Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6406
Peer-review started: July 23, 2021
First decision: September 2, 2021
Revised: September 10, 2021
Accepted: April 21, 2022
Article in press: April 21, 2022
Published online: July 6, 2022
Processing time: 335 Days and 23.9 Hours
Nearly 10% of patients undergoing primary total knee arthroplasty (TKA) have valgus deformity (VD) of the knee. For severe VD of the knee, a more lateral structural release is needed to achieve balance between medial and lateral space and neutral femorotibial mechanical axis (FTMA), which is challenging and technical.
To introduce a new surgical technique of resection, soft tissue release, and FTMA for Ranawat type-II VD with a 5-year follow-up.
A retrospective study was conducted on patients who underwent TKA from December 2011 to December 2014. Hip-knee-ankle (HKA), range of motion (ROM), Oxford knee score (OKS), and knee society score (KSS) were used to assess the joint activity of patients in the new theory TKA group (NT-TKA) and were compared with those of the conventional TKA group (C-TKA).
A total of 103 people (103 knees) were included in this study, including 42 patients with an average follow-up period of 83 mo in the C-TKA group and 61 patients with an average follow-up period of 76 mo in the NT-TKA group. Six patients had constrained prosthesis, one had common peroneal nerve injury, and two had joint instability in the C-TKA group, but none of these occurred in the NT-TKA group. There were significant statistical differences in constrained prosthesis usage and complications between the groups (P = 0.002 and P = 0.034, respectively). The KSS at 1 mo post-operation for the C-TKA and NT-TKA groups were 11.2 ± 3.8 and 13.3 ± 2.9, respectively, with a significant difference (P = 0.007). However, the data of HKA, ROM, OKS KSS, and prosthesis survival rate were insignificant (P > 0.05) in both the preoperative and follow-up periods.
Adopting 5°-7° valgus cut angle for VD and sacrificing 2° neutral FTMA for severe VD which cannot be completely corrected during TKA can reduce the need for soft tissue release, maintain early joint stability, reduce the use of constrained prostheses, and minimize postoperative complications.
Core Tip: This study aimed to provide a new theory of surgical resection, soft tissue release, and femorotibial mechanical axis (FTMA) for Ranawat type-II valgus deformity (VD) of the knee using bone and soft tissue co-balance theory to reduce the complexity of the surgery and to improve postoperative outcomes. Bone and soft tissue balance is equally important in a total knee arthroplasty procedure. Adopting 5°-7° valgus cut angle for VD and sacrificing 2° neutral FTMA for severe VD during surgery can reduce the need for soft tissue release, maintain joint stability, and abrogate the use of constrained prostheses while minimizing postoperative complications.
- Citation: Lv SJ, Wang XJ, Huang JF, Mao Q, He BJ, Tong PJ. Total knee arthroplasty in Ranawat II valgus deformity with enlarged femoral valgus cut angle: A new technique to achieve balanced gap. World J Clin Cases 2022; 10(19): 6406-6416
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6406.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6406
Nearly 10% of patients undergoing primary total knee arthroplasty (TKA) have valgus deformity (VD) of the knee. These deformities are commonly accompanied by the lateral femur and tibia bone defect, lateral soft tissue tightening, and medial soft-tissue laxity. Ranawat et al[1] pioneered the classification of VD of the knee into three types: I, II, and III. TKA is indicated for type I and can be corrected with relative ease. Type II is more challenging and technical, and type III usually requires a constrained prosthesis.
To improve clinical outcomes, several studies have described the surgical approach, soft tissue balance, and resection. Rossi et al[2] proposed that a valgus cut angle (VCA) of 3° is a favorable approach. However, the femoral condyle requires greater medial than lateral resection to restore the femorotibial mechanical axis (FTMA), which may result in a hypoplastic lateral condyle[3]. Lateral soft tissue releases are required to balance a VD of the knee. Moreover, there are concerns that excessive soft tissue release could result in joint instability, and therefore, reducing the destruction of lateral soft tissue to protect joint stability is of great significance during TKA. Neutral FTMA, as one of the gold standards for TKA, is universally accepted to improve both postoperative knee function and prosthesis survival rate. However, some scholars[4,5] proposed that the alignment position of the FTMA may have little effect on TKA and the prosthesis survival rate. For severe VD of the knee, more soft tissue destruction and even restrictive prosthesis may be required to achieve neutral FTMA. Therefore, the balance between osteotomy, soft tissue release, and FTMA is very critical and valuable.
This study aimed to provide a new theory of surgical resection, soft tissue release, and FTMA for Ranawat type-II VD of the knee using the theory of bone and soft tissue co-balance to reduce the complexity of the surgery and to improve postoperative outcomes.
This retrospectively study reviewed the data of patients who underwent conventional TKA or new technique TKA at the Department of Orthopedics and Traumatology at the First Affiliated Hospital of Zhejiang Chinese Medical University from January 2011 to December 2014. Patients with Ranawat type-II VD caused by either osteoarthritis, rheumatoid arthritis, or hemophilic arthritis were included in this study. There was no age limit for enrolled patients. A basic understanding of the score sheet and consent for physical examination were also required. Ranawat type-II was defined as the femorotibial axis (FTA) > 10° on anteroposterior radiographs upon standing. Patients with combined joint immobilization, infection, old fracture, or a previous resection were excluded from the study. This study was approved by the hospital ethics and review committee of the First Affiliated Hospital of Zhejiang Chinese Medical University (2019-K-207-01). All patients provided informed consent for this study.
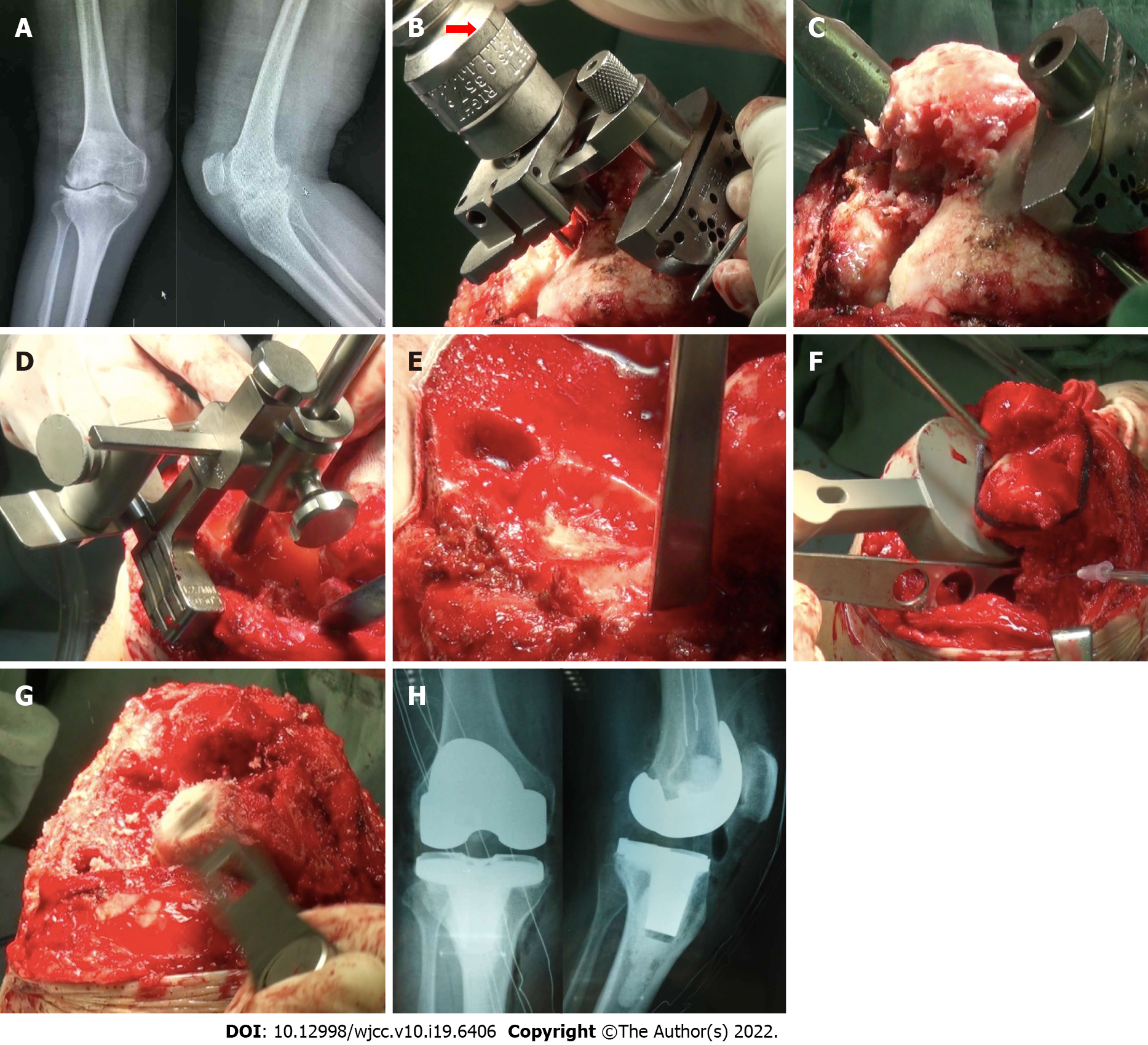
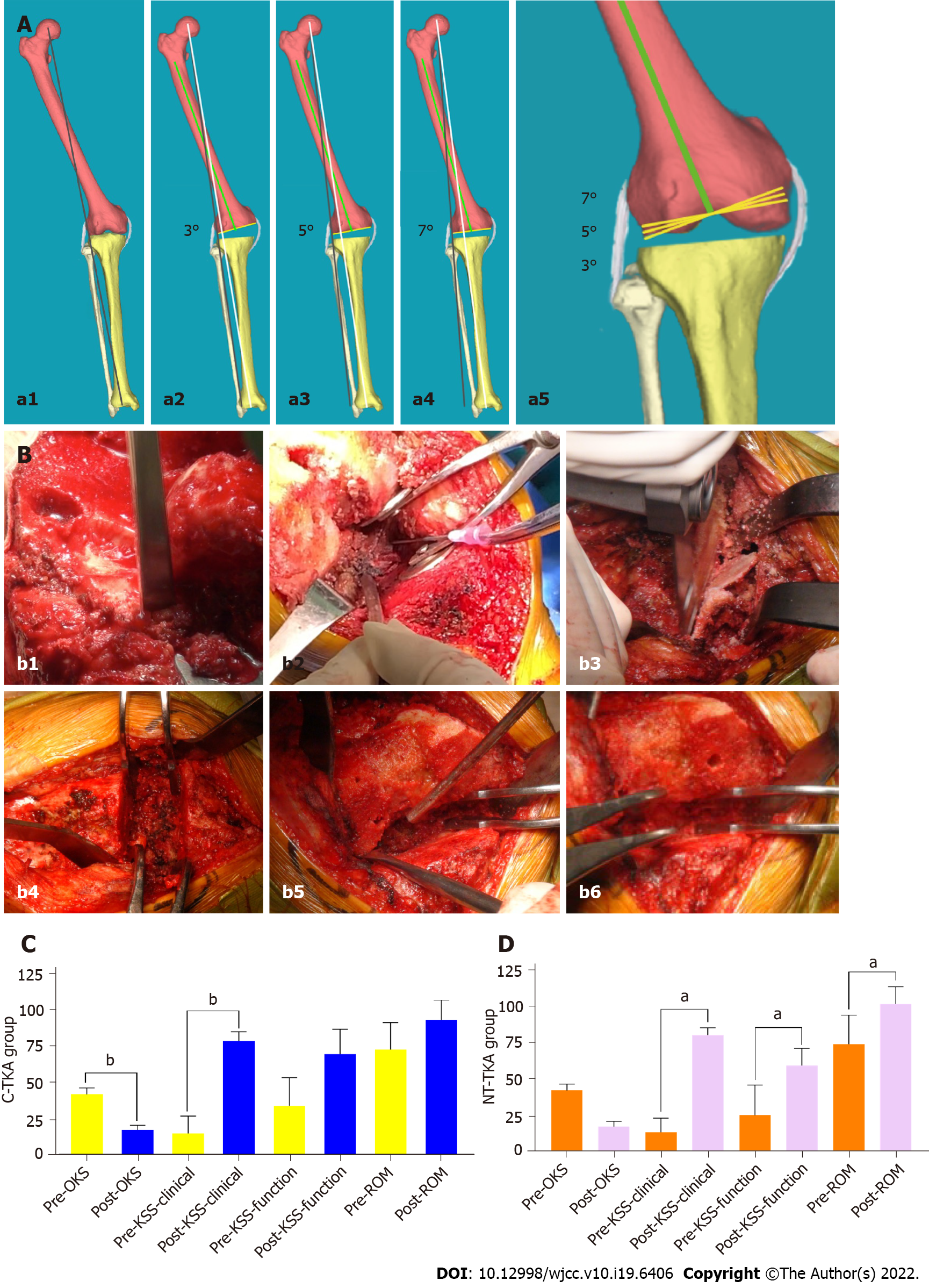
All patients were routinely given prophylactic antibiotics within 30 min before surgery. The supine position and tourniquet were used after a general anesthetic. The incision site was at the mid-level knee via a medial patella approach. For the distal femur resection in the new theory TKA group (NT-TKA), VCA was increased by 2° based on the traditional 3°, and the medial femoral condyle determined the resection thickness. A neutral resection was used routinely in the proximal tibia (Figure 1). Next, the surgeon extended the knee joint, evaluated the extension gap through a spacer block, and then performed joint space balance according to the straightening priority. Osteophytes that affect soft tissue balance were resected in a cuff-like manner, releasing soft tissue attachment point. Pie-crusting release was then performed on the lateral collateral ligament (LCL), the iliotibial band (ITB), and the posterolateral capsule (PLC) with a maximum of eight stitches through a 20 mL syringe needle. If the joint space was difficult to balance, the VCA was expanded to 7° with continuous release of soft tissues until the knee joint extension gap was in a rectangular shape (Figures 1 and 2A). External rotation resection and a "4 in 1" guide resection were performed at the 90° position of knee flexion. The external rotation resection angle of the anterior femoral condyle can be appropriately increased, usually 3°-6°, depending on the severity of the knee valgus. If the knee flexion was tense, the cuff-like release of the anterior soft tissue was performed (Figure 2B). For patients with an unsuccessful correction of the neutral FTMA, a 2° valgus FTMA was sacrificed to reduce the risk of ligament failure, joint instability, and consumption of constrained prostheses.
In the conventional TKA group (C-TKA), the distal femur cut bone angle was set to 3°, and the soft tissue was released according to the above steps until the joint space was balanced and the FTMA returned to 0°. Once the resection and the soft tissue balance were done, the posterior stabilized components were inserted. If the knee was unstable, legacy constrained condylar knee (LCCK) components were installed. If there was a femoral or tibial bone defect, remedial measures such as bone cement, small bone blocks, screws, and bone grafting were taken according to the degree of the defect. The patella was not resurfaced, but osteophyte cleaning and denervation were achieved. Finally, the surgeon stitched and bandaged the incision site. All knee prostheses were purchased from Zimmer (Zimmer, NexGen, LPS/LCCK, Warsaw, United States). All procedures were performed by the same orthopedic surgeon with more than 30 years of clinical experience.
Postoperatively, prophylactic low molecular weight heparin (0.4 mL/4100 IU, 1 vial a day) was initiated and maintained for 5 wk for prevention of deep venous thrombosis or VTE. Cefuroxime sodium (1.5 g, twice a day) was given and maintained for 1 wk to prevent infection. In addition, all patients received physiotherapy and rehabilitation training under the guidance of a professional rehabilitation specialist. At day 1 post-surgery, patients were allowed to walk with full weight-bearing under the protection of crutches until the patient was confident walking independently.
Hip-knee-ankle (HKA), range of motion (ROM), Oxford knee score (OKS), and knee society score (KSS) were used to evaluate the joint function of patients before and after surgery. Any adverse events were recorded during the postoperative follow-up period.
The sample sizing was calculated by KSS. The data of patients enrolled in this study were accessed via an electronic medical record system by two investigators who received standardized training. Main biodata included age, gender, body mass index, diagnosis, FTMA, and operation time.
All patients were discharged from the hospital 2 wk after surgery and were followed by telephone and outpatient clinic visits at 1, 3, and 6 mo for the first year, and then an annual telephone or outpatient follow-up for 3 years. Physical examination and routine radiographs (X-ray) of the surgical site were performed at each follow-up visit by the attending physician. For patients living in far-flung areas, the X-ray results from the local hospital were accepted.
Data were analyzed by another researcher who also received standardized training of SPSS for Mac (Version 21; IBM Corp, Armonk, NY, United States). Normally distributed and non-normally distributed continuous variables are presented as the mean ± SD and median (range), respectively. Categorical variables are presented as counts (percentages). Normally distributed and non-normally distributed continuous variables were analyzed by independent-sample t-test and Mann-Whitney U test. Categorical variables were analyzed by the chi-square test. Statistical significance was defined at P < 0.05.
A total of 109 patients (110 knees) with knee valgus who underwent primary TKA were included in this study from January 2011 to December 2014. Six patients dropped out from the study, including two patients who died of a cardiovascular event, three patients lost to follow-up, and 1 bedridden patient with cerebral hemorrhage. Finally, 103 patients (103 knees), including 69 females and 34 males with a mean age of 63 years (range, 38 to 79 years), were included in this study with a mean follow-up period of 79 mo (range, 60 to 104 mo). Of the patients included, 42 (42 knees; 15 males and 27 females) with an average follow-up of 83 mo (range, 63-104 mo) were assigned to the C-TKA group, and 61 (61 knees; 19 males and 42 females) with an average follow-up period of 76 mo (range, 60-97 mo) were assigned to the NT-TKA group. There were no statistically significant differences between the two groups with regard to age, gender, body mass index, diagnosis, FTA, and length of follow-up (Table 1).
| Characteristic | C-TKA group (n = 42 case) | NT-TKA group (n = 61 case) | P value |
| Knee number (n) | 42 | 61 | |
| Age (yr) | 62.9 (39-77) | 63.5 (38-79) | 0.083 |
| Gender, n (%) | 0.628 | ||
| Male | 15 (35.71) | 19 (31.15) | |
| Female | 27 (64.29) | 42 (68.85) | |
| BMI (kg/m2) | 24.0 ± 2.2 | 25.1 ± 2.8 | 0.091 |
| Diagnosis, n (%) | 0.770 | ||
| Primary osteoarthritis | 30 (71.43) | 44 (72.13) | |
| Rheumatoid arthritis | 11 (26.19) | 14 (22.58) | |
| Hemophilic arthritis | 1 (2.38) | 3 (4.92) | |
| FTA (°) | 26.8 ± 5.7 | 26.3 ± 5.2 | 0.784 |
| Operation time | 105.6 ± 17.7 | 99.2 ± 11.0 | 0.031 |
| Follow-up (mo) | 83.4 ± 10.1 | 75.6 ± 10.0 | 0.907 |
The KSS data in clinical stability at 1 mo post-operation for the C-TKA and NT-TKA groups were 11.2 ± 3.8 and 13.3 ± 2.9, respectively, with a significant difference (P < 0.01); however, there was no significant difference in joint stability at the last follow-up (Table 2). The HKA, ROM, OKS KSS, and prosthesis survival rate data had no significant differences in both the preoperative and follow-up periods. In the C-TKA and NT-TKA groups, the last follow-up patient data showed improved HKA, ROM, OKS, and KSS compared to preoperative data (Figure 2C and D).
| Parameter | C-TKA group (n = 42 case) | NT-TKA group (n = 61 case) | P value |
| HKA (°) | |||
| Pre- | 17.2 ± 5.9 | 16.0 ± 4.5 | 0.076 |
| Post- | 0.5 ± 1.0 | 0.8 ± 1.1 | 0.225 |
| P value | < 0.001 | <0.001 | - |
| ROM (°) | |||
| Pre- | 73.0 ± 18.7 | 75.0 ± 20.1 | 0.369 |
| Post- | 93.5 ± 13.6 | 102.9 ± 11.8 | 0.781 |
| P value | 0.074 | < 0.001 | - |
| OKS | |||
| Pre- | 42.0 ± 4.5 | 42.8 ± 4.5 | 0.654 |
| Post- | 17.4 ± 3.3 | 17.8 ± 3.6 | 0.854 |
| P value | 0.038 | 0.173 | - |
| KSS | |||
| Pre-clinical | 14.9 ± 12.1 | 13.9 ± 9.7 | 0.077 |
| Post-clinical | 78.9 ± 6.4 | 81.3 ± 5.0 | 0.655 |
| P value | 0.010 | < 0.001 | - |
| Pre-functional | 34.2 ± 19.4 | 25.7 ± 20.9 | 0.530 |
| Post-functional | 69.9 ± 17.1 | 60.0 ± 12.1 | 0.172 |
| P value | 0.117 | < 0.001 | - |
| KSS clinical stability | |||
| Preoperative | 9.3 ± 4.4 | 10.0 ± 4.0 | 0.378 |
| 1 mo (post) | 11.2 ± 3.8 | 13.3 ± 2.9 | 0.007 |
| Last follow-up | 14.3 ± 1.8 | 14.5 ± 1.5 | 0.132 |
| Complications | 3 | 0 | 0.034 |
| Instability | 2 | 0 | |
| Nerve injury | 1 | 0 | |
| Prosthesis | 0.002 | ||
| Posterior stabilized | 36 | 61 | |
| Constrained prosthesis | 6 | 0 | |
| Survival rate | 42/42 | 61/61 |
There were six patients with constrained prostheses, one with common peroneal nerve injury, and two with joint instability in the C-TKA group, but no patients developed such complications in the NT-TKA group. There were significant differences in the constrained prosthesis usage and complications between the groups (P < 0.01 and P < 0.05, respectively) (Table 2). At the last follow-up, the prostheses were all stable, and no patients underwent joint revision in either group.
This study proposed to apply the theory of synergistic balance between bone and soft tissue in TKA surgery, which reduced the need for soft tissue loosening, operation time, and constrained prosthesis while maintaining early stability of the joint.
TKA for VD requires the surgeon to be equipped with experience in dealing with different bone and soft-tissue conditions, positioning of the resection, soft-tissue release, and possible complications. For patients with severe VD, sacrificing 2° of neutral FTMA can abrogate excessive release of the lateral soft tissue and reduce the incidence of joint instability while maintaining joint function. To our knowledge, this is the first study to follow patients for more than 5 years in exchange for soft tissue stabilization at the expense of FTMA. In our opinion, TKA should be pursued with the common balance of bone and soft tissue since both are critical and closely related to preoperative joint function.
TKA for Ranawat type-II VD is challenging due to intra- and extra-articular bony abnormalities. Improper limb and component alignments occur due to distortion of the bony canal and variations in femoral anatomy. Therefore, a conventional system to guide alignment may be inappropriate[1,6]. The VCA can be determined in two ways during distal femur resection: Fixed VCA and individualized angle. Koskinen et al[7] suggested using a 3° VCA of the distal femur instead of a 5°-7° to achieve optimal correction of the underlying deformity for the knee valgus. However, Huang et al[6] found conventional 3° VCA in patients with Ranawat type-II VD knee might be unreasonable because of the coronal femoral bowing deformities. To restore the FTMA, distal femoral resection should be performed with an overcorrection of 2°[8]. Tucker et al[9] believed that a VCA of 5° valgus or more should be applied if the trapezoidal extension gap was unbalanced. However, fixed VCA might result in unexpected results. Some authors[10,11] advocated for an individualized angle, defined by the anatomical and mechanical axes of the femur. However, a hypoplastic lateral femoral condyle in the valgus knee might lead to the offsetting of the central knee joint line; hence, the actual anatomical axis of the femur is not achieved. In this study, the conventional 3° VCA was increased to 5°-7°, which corrected more osseous FTMA and increased the relative length of the lateral soft tissue. Moreover, 7° VCA is relatively safe in the knee valgus, like ordinary TKA, and does not damage the collateral ligament.
Balancing the soft tissue in Ranawat type-II valgus knee is another challenge and might contribute to complications such as peroneal nerve palsy and joint instability. Several surgical techniques have been developed to release the lateral supporting structures in TKA, including cruciform release, Z-plasty, and pie-crust technology. From our experience, the first step is to remove osteophytes, which affect soft tissue tension. We recommend to use the pie-crusting technique with a needle, not a blade, which can reduce the risk of joint instability.
Effective restoration of the FTMA mainly depends on the precise resection and soft tissue release in TKA. Poor prosthesis position will increase the failure rate of TKA[12]. A 8-12-year follow-up study of 115 TKA patients by Jeffrey et al[13] found that the rate of joint prosthesis loosening was about 3% with FTMA in a neutral position (within ± 3°) and 24% beyond this range (> 3°) (P < 0.05). Studies have shown that a neutral MA can protect the soft tissue, improve joint function, and prolong prosthesis survival when adapted as a gold standard. However, Stucinskas et al[5] conducted a 1-year follow-up of 91 TKA patients and found that patients with neutral FTMA had no significant results in ROM, KSS, and muscle strength compared with patients with non-neutral FTMA. Bellemans et al[14] also held the same view that restoration of neutral FTMA in all patients may not be befitting and would be unnecessary. Although the mean coronal alignment was almost constant, most patients did not achieve neutral FTMA[14]. Hirschmann et al[4] measured the HKA angle of 308 non-osteoarthritic knees of 160 patients and found that constitutional varus and valgus probabilities were 32.4% and 26.6%, respectively. Similarly, Bellemans et al[14] found an incidence of 48.2% and 4.8%, respectively. Lately, the concept of anatomic restoration or kinematically aligned (KA) has gained traction[15]. This theory does not necessarily restore neutral FTMA but rather the natural alignment of the knee. KA TKA reduces the need for soft tissue release and naturally restores the FTMA more to the pre-arthritic state of the knee. Laende et al[16] conducted a randomized controlled trial with a 2-year follow-up and found no significant differences in the prosthesis fixation and OKS scores between KA TKA and FTMA TKA. A meta-analysis by Hetaimish et al[17] showed that even if KA TKA did not deliberately pursue the neutral MA, there was no significant difference in the incidence of postoperative complications, hemoglobin level, or hospital stay compared with FTMA TKA. However, there was a benefit trend towards shorter operation time (P = 0.01) and better overall knee function (P < 0.01) in patients with FTMA TKA. Besides, more patients who undergo FTMA TKA might have an outlier varus and valgus alignment when compared to FTMA due to high intraoperative forces in the medial and lateral compartments of the knee[18]. Based on our theory, which was similar to KA, patients with poor preoperative lateral soft tissue status and VD > 20° would be sacrificed a 2° valgus.
The constrained prosthesis was considered a better option when the above strategy did not achieve joint stability. The constrained prosthesis can simplify operation procedures, avoid excessive soft tissue release, and shorten operation time but not without its associated prohibitive cost, more bone loss, and knee pain. Meanwhile, the rate of constrained prosthesis revision was twice as high at 10 years and three times higher at 20 years postoperatively[19]. Therefore, several studies recommend minimizing the use of constrained prostheses under the premise of stability[20]. The balance between bone and soft tissue should be considered during any TKA procedure. If joint space balance cannot be achieved by soft tissue release, the VCA should be increased appropriately. If the joint gap is still unbalanced, a 2° FTMA is sacrificed for the joint stability and unconstrained prosthesis (Table 2). Statistical results show that the probability of peroneal nerve injury is 0.3%-9.5%, which manifests as sagging feet, spanning gait, inability to supinate the foot, muscle atrophy, and loss of cutaneous sensation in the innervated area. In the current study, there were 1 of 42 patients with peroneal nerve injury caused by traction, which recovered fully following VD correction in the C-TKA group but no patient in the NT-TKA cohort developed this injury.
Limitations of this study include possible biases like patient performance bias and lack of independent review of radiographs. In addition, this was a single surgeon case series using the new concept of resection and soft tissue release. Also, our study is a short-term study, and the theory of bone and soft tissue co-balance requires longer follow-up to ascertain its impact on joint function and prosthetic survival. The application of finite element analysis can provide simulated solutions for such clinical conundrums. Future research should focus on the influence of resection on soft tissue release and the critical value of ligament release by finite element analysis, along with mechanical changes in the medial and lateral prosthesis planes post-VD correction.
Bone and soft tissue balance is equally important in a TKA procedure. Adopting 5°-7° VCA for VD and sacrificing 2° neutral FTMA for severe VD of the knee during TKA can reduce the need for soft tissue release, maintain joint stability, and abrogate the use of constrained prostheses while minimizing postoperative complications.
Total knee arthroplasty (TKA) for Ranawat Type II valgus deformity (VD) of the knee is challenging and technical due to resection and soft tissue balance.
Unreasonable osteotomy and soft tissue release in pursuit of neutral femorotibial mechanical axis (FTMA) will increase joint instability, limited prosthesis use, and complications.
This study aimed to provide a new technique of surgical resection, soft tissue release, and FTMA for the VD of the knee during TKA.
Sixty-one patients had a valgus cut angle (VCA) of 5°-7° in the new theory TKA group (NT-TKA). We chose to sacrifice the 2° FTMA to reduce the risk of survival failure, joint installation, and consumption of constrained procedures if the FTMA still cannot return to the neutral position after the maximum soft tissue release. Forty-two patients in the conventional TKA group (C-TKA) were treated with a VCA of 3°-5° and pursuit of neutral FTMA.
The constrained prosthesis usage and complications in NT-TKA were lower than those in C-TKA (P = 0.002 and P = 0.034, respectively). The KSS at 1 mo post-operation for NT-TKA was higher than that in C-TKA (P = 0.007).
Adopting 5°-7° VCA for VD and sacrificing 2° neutral FTMA for severe VD which cannot be completely corrected during TKA can reduce the need for soft tissue release, maintain early joint stability, reduce the use of constrained prostheses, and minimize postoperative complications.
This series of surgical technique for VD of the knee during TKA have certain clinical guiding significance.
We would like to thank Tong PJ and Lv SJ for their help in research ideas and design; He BJ and Lv SJ for their role in research implementation and manuscript writing; Huang JF for manuscript editing and writing; Wang XJ, Mao Q, Lv SJ, and He BJ for their immense support in data collection and manuscript submission.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abulsoud MI, Egypt S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Yan JP
| 1. | Ranawat AS, Ranawat CS, Elkus M, Rasquinha VJ, Rossi R, Babhulkar S. Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am. 2005;87 Suppl 1:271-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 97] [Article Influence: 4.9] [Reference Citation Analysis (1)] |
| 2. | Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop. 2014;38:273-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 3. | McAuley JP, Collier MB, Hamilton WG, Tabaraee E, Engh GA. Posterior cruciate-retaining total knee arthroplasty for valgus osteoarthritis. Clin Orthop Relat Res. 2008;466:2644-2649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Moser LB, Hess S, Amsler F, Behrend H, Hirschmann MT. Native non-osteoarthritic knees have a highly variable coronal alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27:1359-1367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Stucinskas J, Robertsson O, Sirka A, Lebedev A, Wingstrand H, Tarasevicius S. Moderate varus/valgus malalignment after total knee arthroplasty has little effect on knee function or muscle strength. Acta Orthop. 2015;86:728-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Huang TW, Chuang PY, Lee CY, Lin SJ, Huang KC, Shen SH, Tsai YH, Lee MS, Hsu RW. Total knee arthroplasty in patients with Ranawat type-II valgus arthritic knee with a marked coronal femoral bowing deformity: comparison between computer-assisted surgery and intra-articular resection. J Orthop Surg Res. 2016;11:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Koskinen E, Remes V, Paavolainen P, Harilainen A, Sandelin J, Tallroth K, Kettunen J, Ylinen P. Results of total knee replacement with a cruciate-retaining model for severe valgus deformity--a study of 48 patients followed for an average of 9 years. Knee. 2011;18:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Lombardi AV Jr, Dodds KL, Berend KR, Mallory TH, Adams JB. An algorithmic approach to total knee arthroplasty in the valgus knee. J Bone Joint Surg Am. 2004;86-A Suppl 2:62-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Tucker A, O'Brien S, Doran E, Gallagher N, Beverland DE. Total Knee Arthroplasty in Severe Valgus Deformity Using a Modified Technique-A 10-Year Follow-Up Study. J Arthroplasty. 2019;34:40-46.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Shi X, Li H, Zhou Z, Shen B, Yang J, Pei F. Comparison of Postoperative Alignment Using Fixed vs Individual Valgus Correction Angle in Primary Total Knee Arthroplasty With Lateral Bowing Femur. J Arthroplasty. 2016;31:976-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Rahm S, Camenzind RS, Hingsammer A, Lenz C, Bauer DE, Farshad M, Fucentese SF. Postoperative alignment of TKA in patients with severe preoperative varus or valgus deformity: is there a difference between surgical techniques? BMC Musculoskelet Disord. 2017;18:272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Kim YH, Park JW, Kim JS, Park SD. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38:379-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 272] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 13. | Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 767] [Cited by in RCA: 698] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 14. | Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? Clin Orthop Relat Res. 2012;470:45-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 729] [Article Influence: 56.1] [Reference Citation Analysis (0)] |
| 15. | Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS. Alignment in total knee arthroplasty. Bone Joint J. 2020;102-B:276-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 167] [Article Influence: 33.4] [Reference Citation Analysis (0)] |
| 16. | Laende EK, Richardson CG, Dunbar MJ. A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Bone Joint J. 2019;101-B:929-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 80] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 17. | Hetaimish BM, Khan MM, Simunovic N, Al-Harbi HH, Bhandari M, Zalzal PK. Meta-analysis of navigation vs conventional total knee arthroplasty. J Arthroplasty. 2012;27:1177-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 244] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 18. | Shelton TJ, Nedopil AJ, Howell SM, Hull ML. Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Bone Joint J. 2017;99-B:1319-1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 19. | Martin JR, Beahrs TR, Stuhlman CR, Trousdale RT. Complex Primary Total Knee Arthroplasty: Long-Term Outcomes. J Bone Joint Surg Am. 2016;98:1459-1470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Madonna V, Screpis D, Condello V, Piovan G, Russo A, Guerriero M, Zorzi C. A novel technique for combined medial collateral ligament and posterior oblique ligament reconstruction: technical note. Knee Surg Sports Traumatol Arthrosc. 2015;23:2814-2819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |