Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6314
Peer-review started: December 31, 2021
First decision: January 23, 2022
Revised: January 27, 2021
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: June 26, 2022
Processing time: 167 Days and 12.4 Hours
Acute lower gastrointestinal bleeding is common in clinical practice, and the colon is responsible for the majority of cases. However, appendiceal bleeding is an extremely rare cause. Appendiceal bleeding due to vascular diseases, such as angiodysplasia and Dieulafoy’s lesion, may result in massive lower gast
A 32-year-old male presented to our hospital with hematochezia that had lasted for 6 h, with approximately 600-800 mL bloody stools and loss of consciousness for a few seconds. Persistent bleeding from the orifice of the appendix was observed by colonoscopy. Following the new diagnosis of appendiceal bleeding, the patient was treated by an emergency laparoscopic appendectomy. Finally, the patient was pathologically diagnosed with appendiceal Dieulafoy’s lesion. The patient was uneventfully discharged, and follow-up 2 wk later showed no evidence of rebleeding.
Although appendiceal bleeding is a rare cause of acute lower gastrointestinal bleeding, clinicians should consider it during differential diagnosis.
Core Tip: Appendiceal bleeding is a rare cause of acute lower gastrointestinal bleeding. Appendiceal bleeding due to vascular diseases, such as angiodysplasia and Dieulafoy’s lesion, may result in massive lower gastrointestinal bleeding. Appendectomy is a reliable and effective option for treatment.We report a case of lower gastrointestinal bleeding due to appendiceal Dieulafoy’s lesion. The patient recovered well after an emergency laparoscopic appendectomy. Clinicians should consider appendiceal bleeding during differential diagnosis.
- Citation: Zhou SY, Guo MD, Ye XH. Appendiceal bleeding: A case report. World J Clin Cases 2022; 10(18): 6314-6318
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6314.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6314
The common causes of lower gastrointestinal bleeding are mostly known to be diseases of the colon, rectum, and terminal ileum[1]. However, appendiceal bleeding as the origin is extremely rare. Diverticulum, angiodysplasia, inflammation, and neoplasm are the usual etiologies for appendiceal bleeding[2,3]. Vascular diseases, such as angiodysplasia and Dieulafoy’s lesion, are one of the most common causes of massive bleeding and sometimes can be life-threatening[1,4]. We report herein a case of lower gastrointestinal bleeding due to appendiceal Dieulafoy’s lesion, with a literature review.
A 32-year-old male presented to the emergency department of our hospital with hematochezia that had lasted for 6 h.
The patient reported having experienced approximately 600-800 mL bloody stools before presentation to the hospital. The patient also reported having experienced loss of consciousness for a few seconds. No other gastrointestinal symptoms, such as nausea, vomiting, or abdominal pain, were experienced during the process. The patient denied past history of hematochezia.
The patient had been previously diagnosed with hemorrhoids and hypertension, but was taking no medications.
The personal and family history-taking revealed no information relevant to the current case.
The patient’s temperature was 36.5 °C, heart rate was 95 beats per minute, respiratory rate was 20 breaths per minute, blood pressure (measured with electronic cuff) was 147/105 mmHg, and oxygen saturation in room air was 99%. The physical examination showed an anemic appearance, without any other pathological signs.
The laboratory tests showed that hemoglobin was 102 g/L (normal range: 130-175 g/L), revealing a mild anemia. Other routine relevant examinations, such as platelet counts and for markers of coagulation function, and liver and renal function, yielded normal findings. Unfortunately, the patient passed bloody stools again 1 d after conservative treatment in our department, with his hemoglobin level dropping to 86 g/L.
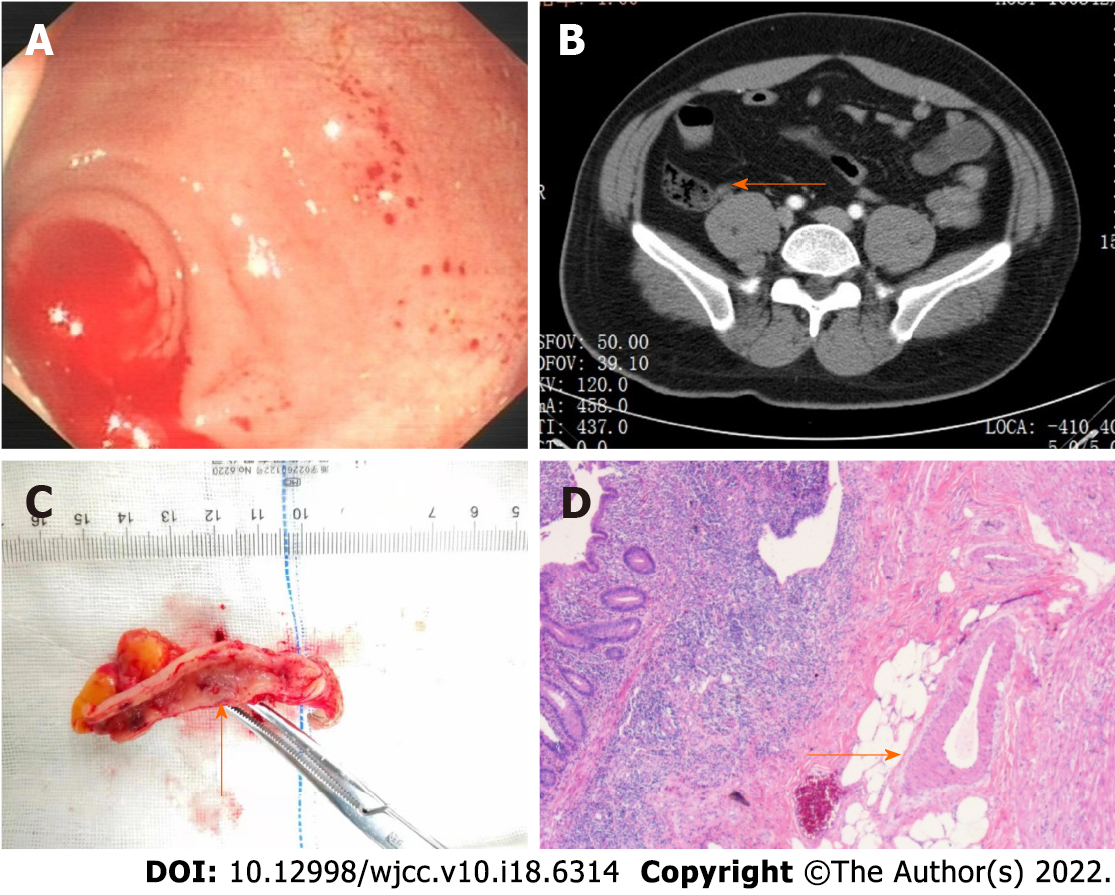
An emergency colonoscopy was performed, and extended up to the terminal ileum. During the procedure, blood clots in the cecum were first washed out and we were then able to observe a large quantity of fresh blood oozing out of the appendiceal orifice (Figure 1A). In addition, contrast-enhanced abdominal computed tomography (CT) scan showed a high-density area in the appendix without any signs of acute appendicitis, tumor, or diverticulum (Figure 1B).
Bleeding of the appendix.
We suspected that the source of bleeding was the appendix, which prompted an emergency laparoscopic appendectomy. During that surgery, no signs of acute appendicitis or diverticulitis were observed; however, a large amount of blood clots was observed through the longitudinal incision of the appendix. A vessel stump was also found on the mucosa of the appendix (Figure 1C). Pathologically, a caliber-persistent artery was detected near the vessel stump of the mucosa surface, corresponding to Dieulafoy’s lesion within the appendix (Figure 1D).
The patient had no recurrent hematochezia or melena, and was discharged from the hospital 6 d after the surgery. Follow-up 2 wk later showed no evidence of rebleeding.
Acute lower gastrointestinal bleeding is commonly encountered in clinical practice, with colon being responsible for the majority of cases[1]. Appendiceal bleeding, on the other hand, is an extremely rare cause, and as such may be missed or misdiagnosed.Although lower gastrointestinal bleeding is generally less severe than upper gastrointestinal bleeding - with spontaneous cessation of the bleeding occurring in most cases, appendiceal bleeding attributed to vascular diseases, such as angiodysplasia and Dieulafoy’s lesion, may result in massive lower gastrointestinal bleeding and sometimes can be life-threatening[1,4]. As a clinician, having an awareness of appendiceal bleeding is significant. A literature search of relevant articles on the PubMed/MEDLINE database, from January 1977 to November 2021, was conducted, using the key words of “appendix bleeding” or “appendix hemorrhage”. Six articles regarding appendiceal bleeding due to vascular diseases were identified (Table 1)[5-10].
| Case | Age/sex | Chief complaint | Hemoglobin, g/L | Techniques | Treatment | Pathology | Ref. |
| 1 | 21/female | Massive hematochezia | 106 | Endoscopy | Appendectomy | Dieulafoy’s lesion | [5] |
| 2 | 72/male | Hematochezia | 126 | Endoscopy | Appendectomy | Angiodysplasia | [6] |
| 3 | 68/male | Massive hematochezia | 82 | Endoscopy | Appendectomy | Dieulafoy’s lesion | [7] |
| 4 | 41/male | Melena | Not reported | Endoscopy | Appendectomy | Atypical florid vascular proliferation | [8] |
| 5 | 76/female | Massive hematochezia | 52 | Angiography | Vessel embolization and appendectomy | Angiodysplasia | [9] |
| 6 | 42/male | Melena | 77 | Endoscopy | Appendectomy | Vascular malformation | [10] |
| Our case | 32/male | Massive hematochezia | 86 | Endoscopy | Appendectomy | Dieulafoy’s lesion |
The average age of the included cases was 50.3 years (range: 21-76 years). In terms of sex, 5 males and 2 females are reported on herein. Similar to previous reports, the most likely cause of hospitalization was massive hematochezia, rather than melena[3]. Pathological analyses showed the main vascular factors of appendiceal bleeding to be angiodysplasia and Dieulafoy’s lesion. Dieulafoy’s lesion is caused by an abnormal artery that fails to diminish to the minute size of the mucosal capillary microvasculature[11]. The most common location of Dieulafoy’s lesion is the stomach. Others have reported Dieulafoy’s lesion in the esophagus, duodenum, small intestine, colon, and rectum[12-15]; however, an appendiceal Dieulafoy’s lesion is extremely rare. Among the included publications, there were only 2 cases of appendiceal bleeding due to Dieulafoy’s lesion published in English language[5,7], with ours being the third case.
Several modalities, such as colonoscopy, contrast-enhanced abdominal CT, and angiography, can be applied in diagnosing appendiceal bleeding[2,3,9]. In our case, colonoscopy directly revealed the active bleeding from the appendiceal orifice. For such cases, emergency colonoscopy for acute lower gastrointestinal bleeding should be utilized, at least to the terminal ileum. In addition, the orifice of the appendix should be carefully observed. Contrast-enhanced abdominal CT is useful in evaluating diverticulum, neoplasm, or acute inflammation. Although mesenteric artery angiography requires bleeding of more than 0.5 mL/min, vessel embolization is feasible in controlling acute bleeding[9].
A reliable and effective choice of treatment for appendiceal bleeding is appendectomy[2]. Other attempts, including vessel embolization and endoscopic therapy (therapeutic barium enema and endoclips), have been reported as successful for controlling bleeding[9,16,17]; however, the risk of acute appendicitis and rebleeding after vessel embolization and endoscopic therapy are unmanageable, and the patient may still require an appendectomy[9,17]. Studies for the feasibility of vessel embolization and endoscopic therapy continue to be warranted.
We present a treatment experience of appendiceal bleeding caused by Dieulafoy’s lesion. Although appendiceal bleeding is a rare cause of acute lower gastrointestinal bleeding, clinicians should consider it during differential diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bhusal U, Nepal; Kumar S, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Marion Y, Lebreton G, Le Pennec V, HournaE, Viennot S, Alves A. The management of lower gastrointestinal bleeding. J Visc Surg. 2014;151:191-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Maeda Y, Saito S, Ohuchi M, Tamaoki Y, Nasu J, Baba H. Appendiceal bleeding in an elderly male: a case report and a review of the literature. Surg Case Rep. 2021;7:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 3. | Chen W, Qiu H, Yang X, Zhang J. Appendix Bleeding with Painless Bloody Diarrhea: A Case Report and Literature Review. Open Med (Wars). 2019;14:735-739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Hoedema RE, Luchtefeld MA. The management of lower gastrointestinal hemorrhage. Dis Colon Rectum. 2005;48:2010-2024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Xue M, Weng WH, Wang LJ. An Unusual Cause of Acute Massive Lower Gastrointestinal Bleeding. Gastroenterology. 2020;158:1550-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Choi JM, Lee SH, Ahn BK, Baek SU. Hematochezia due to Angiodysplasia of the Appendix. Ann Coloproctol. 2016;32:117-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Reynolds JK, Mejia VA. Appendiceal Dieulafoy lesion: an unusual cause of massive lower gastrointestinal bleeding. Am Surg. 2015;81:E18-E19. [PubMed] |
| 8. | Gu MJ, Choi JH, Kim SH. Atypical florid vascular proliferation in appendix: a diagnostic dilemma. DiagnPathol. 2013;8:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kyokane T, Akita Y, Katayama M, Kitagawa Y, Sato T, Shichino S, Nimura Y. Angiodysplasia of the appendix. Am J Gastroenterol. 2001;96:242-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | So JB, Alexander DJ, Chong AP, Goh PM. Laparoscopic appendicectomy in the management of acute lower gastrointestinal bleeding. GastrointestEndosc. 1995;42:488-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Dieulafoy G. Exulceratio simplex. Bull Acad Med. 1898;39:49-84. |
| 12. | Inayat F, Ullah W, Hussain Q, Hurairah A. Dieulafoy's lesion of the oesophagus: a case series and literature review. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Inayat F, Amjad W, Hussain Q, Hurairah A. Dieulafoy's lesion of the duodenum: a comparative review of 37 cases. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Malik A, Inayat F, Goraya MHN, Almas T, Ishtiaq R, Malik S, Tarar ZI. Jejunal Dieulafoy's Lesion: A Systematic Review of Evaluation, Diagnosis, and Management. J Investig Med High Impact Case Rep. 2021;9:2324709620987703. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Inayat F, Ullah W, Hussain Q, Abdullah HMA. Dieulafoy's lesion of the colon and rectum: a case series and literature review. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Chung IH, Kim KH. A case of successful colonoscopic treatment of acute appendiceal bleeding by endoclips. J Korean Soc Coloproctol. 2011;27:329-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Smith EJ, Coventry C, Taylor J, De'ath H, Haque A. A case of endovascular management to gain control of a lower gastrointestinal haemorrhage caused by appendiceal artery bleeding. J Surg Case Rep. 2021;2021:rjab204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |