Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6370
Peer-review started: October 29, 2021
First decision: December 12, 2021
Revised: December 13, 2021
Accepted: May 8, 2022
Article in press: May 8, 2022
Published online: July 6, 2022
Processing time: 238 Days and 0.9 Hours
The coronavirus disease 2019 (COVID-19) pandemic impacted in a still undefined way pregnant women’s mental health. There are reports of mood and affect changes in the general population and the suggestion that similar changes occur also in the pregnant population. The greater vulnerability of women during the COVID-19 restriction period may translate into a greater risk for mental disorders in the gestational period. We hypothesised that pregnant women in the pre-pandemic period would have less psychopathology and more psychological support than pregnant women during the pandemic restriction period.
To compare pregnant women for anxiety, prenatal depression, psychopathology, and social support before and after the awareness of the pandemic.
We administered to women willing to participate in their 2nd-3rd trimesters of pregnancy the Edinburgh Postnatal Depression Scale (EPDS), the State-Trait Anxiety Inventory Form Y (STAI-Y), and the Symptom CheckList-90-Revised (SCL-90R); we further collected sociodemographic variables and explored women’s social support. The comparison was cross-sectional. The first sample was termed nonCOVID-19 because data were gathered before the COVID-19 outbreak (January 2020-February 2020) was declared, and the second sample termed COVID-19 because participants were already subjected to the COVID-19–related restrictive measures (January 2021-February 2021). Since normal distribution was not met (Shapiro-Wilk test applied), we applied nonparametric Mann-Whitney’s U-test to compare psychometric tests. Ethical standards were met.
The nonCOVID-19 group reported higher support from partners only, while the COVID-19 group reported multiple support (χ2 = 9.7181; P = 0.021); the nonCOVID-19 group scored higher than the COVID-19 group only on state anxiety among psychometric scales [STAI-Y1, nonCOVID-19 median = 39 (95%CI: 39.19-51.10) vs COVID-19 median= 32 (95%CI: 30.83-38.90); Mann-Whitney’s U=117.5, P = 0.00596]. Other measures did not differ meaningfully between the two groups. Scores on the EPDS, the state and trait subscales of the STAI-Y, and most SCL-90R subscales inter-correlated with one another. The anxiety component of the EPDS, EPDS-3A, correlated poorly with other measures, while it was the Global Symptom Index of the SCL-90-R that correlated most strongly with most measures. Our results are at odds with most literature and do not confirm increased depression and anxiety rates in pregnant women during the pandemic.
The ability of pregnant women to deal with novel generalised threats involves mobilization of inner resources. Increasing sources of social support may have produced anxiolysis in the COVID-19 sample.
Core Tip: The impact of the coronavirus disease 2019 (COVID-19) pandemic on women’s mental health is currently undefined. We assessed anxiety, prenatal depression, and psychopathology in pregnant women by comparing a sample with data collected prior to COVID-19 with one post-COVID-19. The pre-COVID-19 sample scored higher on state anxiety than the post-COVID-19 group; the former reported more partner support, while the latter reported more multiple support. Results show that pregnant women did respond to COVID-19 threat and restriction with increased psychopathology, indicating the recruitment of inner resources, but modified their social support pattern.
- Citation: Chieffo D, Avallone C, Serio A, Kotzalidis GD, Balocchi M, De Luca I, Hirsch D, Gonsalez del Castillo A, Lanzotti P, Marano G, Rinaldi L, Lanzone A, Mercuri E, Mazza M, Sani G. Pregnancy-related psychopathology: A comparison between pre-COVID-19 and COVID-19–related social restriction periods. World J Clin Cases 2022; 10(19): 6370-6384
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6370.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6370
The coronavirus disease 2019 (COVID-19) pandemic has impacted mental health of the general population. In Italy, the impact was found to be quite high[1], while in the extended Middle-East–North African region, it was reported to be mild[2], and in Taiwan, it was lower than that in other countries[3]. This heterogeneous distribution grossly matches the impact of the virus on within-country COVID-19 morbidity and mortality[1-3]. The individual psychopathological issues were also differently affected; fear decreased from the first to the second wave in China, while depression increased[4]. Clinically meaningful mental distress levels rose from about 20% in the pre-COVID-19 period to about 30% one month into UK pandemic-related restrictions[5]. In a large multination-multilingual survey, 40% of respondents reported fair mental health, 50% had only moderate mental health, and 10% reported poor mental health[6]. In this study, as well as in other studies conducted in France[7], Spain[8], Jordan[9], and Israel[10], it emerged that poor social conditions were a risk factor of developing poor mental health. Women were found to be more vulnerable to poor mental health[5,7-8,10,11]. The increase in psychological distress during the lockdown was found to have a greater impact on women[5,12]. Loneliness was attributed a role in engendering depressive symptoms in a US sample during the pandemic[11]. The relationship between loneliness and depression has long been known[13], while a link to anxiety became the focus of investigation much later[14]. During the pandemic, the proportion of lonely people in the general population increased due to the restrictive measures, so it is estimated that more people than before were exposed to depression and anxiety. In fact, during the COVID-19 pandemic period, a complex pattern of interrelationships among these constructs emerged, with loneliness and depression predicting each other across time, and loneliness predicting anxiety with the mediation of depression across time, independently from gender[15]. Loneliness, depression, and anxiety interact with negative thinking to boost each other in perinatal women and the chain may be interrupted or eased through social support[16]. However, most women during the pandemic have concerns about their own health and that of their foetus, and more than loneliness may impact their psychopathology.
This greater vulnerability of women during COVID-19 restrictions may translate into a greater risk for mental disorders in the gestational period[17]. Pregnant and postpartum women fear COVID-19 exposure or infection for themselves and/or foetus/baby; limited social support, and physical isolation and distancing may impact their mental health[18]. Perinatal women were at greater risk for psychopathology during the COVID-19 period in an analysis of the literature[17]. COVID-19–related social adversity affected negatively maternal mental health[19]. Pregnant women showed stronger increases in depression, anxiety, and negative affect than their non-pregnant counterparts, as well as reduced positive affect[20]. During the COVID-19 period, about 60% of pregnant women scored positive on depression questionnaires, about 30.0% scored positive on anxiety questionnaires, about 20% reported high levels of stress, and about 20% reported clinically significant insomnia[21]. Thus, the perinatal period during COVID-19 times may be an at-risk period for mental health according to current data. However, despite the bleak outlook for mental health during the COVID-19 period, there is hope that adequately addressing coping and resilience issues, mental health would not be adversely affected. In fact, dysfunctional coping has been linked to poor mental outcome, while emotion-focused coping has been associated with better mental outcomes[21]. Furthermore, in a general population sample, psychiatric symptoms increased acutely, but returned to baseline levels during sustained COVID-19 measures, pointing to the recruitment of internal resources related to resilience that may dampen the effect of the pandemic on mental health[22].
Since the influence of the pandemic in pregnancy and post-delivery has not been definitively established, having tested for psychopathology (depression, anxiety, and general psychopathology) a sample of pregnant women in their 2nd-3rd trimesters of pregnancy during the pre-COVID-19 period (i.e., a period when the virus had not yet spread over the country, or at least, people in the country did not figure out that it could represent a threat), we administered the same tests in women of comparable gestational ages after the COVID-19 outbreak and its consequent restrictions (when people in the country were aware of the threat the virus represented to their lives). We aimed at seeking possible differences in psychopathology between the two samples. We mainly focused on depression and anxiety symptoms, but did not disregard general psychopathology. We also collected socio-demographic data to identify possible predictors of clinically significant symptoms in our sample of pregnant women.
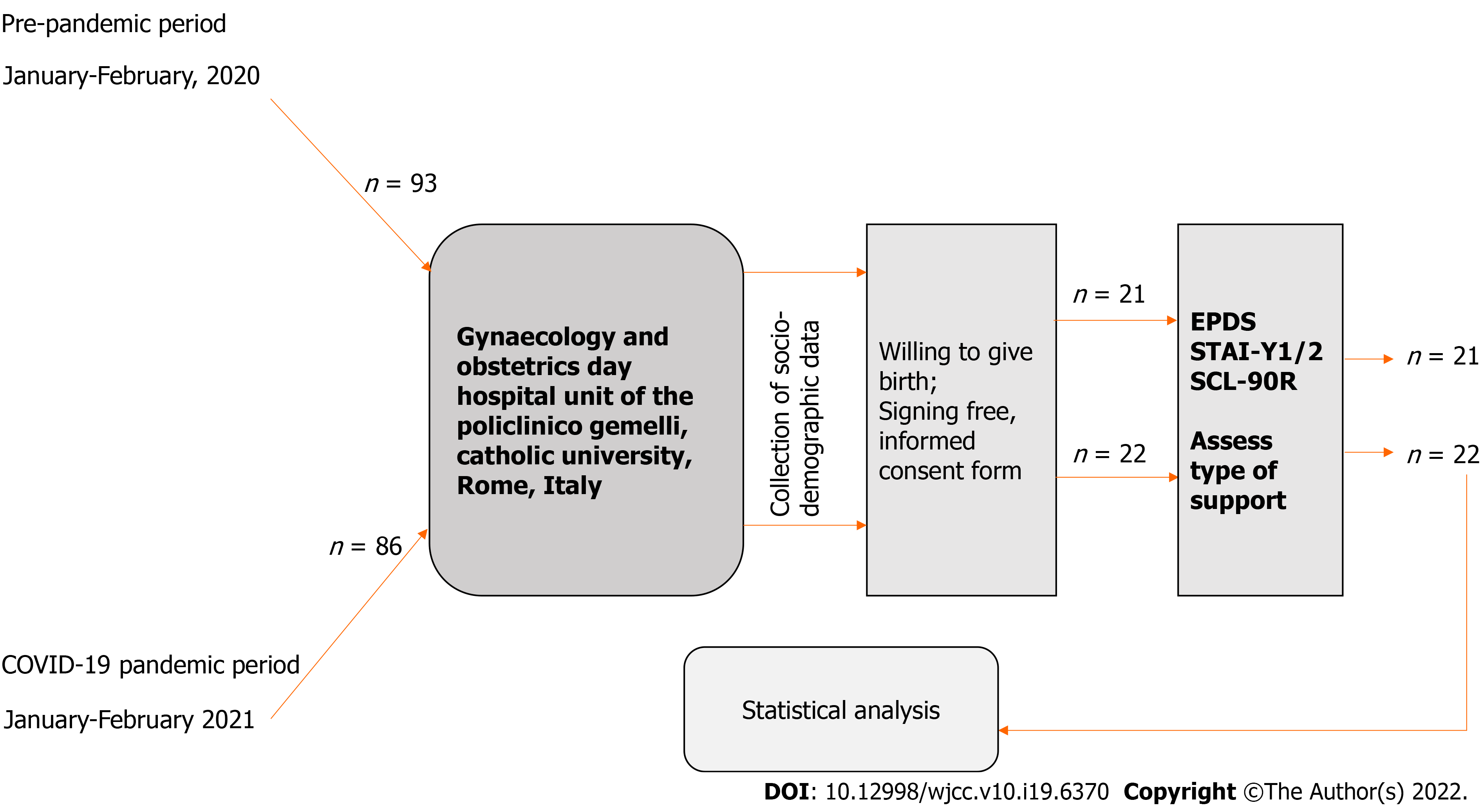
Consecutive pregnant women who visited the Gynaecology and Obstetrics Day Hospital Unit during the period January 2021-February 2021, amidst the COVID-19 pandemic, underwent screening for depression, anxiety, and psychiatric symptoms. The visit included basic assessment, the completion of a sociodemographic data collection form, and the administration of specific questionnaires. This group was defined as a COVID-19 group, despite that the women screened negative for the virus. This sample was compared with a sample of pregnant women whose data had been collected during the same year period of the previous year (nonCOVID-19 group), when they knew nothing about the impending pandemic. Eligible were women willing to give birth and to participate in the study. Among the 93 women visiting the service during the pre-pandemic period, only 21 provided free, informed consent for filling-in the proposed questionnaires, while during the corresponding COVID-19 pandemic period, 22 of 86 women provided content (Figure 1). Sociodemographic variables were not different between the women who accepted and those who did not. The reasons of refusal were most often lack of time and length of the Symptom CheckList-90-Revised (SCL-90R) questionnaire (Table 1).
| Parameter | Pre-COVID-19 | COVID-19 period | Statistic | P value | ||
| Age, yr (mean ± SD) | 35.714 ± 5.763 | 34.591 ± 8.342 | t = -0.511 | 0.612 | ||
| Gestational age, wk | 19.476 ± 4.792 | 17.636 ± 6.616 | t = 1.040 | 0.304 | ||
| Country of origin | ||||||
| Italy | 17 | 18 | χ2 = 0.1018 | 0.750 | ||
| Romania | 1 | 0 | ||||
| Ukraine | 1 | 1 | ||||
| Belgium | 1 | 0 | ||||
| Brazil | 1 | 1 | ||||
| Ecuador | 0 | 1 | ||||
| Gabon | 0 | 1 | ||||
| Educational level | ||||||
| Primary school | 0 | 0 | χ2 = 0.0879 | 0.957 | ||
| Middle school | 4 | 5 | ||||
| High school | 9 | 9 | ||||
| College/University/Postgraduate | 8 | 8 | ||||
| Partners | ||||||
| Yes | 20 | 20 | χ2 = 0.0017 | 0.967 | ||
| No | 1 | 2 | ||||
| Past pregnancies | ||||||
| No | 9 | 9 | χ2 = 0.0323 | 0.857 | ||
| Yes | 12 | 13 | ||||
| Past abortions | ||||||
| No | 14 | 13 | χ2 = 0.0393 | 0.843 | ||
| Yes | 7 | 9 | ||||
| Past abortion types | ||||||
| None | 14 | 13 | χ2 = 0.414 | 0.813 | ||
| Spontaneous | 4 | 6 | ||||
| Induced | 1 | 0 | ||||
| Both | 2 | 3 | ||||
| Medical conditions | ||||||
| Yes | 4 | 7 | χ2 = 0.3718 | 0.542 | ||
| No | 17 | 15 | ||||
| Psychiatric disorders (lifetime) | ||||||
| Yes | 10 (5 major depressive, 3 anxiety, 1 bipolar, 1 schizotypal personality) | 6 (3 major depressive, 3 anxiety) | χ2 = 1.1324 | 0.287 | ||
| No | 11 | 16 | ||||
| Psychotherapy | ||||||
| Yes | 6 | 1 | χ2 = 2.9585 | 0.085 | ||
| No | 15 | 21 | ||||
| Psychopharmacological treatment | ||||||
| Yes | 3 | 1 | χ2 = 0.3295 | 0.566 | ||
| No | 18 | 21 | ||||
| Family psychiatric history | ||||||
| Yes | 6 | 8 | χ2 = 0.0482 | 0.826 | ||
| No | 15 | 14 | ||||
| Current psychiatric disorder | ||||||
| Yes | 6 | 8 | χ2 = 0.0482 | 0.826 | ||
| No | 15 | 14 | ||||
| Stressful life events | ||||||
| Yes | 7 | 13 | χ2 = 1.9234 | 0.165 | ||
| No | 14 | 9 | ||||
| Significant pregnancy complications | ||||||
| Yes | 4 (3 emesis gravidarum, 1 pre-eclampsia) | 3 (emesis gravidarum) | χ2 = 0.2308 | 0.631 | ||
| No | 17 | 19 | ||||
| Support | ||||||
| Yes | 20 | 21 | χ2 = 0.477 | 0.490 | ||
| No | 1 | 1 | ||||
| Type of support | ||||||
| None | 1 | 1 | χ2 = 9.7181 | 0.021121 | ||
| Partner | 13 | 4 | ||||
| Relatives and friends | 4 | 6 | ||||
| Multiple | 3 | 11 | ||||
During the period of data collection of the COVID-19 sample, the infection had spread throughout Italy; however, in the north of Italy, the infection was widespread, very lethal, and out of control, whereas in Rome, which is situated in central Italy, the spread was threatening, but under control.
We compared data of the COVID-19 and the nonCOVID-19 samples, both regarding scores on psychometric instruments and sociodemographic, family, and personal clinical variables. The aim was to establish differences between the pre-pandemic and the pandemic periods in psychological distress and psychopathology of childbearing women.
Edinburgh Postnatal Depression Scale (EPDS)[23]: This is a 10-item self-rated questionnaire screening the risk of depression during the peripartum over the past week. Initially developed for the identification of postpartum depression[23], the EPDS was later validated for prenatal screen as well[24-25]. The questionnaire refers to how the woman felt in the last 7 d and each item is scored on a Likert-scale from 0 to 3, with each point receiving variable labels. Items 1 and 2 assess anhedonia, 3 guilt, 4 anxiety, 5 fear or panic, 6 helplessness, 7 sleep disorders, 8 sadness, 9 tendency to cry, and 10 tendency towards self-harm. Items 1, 2, and 4 are scored according to an increasing severity gradient, while all others are scored reversely. Higher scores indicate a higher risk of depression. In the original English version, a cutoff between 12 and 13 showed an 86% sensitivity and 78% specificity; however, the authors suggested a threshold between 9 and 10 for community screening[23]. These cutoffs were adopted by both original developers and other investigators[26,27]. The Italian validation studies identified 9-10[28] and 12-13[29] as optimal cutoffs. In this study, we adopted the following cutoffs: Total EPDS score ≥ 13 for “risk for major depression”, and 9-12 for “risk for mild depression”. Three items of the EPDS (EPDS 3-A, items 3, 4, and 5) were found to cluster together on an anxiety factor in postpartum women, with optimum cutoff scores ranging from 4-6 in different studies[30-34]. A higher cutoff was found to be best for postnatal anxiety (≥ 6)[31], with a lower cutoff of ≥ 4 best fitting the antenatal period[33]. We endorsed the latter as a proxy for anxiety, as our sample was exclusively composed of prenatal women. However, the authors maintain that the scale does not confirm an anxiety disorder and does not distinguish whether anxiety scores on these three items are a feature of depression or a distinct entity. In the original study, the authors recommended to watch immediately the score on item 10 (self-harm) and refer the patient for further evaluation in case score is ≠ 0, a recommendation that we adhered to strictly. The questionnaire has shown good psychometric properties, with a positive predictive value (PPV) ranging from 22%-82% and negative predictive value ranging from 70%-100%[35].
State-Trait Anxiety Inventory Form Y (STAI-Y)[36]: Charles Spielberger developed his concept of state and trait anxiety after Cattell and Schneier[37] (1958), to measure two different, albeit keen constructs, one responsive to environmental change (state) and the other relatively invariant (trait) in the mid-sixties[38] and published the X-form version a few years later[39]. Thirteen years later, they developed and validated their definitive Y-form, which differed in some respects from the X-form, with simpler forms of sentences and reversely directed items[40]. The inventory consists of two self-rated sheets with 20 statements each. Every item is scored 1 to 4 according to Likert scales, with the state Y1 referring to “how you feel right now”, with responses being 1 = Not at all, 2 = Somewhat, 3 = Moderately so, and 4 = Very much so, and the trait Y2 referring to “how you generally feel”, with responses being 1 = Almost never, 2 = Sometimes, 3 = Often, and 4 = Almost always. Higher scores indicate higher anxiety levels. Items 3, 4, 6, 7, 9, 12, 13, 14, 17, and 18 of the state form Y1 and 22, 24, 25, 28, 29, 31, 32, 35, 37, 38, and 40 of the trait form Y2 count as they are scored, while all others are scored inversely (1 counts 4, 2 counts 3, 3 counts 2, and 4 counts 1). The best fit is for a four-factor model, consisting of state anxiety present, state anxiety absent, trait anxiety present, and trait anxiety absent, each corresponding to the directly scored and to reverse items of each subscale[41]. This model provided a higher than 0.70 alpha composite reliability, convergent validity, and discriminant validity. Correlations between state anxiety present and trait anxiety present, and between state anxiety absent and trait anxiety absent were high (r = 0.770 and r = 0.923, respectively)[41].
Although there is still debate for the cutoffs of the STAI-Y[42], gender was found not to affect scores[43]. The developers of the scale provided the following cutoffs, which we followed in classifying our patients, i.e., 20-39 indicates low anxiety, 40-59 moderate, and 60-80 high anxiety, independently from the version used (state or trait)[36]. The STAI-Y2 showed an area under the curve of 84.7% for a cutoff of ≥ 52, with a 81.3% sensitivity and 77.5% specificity, a PPV of 41.9%, and a negative predictive value of 95.4% in a recent study[44], but the resulting cutoff has not been generally adopted.
Symptom CheckList-90-Revised[45]: This is a self-rated 90-item questionnaire exploring nine psychological domains. It evolved from a previous 58-item self-rated questionnaire, which was developed at Johns Hopkins in Baltimore, Maryland, with the intention to rate symptom severity along five dimensions, i.e., obsessive-compulsive behaviour, anxiety, depression, somatization, and interpersonal sensitivity; scores were then combined to produce a total distress score[46]. The revised version deleted some items from the first version and added 45 new items referring to four new dimensions, i.e., hostility, phobic anxiety, paranoid ideation, and psychoticism. The instrument contains items coding for eating and sleep problems. In particular, three items, i.e., 44 (Trouble falling asleep), 64 (Awakening in the early morning), and 66 (Sleep that is restless or disturbed), clustered to form the SLEEP dimension[47], which we used in this study. The distress related to each item during the last week is scored on a five-point (0-4) Likert scale, where 0 is not at all, 1 is a little bit, 2 is moderately, 3 is quite a bit, and 4 is extremely. The instrument provides three general indexes, i.e., the Global Severity Index (GSI), obtained by adding all scores and dividing by 90, the Positive Symptom Total (PST), i.e., the total number of symptoms on which the respondent scored > 0, and the Positive Symptom Distress Index, obtained by adding all scores on the 90 items and dividing by the PST. Despite good internal coherence for all subscales (α values 0.70-0.96), the SCL-90-R shows factor-structure instability, suggesting that the most reliable index to adopt is the GSI[48]. The tool was showed to be able to discriminate between community dwellers and psychiatric patients, with an area under the curve (AUC) of 83 %, Glass’s Δ of 1.4, Cohen’s d of 1.1, and diagnostic odds ratio of 12.5[49]. GSI ≥ 0.57 has been suggested as a cutoff for a German sample[50] to distinguish normal from psychiatric cases, but in a Chilean inmate population, this figure rose to 1.42[51].
All participants provided written informed consent, in accordance with all applicable regulatory and Good Clinical Practice guidelines and in full respect of the Ethical Principles for Medical Research Involving Human Subjects, as adopted by the 18th World Medical Association General Assembly (WMA GA), Helsinki, Finland (June 1964), and subsequently amended by the 64th WMA GA, Fortaleza, Brazil (October 2013). The study received approval from the local ethics committee (Ethics Committee of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Università Cattolica del Sacro Cuore of Rome, Rome, Italy).
We express sociodemographic parameters as the mean ± SD and used the t-test to compare the two groups when the variables were continuous, and as number (n) and percentages when the variables were nominal and used the χ2-test to compare the two groups. We used Pearson’s r coefficient to assess correlations. We preliminarily tested normality of distribution using the Shapiro-Wilk test[52]. The test produced values of W = 0.9219, P = 0.0062 for the EPDS, W = 0.8810, P = 0.0003 for the STAI-Y, and W = 0.7752, P < 0.000001 for the SCL-90, all of which were not compatible with a normal distribution. Hence, we turned to the non-parametric Mann-Whitney U-test and express psychometric data as medians and 95% confidence interval [CI]. We applied the Bonferroni correction[53] to address multiple testing. This brought the cutoff for statistical significance originally set at P < 0.05 (valid for sociodemographic comparisons) down to P < 0.0125 for the psychometric comparisons (for intra-SCL-90 comparisons this was P < 0.0045), while for correlations, we applied no correction as it could be too conservative and exposed to type-II error[54]. A biostatistician processed all data using the SPSS version 26.0 (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corporation, 2019).
The pre-COVID-19 (n = 21) and COVID-19 (n = 22) groups did not differ for age [mean age (years) = 35.714 ± 5.763 vs 34.591 ± 8.342; t = -0.511; P = 0.612, not significant (NS)] or gestational age [mean (week) = 19.476 ± 4.792 vs 17.636 ± 6.616; t = 1.040; P = 0.304, NS]. Table 1 shows the sociodemographic characteristics of the two samples. The only measure in which the nonCOVID-19 and COVID-19 groups differed was the type of support, with the nonCOVID-19 group reporting higher support from partners only, whereas the COVID-19 group reported multiple support, which comprised partners, parents and relatives, and friends (χ2 = 9.7181; P = 0.021) (Table 1). However, total support was almost identical between the two groups.
Table 2 shows the comparison between the pre-COVID-19 and post-COVID-19 outbreak hospitalized samples on their scores on psychometric questionnaires. The two samples did not differ in their EPDS scores, total or EPDS-3A; all women scored 0 on the suicidal ideation item. The pre-COVID-19 sample scored higher on the state anxiety questionnaire only.
| Measure [median (95%CI) for all measures] | Pre-COVID-19 | COVID-19 period | Mann-Whitney’s U | P value |
| EPDS total score | 6 (4.92 to 9.94) | 7.5 (5.64 to 9.64) | 213 | 0.6672 |
| EPDS-3A (anxiety cluster, items 3, 4, and 5) | 2 (1.52 to 3.24) | 3 (2.64 to 4.36) | 150.5 | 0.05238 |
| EPDS-suicide item 10 | 0 (0 to 0) | 0 (0 to 0) | 231 | 0.99202 |
| STAI-Y1 state | 39 (39.19 to 51.10) | 32 (30.83 to 38.90) | 117.5 | 0.00596a |
| STAI-Y2 trait | 33 (31.70 to 39.45) | 31 (29.49 to 36.42) | 193.5 | 0.36812 |
| SCL-SOM (somatization) | 0.583 (0.47 to 1.00) | 0.25 (0.27 to 0.66) | 793.5 | 0.54186 |
| SCL-O-C (obsessive-compulsive) | 0.4 (0.39 to 0.92) | 0.1 (0.15 to 0.52) | 631 | 0.20408 |
| SCL-I-S (interpersonal sensitivity) | 0.222 (0.148 to 0.66) | 0.0555 (0.08 to 0.44) | 533 | 0.4654 |
| SCL-DEP (depression) | 0.462 (0.45 to 1.12) | 0.1155 (0.17 to 0.54) | 674.5 | 0.17068 |
| SCL-ANX (anxiety) | 0.6 (0.50 to 1.26) | 0.1 (0.13 to 0.42) | 526.5 | 0.09692 |
| SCL-HOS (hostility) | 0.167 (0.22 to 0.64) | 0.167 (0.06 to 0.19) | 512 | 0.18024 |
| SCL-PHOB (phobic anxiety) | 0 (0.05 to 0.43) | 0 (0.02 to 0.25) | 394 | 0.86502 |
| SCL-PAR (paranoid ideation) | 0.167 (0.15 to 0.74) | 0 (0.12 to 0.43) | 438 | 0.70394 |
| SCL-PSY (psychoticism) | 0 (0.06 to 0.48) | 0 (0.05 to 0.18) | 432 | 0.63836 |
| SCL-SLEEP (sleep disorder) | 0.333 (0.33 to 1.26) | 0.333 (0.30 to 0.9148) | 474.5 | 0.96012 |
| SCL-GSI (Global Symptom Index) | 0.311 (0.34 to 0.81) | 0.1665 (0.16 to 0.42) | 838 | 0.56868 |
There were 4 out of 21 (19.05%) cases in the pre-COVID-19 group who scored positive for risk for major depression on the EPDS total (≥ 13), with 3 cases between 9 and 12, i.e., risk for mild depression (14.28%), while 14 cases (66.67%) scored lower than all cutoffs (no depression); 5 (23.81%) scored positive on the EPDS-3A (≥ 4), and none (0%) on the EPDS suicide item 10. In the COVID-19 sample, there were 2 out of 22 (9.09%) cases scoring positive for risk for major depression (EPDS total ≥ 13), 7 (31.82%) scored 9-12 (risk for mild depression), and 13 (59.09%) scored lower than 9 (no depression), while 10 (45.45%) scored positive on the three-item anxiety component of the EPDS (-3A) and none (0%) scored ≠ 0 on the suicide item 10. The two groups did not differ significantly.
According to the cutoffs provided by Spielberger et al[36], we classified 11 (52.38%) patients from the pre-COVID-19 sample and 18 (81.82%) from the COVID-19 sample as low anxiety on the STAI-Y1, and 6 (28.57%) from the pre-COVID-19 and 4 (18.18%) from the COVID-19 sample as moderate, while 4 (19.05%) patients from the pre-COVID-19 group and none (0%) from the COVID-19 group scored in the high anxiety range. The two groups differed meaningfully, with the pre-COVID-19 group scoring more in the severe range than the COVID-19 sample (χ2 = 8.116; P = 0.03933, two-sided). Regarding the STAI-Y2 form, 14 (66.67%) patients from the pre-COVID-19 group and 16 (72.73%) from the COVID-19 group scored in the low anxiety range, 7 (33.33%) from the pre-COVID-19 and 6 (27.27%) from the COVID-19 samples scored in the moderate anxiety range, and no patient from either group scored in the high anxiety range (0% for both samples). The two groups did not differ meaningfully (χ2 = 0.187; P = 0.74699, two-sided). Correlations are shown in Table 3. It is worthy of note that the EPDS-3A correlated poorly with other measures, while the GSI of the SCL-90-R correlated most strongly with most measures.
| EPDS total | EPDS-3A | STAI-Y1 | STAI-Y2 | SCL-SOM | SCL-OC | SCL-INT | SCL-DEP | SCL-ANX | SCL-HOS | SCL-PHOB | SCL-PAR | SCL-PSY | SCL-SLEEP | SCL-GSI | |
| EPDS total | - | 0.703c | 0.61c | 0.53c | 0.4602b | 0.4673b | 0.3278a | 0.44b | 0.4233b | 0.3454a | 0.1706 | 0.4185b | 0.1675 | 0.6013c | 0.458b |
| EPDS-3A | 0.703c | - | 0.1561 | 0.1108 | 0.2996 | 0.225 | 0.2065 | 0.2553 | 0.2744 | 0.2194 | 0.2133 | 0.2297 | 0.1519 | 0.3224a | 0.2858 |
| STAI-Y1 | 0.61c | 0.1561 | - | 0.7365c | 0.4101b | 0.5533b | 0.4736b | 0.6443c | 0.6568c | 0.4417b | 0.2841 | 0.4448b | 0.2532 | 0.4705b | 0.574c |
| STAI-Y2 | 0.53c | 0.1108 | 0.7365c | - | 0.4623b | 0.585c | 0.5083c | 0.5457c | 0.5145c | 0.4041b | 0.3112a | 0.5736c | 0.3359a | 0.5024c | 0.5644c |
| SCL-SOM | 0.4602b | 0.2996 | 0.4101b | 0.4623b | - | 0.7321c | 0.6493c | 0.723c | 0.5977c | 0.7221c | 0.6816c | 0.6684c | 0.652c | 0.6091c | 0.8345c |
| SCL-OC | 0.4673b | 0.225 | 0.5533b | 0.585c | 0.7321c | - | 0.7634c | 0.8937c | 0.7555c | 0.7149c | 0.5539c | 0.8873c | 0.6972c | 0.5762c | 0.9174c |
| SCL-INT | 0.3278a | 0.2065 | 0.4736b | 0.5083c | 0.6493c | 0.7634c | - | 0.7977c | 0.6119c | 0.6796c | 0.6925c | 0.8046c | 0.7961c | 0.396b | 0.8512c |
| SCL-DEP | 0.44b | 0.2553 | 0.6443c | 0.5457c | 0.723c | 0.8937c | 0.7977c | - | 0.8588c | 0.7255c | 0.6221c | 0.8443c | 0.7751c | 0.5262c | 0.9535c |
| SCL-ANX | 0.4233b | 0.2744 | 0.6568c | 0.5145c | 0.5977c | 0.7555b | 0.6119c | 0.8588c | - | 0.7571c | 0.4613b | 0.6853c | 0.6115c | 0.5563c | 0.8535c |
| SCL-HOS | 0.3454a | 0.2194 | 0.4417b | 0.4041b | 0.7221c | 0.7149c | 0.6796c | 0.7255c | 0.7571c | - | 0.5406c | 0.6628c | 0.6504c | 0.5008c | 0.8195c |
| SCL-PHOB | 0.1706 | 0.2133 | 0.2841 | 0.3112a | 0.6816c | 0.5539c | 0.6925c | 0.6221c | 0.4613b | 0.5406c | - | 0.5855c | 0.6864c | 0.295 | 0.7034c |
| SCL-PAR | 0.4185b | 0.2297 | 0.4448b | 0.5736c | 0.6684c | 0.8873c | 0.8046c | 0.8443c | 0.6853c | 0.6628c | 0.5855c | - | 0.8686c | 0.6187c | 0.9035c |
| SCL-PSY | 0.1675 | 0.1519 | 0.2532 | 0.3359a | 0.652c | 0.6972c | 0.7961c | 0.7751c | 0.6115c | 0.6504c | 0.6864c | 0.8686c | - | 0.4808b | 0.8479c |
| SCL-SLEEP | 0.6013c | 0.3224a | 0.4705b | 0.5024c | 0.6091c | 0.5762c | 0.396b | 0.5262c | 0.5563c | 0.5008c | 0.295 | 0.6187c | 0.4808b | - | 0.6395c |
| SCL-GSI | 0.458b | 0.2858 | 0.574c | 0.5644c | 0.8345c | 0.9174c | 0.8512c | 0.9535c | 0.8535c | 0.8195c | 0.7034c | 0.9035c | 0.8479c | 0.6395c | - |
In the current study, we investigated pregnancy-related depression, anxiety, and psychopathology in two distinct samples. One sample was assessed during the pre-COVID-19 period and the other during the COVID-19 restriction period. We found that the COVID-19 group of pregnant women scored lower on state anxiety than the pre-COVID-19 group. The two groups did not differ for their baseline characteristics, save for the type of support that the women received during their pregnancy, where the prevailing modality turned to multiple in COVID-19 times.
We would have expected greater psychopathology in the post-restriction COVID-19 sample of pregnant women, as reports mostly indicated a rise in anxiety[55], depression[56,57], sleep disorders[58], and post-traumatic symptoms[59,60]. In fact, in a meta-analysis, Yan et al[61] found pregnant women during the COVID-19 pandemic to have a higher relative risk for cumulative anxiety/ depression than women in the same locations before the pandemic. Another meta-analysis found increased anxiety from the pre-pandemic to the COVID-19 pandemic period in perinatal women, but the increase in depression was not significant[62]. We here found a decreased score of state anxiety in pregnant women amidst the pandemic period that could point to pregnant women feeling worse in better times, a paradoxical finding indeed.
In our sample, 4 of 21 (19.05%) pregnant women in the pre-COVID-19 sample and 2 of 22 (9.09%) pregnant women in the COVID-19 sample met criteria for clinically significant depression (total EPDS score ≥ 13). These results are dissimilar from those of a Turkish study, which found 35.4% of pregnant women in COVID-19 times to score ≥ 13[63], and from those of a Canadian survey, which found 37% depression and 57% anxiety[64]. The results of a large multinational study[65] were less alarming and more similar to ours, with 15% EPDS-assessed depression during pregnancy and 11% GAD-7–measured anxiety. We found 52.38% of the pre-COVID-19 sample and 81.82% from the COVID-19 sample to score low on anxiety, 28.57% of pre-COVID-19 and 18.18% of the COVID-19 sample to score moderate, and 19.05% of pre-COVID-19 participants and 0% of the COVID-19 group to score high on anxiety. This does not compare with those of Preis et al[66], who found 21.1% of their pregnant women during COVID-19 with no-to-minimal anxiety symptoms, 35.6% with mild anxiety, 21.6% with moderate anxiety, and 21.7% with severe anxiety. This cannot be due only to the different instruments used (we used the STAI-Y and they used the GAD-7).
Another Turkish study found even higher anxiety levels in pregnant women (62.6%), even though the proportion was less than that of the non-pregnant women (72.3%)[67]; these authors used the same tool to assess anxiety as we did, i.e., the STAI-Y, the same used by an Italian study which found a 68% prevalence of anxiety[68]. However, these authors assessed women in all trimesters of pregnancy, while we included women in the 2nd and 3rd trimesters. Saccone et al[68] found anxiety symptoms to be more severe during the first trimester, so it is possible that part of the difference could be attributed to the timing of the sampling. Furthermore, they used a less stringent cutoff than Yassa et al[67]. These large differences might be attributed to the different settings, methodologies, and cultural factors. Our results are more similar to those of a Chinese study, which found low rates of both anxiety and depression in pregnant women during COVID-19, that were lower than those of non-pregnant women[69]. These results match our idea that during difficulties, pregnant women recruit psychological resources allowing them to better address their new needs. Our results do not match those of a large meta-analysis, which found proportions of 30% for depression, 34% for anxiety, and 18% for comorbid depression and anxiety[70], while similar rates for both anxiety (31.9%) and depression (31.4%) were found by another meta-analysis of studies conducted during the early phase of the pandemic[71]. It should be said that our pre-pandemic period much overlaps with the early pandemic phase of most Chinese studies. In fact, in a study by Wu T et al[71], 62 studies were Chinese out of a total of 66.
We found that social support for pregnant women was different between the pre-COVID-19 and COVID-19 pandemic periods, in that pregnant women before the pandemic tended to rely more on partner support than on other types of support, while in the pandemic period had turned to a multiple support type. This does not mean that they received less support from their partners, but rather that they used additional support from their environment. This could be the result of a greater social cohesion under the threat of the pandemic or be related to other pandemic-related factors. For example, during the pandemic, access to pregnant women by their support providing figures is restricted[72], so it could be that women during this period turn to whatever support they may find. Lower perceived support, as measured through the Multidimensional Scale of Perceived Social Support, has been reported in Ireland among pregnant women during the pandemic[73]. Here we did not find reduced support compared to the previous pre-pandemic period by assessing support through direct interview, but rather a redistribution between social support types. It is possible that beyond different methodological differences, there are cultural and other reasons that underpin the difference between the two European countries. Social support in pregnant women has been investigated in northern Italy in one study[74], and was found to correlate negatively to depression and anxiety; however, this study quantified the extent of social support without focusing on support pattern as we did. Support has been shown to reduce anxiety in pregnant women during the pandemic in various studies assessing it through specific scales[16,75-77]. The way that we collected social support data (categories) prevented us from correlating them with anxiety scores, but it is possible that the high support perceived by women in our sample could match the lower than expected anxiety levels. Both samples, especially the pre-pandemic one, had higher rates of occurrence of psychopathology than the normally expected. Since there has been a high rate of refusal to complete the questionnaires, it is possible that there has been a selection bias, in that only women who were aware of having psychopathological problems that were prompted to adhere to the study.
The SCL-90R has been used in pregnant women to assess psychopathology in a number of studies also in the COVID-19 period. One Spanish study compared pre-pandemic to COVID-19 pandemic pregnant women and found more depression, insomnia, and phobic anxiety in the COVID-19 pandemic sample[78]. In a Chinese study comparing pregnant healthcare workers with pregnant women from the general population, higher prevalence rates of psychological symptoms of SCL-90R somatization, anxiety, and hostility were found among pregnant healthcare workers[79]. An Italian study of a COVID-19 pandemic sample found high SCL-90R global scores[80], which we did not find.
The small sample size and the fact that each participant was not her own control limit the generalisability of results. The cross-sectional nature of the design further limits the generalisation of the results. A strength of this study is that it compared two temporally near samples, one aware and one unaware of COVID-19. There are few studies comparing the two periods. A longitudinal design could have drawn better data. Women testing positive for COVID-19 have shown a peculiar pattern of anxiety and depression curves, with anxiety scores rapidly decreasing and returning to baseline levels, while depressive scores tended to subside more sluggishly[81]. Our data are limited to women testing negative for COVID-19 and may not extend to those testing positive; however, the latter showed similar rates of anxiety and depression in a case-control study[82]. To address multiple testing and control for type-I statistical error, we applied the extremely conservative Bonferroni correction[53], which is, however, too conservative and may be exposed to type-II error; however, the obtained results dispelled the possibility that potentially significant results could go undetected due to excessive restriction of the significance cutoff. Furthermore, we did not quantify social support through specifically dedicated scales, but rather we focused on support pattern. This may be a limitation, but focusing on pattern, which is an important characteristic of social support, may constitute a strength of our study.
The studies that focused on maternal mental health during the COVID-19 pandemic period, just as other projected or data-driven studies, are extremely rapidly accumulating, but their quality is heterogeneous. They alternate small sample sizes like ours with huge databases. The COVID-19 pandemic led to an increase in publications about COVID-19 with few or ill-collected data on which others commented. While some recognised the lack of appropriately collected data (“It may take time to generate sufficient and sound evidence”), they nevertheless went on to state “but we can safely speculate that pregnant women are at increased risk of developing mental health problems such as depression, anxiety, and post-traumatic stress symptoms”[83]. Future studies should employ longitudinal designs and verify not only the course of anxiety, depression, stress, and posttraumatic stress disorder-related symptoms, and sleep problems, but also psychotic symptoms in women who are pregnant and in those who are not. The timing of testing is important, as women’s responses are moulded though the media and responsible professional information provision and mental health markers may wax and wane during the pandemic on the basis of global response[81]. Another important point is the use of specific ins
The real effects of the pandemic are difficult to assess if adequate instruments are not used. Social isolation and COVID-19 threat may affect mood in pregnancy unpredictably, as they may both improve or worsen it, improve or deteriorate relationships with others[84], or recruit human resources that help overcome pandemic-related stress[22].
The coronavirus disease 2019 (COVID-19) pandemic impacted women’s mental health, particularly the pregnant population. The greater vulnerability of women during the COVID-19 restriction period may translate into a greater risk for mental disorders in the gestational period.
We hypothesised that pregnant women in the pre-pandemic period would have less psychopathology and more psychological support than pregnant women during the pandemic restriction period.
To compare pregnant women for anxiety, prenatal depression, psychopathology, and social support before and after the awareness of the pandemic.
We administered to pregnant women the Edinburgh Postnatal Depression Scale, the State-Trait Anxiety Inventory Form Y, and the Symptom CheckList-90-Revised before the COVID-19 outbreak (nonCOVID-19 sample) and after the COVID-19–related restrictive measures (COVID-19 sample). We further collected sociodemographic variables and explored women’s social support.
The nonCOVID-19 group reported higher support from partners only, while the COVID-19 group reported multiple support; the nonCOVID-19 group scored higher than the COVID-19 group only on state anxiety, while other measures did not differ meaningfully between the two groups. Our results do not confirm increased depression and anxiety rates in pregnant women during the pandemic.
Social support may have produced anxiolysis in the COVID-19 sample.
Future studies focusing on maternal mental health during the COVID-19 pandemic period should employ longitudinal designs and verify the course of anxiety, depression, stress, and post-traumatic stress-related symptoms, sleep problems, and psychotic symptoms in women who are pregnant and in those who are not. Particular attention should be paid to the timing of testing, the use of specific instruments for depression and anxiety in the perinatal period, and the effects of social isolation and COVID-19 threat on mood.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: He Z, China; Hosoya S, Japan; Tolunay HE, Turkey S-Editor: Xing YX L-Editor: Wang TQ P-Editor: Xing YX
| 1. | Amerio A, Lugo A, Stival C, Fanucchi T, Gorini G, Pacifici R, Odone A, Serafini G, Gallus S. COVID-19 Lockdown impact on mental health in a large representative sample of Italian adults. J Affect Disord. 2021;292:398-404. [PubMed] [DOI] [Full Text] |
| 2. | Al Dhaheri AS, Bataineh MF, Mohamad MN, Ajab A, Al Marzouqi A, Jarrar AH, Habib-Mourad C, Abu Jamous DO, Ali HI, Al Sabbah H, Hasan H, Stojanovska L, Hashim M, Abd Elhameed OA, Shaker Obaid RR, ElFeky S, Saleh ST, Osaili TM, Cheikh Ismail L. Impact of COVID-19 on mental health and quality of life: Is there any effect? PLoS One. 2021;16:e0249107. [PubMed] [DOI] [Full Text] |
| 3. | Chen YY, Wu KC, Gau SS. Mental health impact of the COVID-19 pandemic in Taiwan. J Formos Med Assoc. 2021;120:1421-1423. [PubMed] [DOI] [Full Text] |
| 4. | Duan H, Yan L, Ding X, Gan Y, Kohn N, Wu J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: Changes, predictors and psychosocial correlates. Psychiatry Res. 2020;293:113396. [PubMed] [DOI] [Full Text] |
| 5. | Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883-892. [PubMed] [DOI] [Full Text] |
| 6. | Gloster AT, Lamnisos D, Lubenko J, Presti G, Squatrito V, Constantinou M, Nicolaou C, Papacostas S, Aydın G, Chong YY, Chien WT, Cheng HY, Ruiz FJ, Garcia-Martin MB, Obando-Posada DP, Segura-Vargas MA, Vasiliou VS, McHugh L, Höfer S, Baban A, Dias Neto D, Nunes da Silva A, Monestès JL, Alvarez-Galvez J, Paez-Blarrina M, Montesinos F, Valdivia-Salas S, Ori D, Kleszcz B, Lappalainen R, Ivanović I, Gosar D, Dionne F, Merwin RM, Kassianos AP, Karekla M. Impact of COVID-19 pandemic on mental health: An international study. PLoS One. 2020;15:e0244809. [PubMed] [DOI] [Full Text] |
| 7. | Haesebaert F, Haesebaert J, Zante E, Franck N. Who maintains good mental health in a locked-down country? Health Place. 2020;66:102440. [PubMed] [DOI] [Full Text] |
| 8. | González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, Muñoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020;87:172-176. [PubMed] [DOI] [Full Text] |
| 9. | Massad I, Al-Taher R, Massad F, Al-Sabbagh MQ, Haddad M, Abufaraj M. The impact of the COVID-19 pandemic on mental health: early quarantine-related anxiety and its correlates among Jordanians. East Mediterr Health J. 2020;26:1165-1172. [PubMed] [DOI] [Full Text] |
| 10. | Lipskaya-Velikovsky L. COVID-19 Isolation in Healthy Population in Israel: Challenges in Daily Life, Mental Health, Resilience, and Quality of Life. Int J Environ Res Public Health. 2021;18. [PubMed] [DOI] [Full Text] |
| 11. | Lee CM, Cadigan JM, Rhew IC. Increases in Loneliness Among Young Adults During the COVID-19 Pandemic and Association With Increases in Mental Health Problems. J Adolesc Health. 2020;67:714-717. [PubMed] [DOI] [Full Text] |
| 12. | Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, Leyland A, Pearce A, Thomson R, Whitley E, Katikireddi SV. Mental health and health behaviours before and during the initial phase of the COVID-19 Lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021;75:224-231. [PubMed] [DOI] [Full Text] |
| 13. | BARRY MJ Jr. Depression, shame, loneliness, and the psychiatrist's position. Am J Psychother. 1962;16:580-590. [PubMed] [DOI] [Full Text] |
| 14. | Ginter EJ, Glauser A, Richmond BO. Loneliness, social support, and anxiety among two South Pacific cultures. Psychol Rep. 1994;74:875-879. [PubMed] [DOI] [Full Text] |
| 15. | Wu J, Wu Y, Tian Y. Temporal associations among loneliness, anxiety, and depression during the COVID-19 pandemic period. Stress Health. 2021;. [PubMed] [DOI] [Full Text] |
| 16. | Harrison V, Moulds ML, Jones K. Perceived social support and prenatal wellbeing; The mediating effects of loneliness and repetitive negative thinking on anxiety and depression during the COVID-19 pandemic. Women Birth. 2021;. [PubMed] [DOI] [Full Text] |
| 17. | Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women's mental health. Arch Womens Ment Health. 2020;23:741-748. [PubMed] [DOI] [Full Text] |
| 18. | Goyal D, Selix NW. Impact of COVID-19 on Maternal Mental Health. MCN Am J Matern Child Nurs. 2021;46:103-109. [PubMed] [DOI] [Full Text] |
| 19. | Dib S, Rougeaux E, Vázquez-Vázquez A, Wells JCK, Fewtrell M. Maternal mental health and coping during the COVID-19 Lockdown in the UK: Data from the COVID-19 New Mum Study. Int J Gynaecol Obstet. 2020;151:407-414. [PubMed] [DOI] [Full Text] |
| 20. | López-Morales H, Del Valle MV, Canet-Juric L, Andrés ML, Galli JI, Poó F, Urquijo S. Mental health of pregnant women during the COVID-19 pandemic: A longitudinal study. Psychiatry Res. 2021;295:113567. [PubMed] [DOI] [Full Text] |
| 21. | Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. Coping strategies mediate the associations between COVID-19 experiences and mental health outcomes in pregnancy. Arch Womens Ment Health. 2021;24:1007-1017. [PubMed] [DOI] [Full Text] |
| 22. | Yarrington JS, Lasser J, Garcia D, Vargas JH, Couto DD, Marafon T, Craske MG, Niles AN. Impact of the COVID-19 Pandemic on Mental Health among 157,213 Americans. J Affect Disord. 2021;286:64-70. [PubMed] [DOI] [Full Text] |
| 23. | Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-786. [PubMed] [DOI] [Full Text] |
| 24. | Murray D, Cox JL. Screening for depression during pregnancy with the Edinburgh depression scale (EPDS). J Reprod Infant Psychol. 1990;8:99-107. |
| 25. | McBride HL, Wiens RM, McDonald MJ, Cox DW, Chan EKH. The Edinburgh Postnatal Depression Scale (EPDS): A review of the reported validity evidence. In: Zumbo BD, Chan EKH (Eds.) Validity and Validation in Social, Behavioral, and Health Sciences. Social Indicators Research Series 54. Cham (CH): Springer International Publishing, 2014: 157-174. |
| 26. | Murray L, Carothers AD. The validation of the Edinburgh Post-natal Depression Scale on a community sample. Br J Psychiatry. 1990;157:288-290. [PubMed] [DOI] [Full Text] |
| 27. | Zelkowitz P, Milet TH. Screening for post-partum depression in a community sample. Can J Psychiatry. 1995;40:80-86. [PubMed] [DOI] [Full Text] |
| 28. | Carpiniello B, Pariante CM, Serri F, Costa G, Carta MG. Validation of the Edinburgh Postnatal Depression Scale in Italy. J Psychosom Obstet Gynaecol. 1997;18:280-285. [PubMed] [DOI] [Full Text] |
| 29. | Benvenuti P, Ferrara M, Niccolai C, Valoriani V, Cox JL. The Edinburgh Postnatal Depression Scale: validation for an Italian sample. J Affect Disord. 1999;53:137-141. [PubMed] [DOI] [Full Text] |
| 30. | Ross LE, Gilbert Evans SE, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: anxiety as a feature of postpartum depression. Arch Womens Ment Health. 2003;6:51-57. [PubMed] [DOI] [Full Text] |
| 31. | Matthey S. Using the Edinburgh Postnatal Depression Scale to screen for anxiety disorders. Depress Anxiety. 2008;25:926-931. [PubMed] [DOI] [Full Text] |
| 32. | Phillips J, Charles M, Sharpe L, Matthey S. Validation of the subscales of the Edinburgh Postnatal Depression Scale in a sample of women with unsettled infants. J Affect Disord. 2009;118:101-112. [PubMed] [DOI] [Full Text] |
| 33. | Swalm D, Brooks J, Doherty D, Nathan E, Jacques A. Using the Edinburgh postnatal depression scale to screen for perinatal anxiety. Arch Womens Ment Health. 2010;13:515-522. [PubMed] [DOI] [Full Text] |
| 34. | Matthey S, Fisher J, Rowe H. Using the Edinburgh postnatal depression scale to screen for anxiety disorders: conceptual and methodological considerations. J Affect Disord. 2013;146:224-230. [PubMed] [DOI] [Full Text] |
| 35. | Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JR. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2016;16:72. [PubMed] [DOI] [Full Text] |
| 36. | Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the State-Trait-Anxiety Inventory: STAI (Form Y). Palo Alto (CA): Consulting Psychologists Press, 1983. |
| 37. | Cattell RB, Scheier IH. The nature of anxiety: a review of thirteen multivariate analyses comprising 814 variables. Psychol Rep. 1958;4:351-388. |
| 38. | Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Tallahassee (FL): Florida State University, 1968. |
| 39. | Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto (CA): Consulting Psychologists Press, 1970. |
| 40. | González-Fraile E, Domínguez-Panchón AI, Fernández-Catalina P, Gonçalves-Pereira M. [The different versions of the State-Trait Anxiety Inventory]. Rev Psiquiatr Salud Ment. 2014;7:151-152. [PubMed] [DOI] [Full Text] |
| 41. | Seok CB, Abd Hamid HS, Mutang JA, Ismail R. Psychometric properties of the State-Trait Anxiety Inventory (Form Y) among Malaysian university students. Sustainability. 2018;10:3311. |
| 42. | Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S467-S472. [PubMed] [DOI] [Full Text] |
| 43. | Kayikcioglu O, Bilgin S, Seymenoglu G, Deveci A. State and Trait Anxiety Scores of Patients Receiving Intravitreal Injections. Biomed Hub. 2017;2:1-5. [PubMed] [DOI] [Full Text] |
| 44. | Wiglusz MS, Landowski J, Cubała WJ. Psychometric properties and diagnostic utility of the State-Trait Anxiety Inventory in epilepsy with and without comorbid anxiety disorder. Epilepsy Behav. 2019;92:221-225. [PubMed] [DOI] [Full Text] |
| 45. | Derogatis LR. Symptom Checklist-90-R: Administration, Scoring and Procedures Manual, 3rd ed. Minneapolis (MN): National Computer Systems; 1994. |
| 46. | Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19:1-15. [PubMed] [DOI] [Full Text] |
| 47. | Hughes JM, Ulmer CS, Gierisch JM; Mid-Atlantic VA MIRECC Workgroup, Howard MO. Single-Item Measures for Detecting Sleep Problems in United States Military Veterans. J Gen Intern Med. 2018;33:698-704. [PubMed] [DOI] [Full Text] |
| 48. | Prunas A, Sarno I, Preti E, Madeddu F, Perugini M. Psychometric properties of the Italian version of the SCL-90-R: a study on a large community sample. Eur Psychiatry. 2012;27:591-597. [PubMed] [DOI] [Full Text] |
| 49. | Rytilä-Manninen M, Fröjd S, Haravuori H, Lindberg N, Marttunen M, Kettunen K, Therman S. Psychometric properties of the Symptom Checklist-90 in adolescent psychiatric inpatients and age- and gender-matched community youth. Child Adolesc Psychiatry Ment Health. 2016;10:23. [PubMed] [DOI] [Full Text] |
| 50. | Schauenburg H, Strack M. Measuring psychotherapeutic change with the symptom checklist SCL 90 R. Psychother Psychosom. 1999;68:199-206. [PubMed] [DOI] [Full Text] |
| 51. | Ignatyev Y, Fritsch R, Priebe S, Mundt AP. Psychometric properties of the symptom check-list-90-R in prison inmates. Psychiatry Res. 2016;239:226-231. [PubMed] [DOI] [Full Text] |
| 52. | Shapiro SS, Wilk MB. An analysis of variance test for normality (Complete samples). Biometrika. 1965;52:591-611. |
| 53. | Bonferroni CE. Teoria statistica delle classi e calcolo delle probabilità [Statistical theory of classess and probability calculation]. Florence, Italy: Pubblicazioni del Real Istituto Superiore di Scienze Economiche e Commerciali di Firenze, 1936. |
| 54. | Curtin F, Schulz P. Multiple correlations and Bonferroni's correction. Biol Psychiatry. 1998;44:775-777. [PubMed] [DOI] [Full Text] |
| 55. | Mappa I, Distefano FA, Rizzo G. Effects of coronavirus 19 pandemic on maternal anxiety during pregnancy: a prospectic observational study. J Perinat Med. 2020;48:545-550. [PubMed] [DOI] [Full Text] |
| 56. | Ayaz R, Hocaoğlu M, Günay T, Yardımcı OD, Turgut A, Karateke A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J Perinat Med. 2020;48:965-970. [PubMed] [DOI] [Full Text] |
| 57. | Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, Li H, Chen L, Xu H, Li X, Guo Y, Wang Y, Li J, Zhang T, You Y, Yang S, Tao X, Xu Y, Lao H, Wen M, Zhou Y, Wang J, Chen Y, Meng D, Zhai J, Ye Y, Zhong Q, Yang X, Zhang D, Zhang J, Wu X, Chen W, Dennis CL, Huang HF. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol. 2020;223:240.e1-240.e9. [PubMed] [DOI] [Full Text] |
| 58. | Lin W, Wu B, Chen B, Lai G, Huang S, Li S, Liu K, Zhong C, Huang W, Yuan S, Wang Y. Sleep Conditions Associate with Anxiety and Depression Symptoms among Pregnant Women during the Epidemic of COVID-19 in Shenzhen. J Affect Disord. 2021;281:567-573. [PubMed] [DOI] [Full Text] |
| 59. | Ravaldi C, Ricca V, Wilson A, Homer C, Vannacci A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during "lockdown" in Italy. Arch Womens Ment Health. 2020;23:783-786. [PubMed] [DOI] [Full Text] |
| 60. | Berthelot N, Lemieux R, Garon-Bissonnette J, Drouin-Maziade C, Martel É, Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet Gynecol Scand. 2020;99:848-855. [PubMed] [DOI] [Full Text] |
| 61. | Yan H, Ding Y, Guo W. Mental Health of Pregnant and Postpartum Women During the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. Front Psychol. 2020;11:617001. [PubMed] [DOI] [Full Text] |
| 62. | Hessami K, Romanelli C, Chiurazzi M, Cozzolino M. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Fetal Neonatal Med. 2020;1-8. [PubMed] [DOI] [Full Text] |
| 63. | Durankuş F, Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Matern Fetal Neonatal Med. 2020;1-7. [PubMed] [DOI] [Full Text] |
| 64. | Lebel C, MacKinnon A, Bagshawe M, Tomfohr-Madsen L, Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5-13. [PubMed] [DOI] [Full Text] |
| 65. | Ceulemans M, Foulon V, Ngo E, Panchaud A, Winterfeld U, Pomar L, Lambelet V, Cleary B, O'Shaughnessy F, Passier A, Richardson JL, Hompes T, Nordeng H. Mental health status of pregnant and breastfeeding women during the COVID-19 pandemic-A multinational cross-sectional study. Acta Obstet Gynecol Scand. 2021;100:1219-1229. [PubMed] [DOI] [Full Text] |
| 66. | Preis H, Mahaffey B, Heiselman C, Lobel M. Pandemic-related pregnancy stress and anxiety among women pregnant during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol MFM. 2020;2:100155. [PubMed] [DOI] [Full Text] |
| 67. | Yassa M, Yassa A, Yirmibeş C, Birol P, Ünlü UG, Tekin AB, Sandal K, Mutlu MA, Çavuşoğlu G, Tug N. Anxiety levels and obsessive compulsion symptoms of pregnant women during the COVID-19 pandemic. Turk J Obstet Gynecol. 2020;17:155-160. [PubMed] [DOI] [Full Text] |
| 68. | Saccone G, Florio A, Aiello F, Venturella R, De Angelis MC, Locci M, Bifulco G, Zullo F, Di Spiezio Sardo A. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol. 2020;223:293-295. [PubMed] [DOI] [Full Text] |
| 69. | Zhou Y, Shi H, Liu Z, Peng S, Wang R, Qi L, Li Z, Yang J, Ren Y, Song X, Zeng L, Qian W, Zhang X. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl Psychiatry. 2020;10:319. [PubMed] [DOI] [Full Text] |
| 70. | Sun F, Zhu J, Tao H, Ma Y, Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J Psychosom Obstet Gynaecol. 2021;42:91-99. [PubMed] [DOI] [Full Text] |
| 71. | Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, Wang X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord. 2021;281:91-98. [PubMed] [DOI] [Full Text] |
| 72. | Vasilevski V, Sweet L, Bradfield Z, Wilson AN, Hauck Y, Kuliukas L, Homer CSE, Szabo RA, Wynter K. Receiving maternity care during the COVID-19 pandemic: Experiences of women's partners and support persons. Women Birth. 2021;. [PubMed] [DOI] [Full Text] |
| 73. | Matvienko-Sikar K, Pope J, Cremin A, Carr H, Leitao S, Olander EK, Meaney S. Differences in levels of stress, social support, health behaviours, and stress-reduction strategies for women pregnant before and during the COVID-19 pandemic, and based on phases of pandemic restrictions, in Ireland. Women Birth. 2021;34:447-454. [PubMed] [DOI] [Full Text] |
| 74. | Grumi S, Provenzi L, Accorsi P, Biasucci G, Cavallini A, Decembrino L, Falcone R, Fazzi EM, Gardella B, Giacchero R, Guerini P, Grossi E, Magnani ML, Mariani EM, Nacinovich R, Pantaleo D, Pisoni C, Prefumo F, Sabatini C, Scelsa B, Spartà MV, Spinillo A, Giorda R, Orcesi S, Borgatti R. Depression and Anxiety in Mothers Who Were Pregnant During the COVID-19 Outbreak in Northern Italy: The Role of Pandemic-Related Emotional Stress and Perceived Social Support. Front Psychiatry. 2021;12:716488. [PubMed] [DOI] [Full Text] |
| 75. | Yue C, Liu C, Wang J, Zhang M, Wu H, Li C, Yang X. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: The mediating effect of risk perception. Int J Soc Psychiatry. 2021;67:120-127. [PubMed] [DOI] [Full Text] |
| 76. | Behmard V, Bahri N, Mohammadzadeh F, Noghabi AD. Relationships between anxiety induced by COVID-19 and perceived social support among Iranian pregnant women. J Psychosom Obstet Gynaecol. 2021;1-8. [PubMed] [DOI] [Full Text] |
| 77. | Brik M, Sandonis MA, Fernández S, Suy A, Parramon-Puig G, Maiz N, Dip ME, Ramos-Quiroga JA, Carreras E. Psychological impact and social support in pregnant women during lockdown due to SARS-CoV2 pandemic: A cohort study. Acta Obstet Gynecol Scand. 2021;100:1026-1033. [PubMed] [DOI] [Full Text] |
| 78. | Puertas-Gonzalez JA, Mariño-Narvaez C, Peralta-Ramirez MI, Romero-Gonzalez B. The psychological impact of the COVID-19 pandemic on pregnant women. Psychiatry Res. 2021;301:113978. [PubMed] [DOI] [Full Text] |
| 79. | Liu M, Li N, Cai X, Feng X, Wang R, Xiong P. The Prevalence of Psychological Symptoms in Pregnant Healthcare Workers (HCWs) and Pregnant Non-HCWs During the Early Stage of COVID-19 Pandemic in Chongqing, China. Front Psychiatry. 2021;12:708698. [PubMed] [DOI] [Full Text] |
| 80. | Di Buò A, Moretti P, Menculini G, Minuti A, Valentini E, Cerasoli I, Mancini N, Moro B, Radici S, Gerli S, Tortorella A. Antepartum Distress during COVID-19 Pandemic: an Observational Study. Psychiatr Danub. 2021;33:137-141. [PubMed] |
| 81. | Kotabagi P, Fortune L, Essien S, Nauta M, Yoong W. Anxiety and depression levels among pregnant women with COVID-19. Acta Obstet Gynecol Scand. 2020;99:953-954. [PubMed] [DOI] [Full Text] |
| 82. | Kotabagi P, Nauta M, Fortune L, Yoong W. COVID-19 positive mothers are not more anxious or depressed than non COVID pregnant women during the pandemic: A pilot case-control comparison. Eur J Obstet Gynecol Reprod Biol. 2020;252:615-616. [PubMed] [DOI] [Full Text] |
| 83. | Thapa SB, Mainali A, Schwank SE, Acharya G. Maternal mental health in the time of the COVID-19 pandemic. Acta Obstet Gynecol Scand. 2020;99:817-818. [PubMed] [DOI] [Full Text] |
| 84. | Milne SJ, Corbett GA, Hehir MP, Lindow SW, Mohan S, Reagu S, Farrell T, O'Connell MP. Effects of isolation on mood and relationships in pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;252:610-611. [PubMed] [DOI] [Full Text] |