire loop snares were successfully used to treat gastrolithiasis, and were significantly more effective than foreign body forceps, snares, and other traditional methods.
Two of the most important disadvantages of endoscopic treatment are the length of the procedure time and the risk of aspiration. Existing endoscopic devices are inadequate for large gastric phytobezars; therefore, our team invented a hand-made tool to solve those problems.
Large gastric persimmon stones are generally resistant to standard endoscopic treatments. As such, a novel, better solution is needed.
The study objective was to explore the clinical efficacy of self-made wire loop snares in treating giant gastric persimmon stones.
The clinical data of 38 patients with gastroliths and who were treated by endoscopic lithotripsy at Taihe Hospital were evaluated retrospectively. The study included an observation group of 23 patients treated with self-made wire loop snares and a control group of 15 patients treated with traditional foreign body forceps, snares, injection needles, and other tools. The rates of successful stone removal, the time needed to perform the treatment, and the length of the hospital stay, and medical costs were compared.
The self-made guidewire loop snares significantly shortened the lithotripsy time under gastroscopy, reduced equipment-associated damage, shortened hospital stay, and saved medical costs.
We reported our experience using self-made guidewire loop snares for the endoscopic treatment of large gastric phytobezoars. The two main advantages of our snare are that the sheath and guidewire can be readily available in almost every endoscopy unit and the procedure can be performed with a standard gastroscope. Furthermore, the guidewire can be easily guided through the sheath to capture the bezoar, resulting in a significantly shorter procedure time than needed with other methods.
The self-made snares successfully grasped large-sized gastric bezoars and fragmented them into small pieces in all patients. A prospective randomized controlled study and a larger patient sample is needed to confirm the safety and effectiveness of the self-made wire loop snare.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang KK, United States S-Editor: Fan JR L-Editor: Kerr C P-Editor: Fan JR
| 1. | Shah M, Wan DQ, Liu Y, Rhoads JM. Gastric Bezoar: Retrieve it, Leave it, or Disbelieve it? J Pediatr Gastroenterol Nutr. 2021;72:e31-e36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Aryannezhad S, Sadeghian Y, Shapoori P, Valizadeh M, Barzin M. A rare case report of late-onset phytobezoar formation following laparoscopic sleeve gastrectomy: delayed redo bariatric surgery. BMC Surg. 2021;21:254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Liu LN, Wang L, Jia SJ, Wang P. Clinical Features, Risk Factors, and Endoscopic Treatment of Bezoars: A Retrospective Analysis from a Single Center in Northern China. Med Sci Monit. 2020;26:e926539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Paschos KA, Chatzigeorgiadis A. Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol. 2019;32:224-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 5. | Hemmasi G, Zanganeh E, Hosseini SA, Alimadadi M, Ahmadi A, Hajiebrahimi S, Seyyedmajidi M. Risk factors, endoscopic findings, and treatments in upper gastrointestinal bezoars: multi-center experience in Iran. Gastroenterol Hepatol Bed Bench. 2021;14:160-164. [PubMed] |
| 6. | Chen WW, Gao RL, Liu LS, Zhu ML, Wang W, Wang YJ, Wu ZS, Li HJ, Gu DF, Yang YJ, Zheng Z, Jiang LX, Hu SS. China cardiovascular diseases report 2015: a summary. J Geriatr Cardiol. 2017;14:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 142] [Reference Citation Analysis (1)] |
| 7. | Tan F, Mo H, He X, Pei H. An unusual case of gastric outlet obstruction caused by multiple giant persimmon phytobezoars. Gastroenterol Rep (Oxf). 2019;7:74-76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Lin L, Wang C, Wu J, Liu K, Liu H, Wei N, Lin W, Jiang G, Tai W, Su H. Gastric phytobezoars: the therapeutic experience of 63 patients in Northern China. Rev Esp Enferm Dig. 2020;112:12-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Mejri A, Trigui E. Phytobezoar: A train can hide another. Int J Surg Case Rep. 2021;81:105814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Wang TT, He JJ, Liu J, Chen WW, Chen CW. Acute pancreatitis and small bowel obstruction caused by a migratory gastric bezoar after dissolution therapy: A case report. World J Clin Cases. 2021;9:3114-3119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Jinushi R, Yano T, Imamura N, Ishii N. Endoscopic treatment for a giant gastric bezoar: Sequential use of electrohydraulic lithotripsy, alligator forceps, and snares. JGH Open. 2021;5:522-524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Blam ME, Lichtenstein GR. A new endoscopic technique for the removal of gastric phytobezoars. Gastrointest Endosc. 2000;52:404-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Özsoy Z, Okan İ. Treatment of phytobezoars: Tailoring management to diverse presentations. Turk J Surg. 2018;34:33-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Ladas SD, Triantafyllou K, Tzathas C, Tassios P, Rokkas T, Raptis SA. Gastric phytobezoars may be treated by nasogastric Coca-Cola lavage. Eur J Gastroenterol Hepatol. 2002;14:801-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 94] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Lee BJ, Park JJ, Chun HJ, Kim JH, Yeon JE, Jeen YT, Kim JS, Byun KS, Lee SW, Choi JH, Kim CD, Ryu HS, Bak YT. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol. 2009;15:2265-2269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Misra SP, Dwivedi M, Misra V. Endoscopic management of a new entity-plastobezoar: a case report and review of literature. World J Gastroenterol. 2006;12:6730-6733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |