Published online Jun 26, 2022. doi: 10.12998/wjcc.v10.i18.6001
Peer-review started: December 27, 2021
First decision: January 25, 2022
Revised: February 24, 2022
Accepted: April 25, 2022
Article in press: April 25, 2022
Published online: June 26, 2022
Processing time: 171 Days and 17.2 Hours
Thoracolumbar fractures are generally combined with spinal cord injury to varying degrees, which may cause deterioration of the patients' condition and increase the difficulty of clinical treatment. At present, anterior or combined anterior-posterior surgery is preferred for severe thoracolumbar fractures.
To investigate the effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury.
One-hundred-and-twenty patients who received surgery for severe thoracolumbar fractures with spinal cord injury at our hospital from February 2018 to February 2020 were randomly enrolled. They were randomly divided into group 1 (one-stage combined anterior-posterior surgery, n = 60) and group 2 (one-stage anterior-approach surgery, n = 60). Treatment efficacy was compared between the two groups.
Blood loss was greater and the operation time was longer in group 1 than in group 2, and the differences were statistically significant (P < 0.05). Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups (P > 0.05). Preoperative function of the affected vertebrae was not significantly different between the two groups (P > 0.05). In each group, the patients showed significant improvement after surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2 (P < 0.05). The canal-occupying ratio of the affected vertebrae was not significantly different between the two groups (P > 0.05). Before surgery, there was no significant difference in the quality of life scores between the two groups (P > 0.05). The above indicators were significantly improved after surgery compared with before surgery in each group. In addition, these indicators were markedly better in group 1 than in group 2 after surgery (P < 0.05 for each).
One-stage combined anterior-posterior surgery effectively improves the function of the affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury. This surgical approach is worthy of popularization in clinical use.
Core Tip: One-stage combined anterior-posterior surgery can effectively improve the function of affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury. This surgical approach is worthy of popularization in clinical use. The one-stage combined anterior-posterior approach effectively restored the height of the affected vertebrae and corrected kyphosis. The one-stage combined anterior-posterior approach also allows for sufficient anterior decompression, and the simple anterior approach does not enable temporary fixation, auxiliary reduction, and three-column fixation according to Denis' three-column concept.
- Citation: Zhang B, Wang JC, Jiang YZ, Song QP, An Y. Effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury. World J Clin Cases 2022; 10(18): 6001-6008
- URL: https://www.wjgnet.com/2307-8960/full/v10/i18/6001.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i18.6001
Thoracolumbar fractures refer to fractures at the thoracolumbar spine, which are mainly featured by local thoracic spinal pain and swelling and muscle tension on both sides of the fracture. Patients with thoracolumbar fractures may have difficulty in standing and turning over. Some may even suffer from movement disorder and significant impairment of daily life activities. The incidence of thoracolumbar fractures is relatively high, and is a common trauma at the Department of Orthopedics. The diagnosis of this disorder has become easier and faster in China due to the continuous improvement in medical technology[1,2]. Thoracolumbar fractures are generally combined with spinal cord injury to varying degrees, which may cause deterioration of the patients' condition and increase the difficulty of clinical treatment. The reasons for this are as follows: The fractured blocks and the intervertebral disc tissues protrude into the spinal canal, resulting in spinal cord contusion and compression. Therefore, fracture reduction, spinal compression, and spinal fixation and fusion at the affected segments are crucial steps in surgery[3]. China has witnessed a rapid development of medical science in recent years, and the diagnosis of thoracolumbar fractures is more rapid, while the selection of an appropriate treatment has become a primary concern[4]. At present, anterior or combined anterior-posterior surgery is preferred for severe thoracolumbar fractures. In this study, the application value, advantages, and disadvantages of these two surgical approaches were compared by reviewing the data of patients with thoracolumbar fractures treated at our hospital.
The present study was approved by the hospital ethics committee. One hundred and twenty patients with severe thoracolumbar fractures and spinal cord injury treated at our hospital from February 2020 to February 2021 were randomly enrolled. The random sampling method was used to divide the patients into two groups, namely, group 1 and group 2, with 60 patients in each group. Informed consent was obtained from all patients. The two groups were not different significantly in terms of the basic information (P > 0.05) (Table 1).
| Groups | Male/female | Age (yr) | Causes of injury (Falling injury/traffic accidents/falling from heights) | Preoperative ASIA grade(B/C/D) | Frankel classification (A/B/C/D) | Preoperative AO classification (A3/B3/C2) | BMI (kg/m2) |
| Group 1 | 35/25 | 45.37 ± 4.24 | 13/32/15 | 13/22/25 | 13/18/15/14 | 13/35/12 | 23.75 ± 1.69 |
| Group 2 | 29/31 | 45.26 ± 4.09 | 16/29/15 | 12/20/28 | 15/20/12/13 | 15/30/15 | 23.84 ± 1.76 |
| χ2/t value | 1.205 | 0.145 | 0.4579 | 0.305 | 0.619 | 0.861 | 0.286 |
| P value | 0.272 | 0.885 | 0.7954 | 0.859 | 0.892 | 0.650 | 0.776 |
Inclusion criteria: (1) No conscious disturbance; (2) complete medical records; (3) thoracolumbar fractures confirmed by computed tomography (CT) or X-rays, combined with nerve injury; (4) fractured blocks occupying over 50% of the spinal canal; (5) patients tolerant to surgery; and (6) the degree of vertebral compression greater than 50%.
Exclusion criteria: (1) Cognitive impairment to varying degrees; (2) recent history of acute and chronic infections; (3) hearing impairment or incapable of communication; (4) pathological fractures caused by tumors, infections, or osteoporosis; (5) severe spinal degenerative diseases; and (6) history of drug dependence or drug allergy.
Patients in group 2 received anterior decompression plus bone grafting with internal fixation. General anesthesia was performed in the lateral position. A lateral-anterior extra-pleuroperitoneal approach was adopted to expose the affected vertebrae and the adjacent vertebrae. The ribs were resected selectively to prepare the bone graft. The lateral portion of the pedicle of the affected vertebral body was resected to expose the dural sac and nerve root sleeve fully. The posterior 3/4 portion of the vertebral body was resected, along with the superior and inferior intervertebral discs and the endplate cartilage. Decompression was performed to the medial margin of the contralateral pedicle. Extra care was taken not to injure the spinal cord. Further inspection was conducted to confirm that the compression was completely removed and the deformity was corrected. Next, an autologous tricortical iliac bone graft of an appropriate length was inserted between the superior and inferior vertebral bodies. The titanium plate was mounted and immobilized. The residual fractured blocks were placed into the iliac bone and the lateral gaps. Thorough hemostasis was performed, followed by washing with normal saline. The incision was sutured layer by layer.
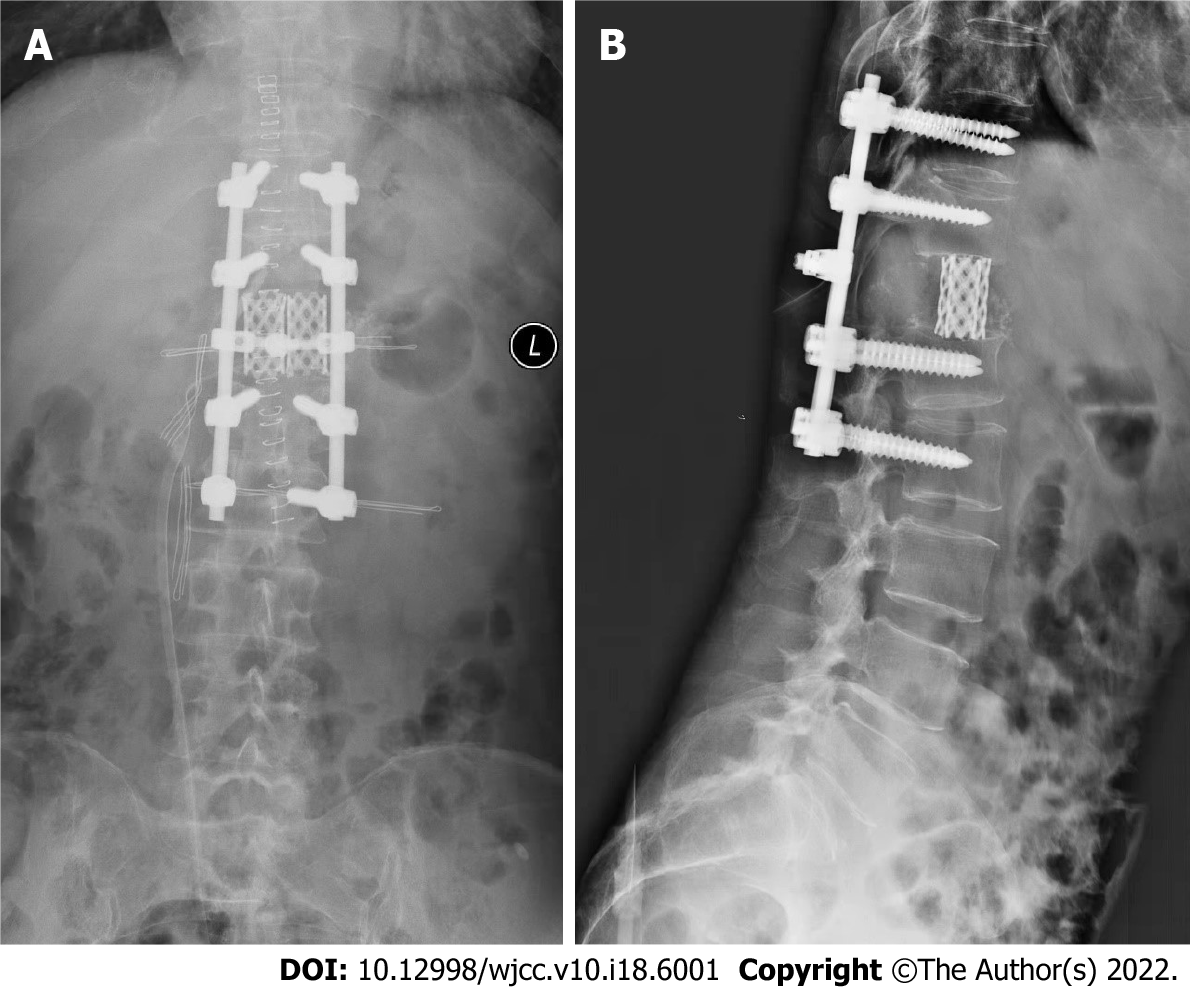
Patients in group 1 received surgery via the combined anterior-posterior approach: The same steps were followed for anterior decompression as in group 2. The incision was maintained at a length of 10-12 cm as no anterior fixation would be performed. Grafting with large iliac bone blocks was performed for the fusion. If the harvested iliac bone blocks were thin, the fusion was performed using a titanium mesh cage. Posterior fixation was performed via the intermuscular space. Therefore, no damage would be caused to the posterior complex structure (Figure 1). The GSS-Ⅱ rod-screw system and Depuy pedicle screw system were used. It was unnecessary to perform canal decompression. Lateral fenestration of the vertebral body was performed if the superior and inferior intervertebral discs of the affected vertebra were not damaged, which was followed by intravertebral bone grafting. A closed thoracic drainage tube was indwelled for all patients receiving thoracotomy. The drainage tube was removed after confirming that there was no effusion or pneumatosis in the thoracic cavity. Costal bone was introduced for patients who received fusion using large iliac bone blocks. The fractured blocks harvested by spinal decompression were regrafted.
The early interventions after surgery were the same in both groups. Patients with nerve injury were treated with hormones and mannitol 4-5 d after surgery and with antibiotics 5-7 d after surgery. Fluid replacement was given to maintain electrolyte and acid-base balance. The indication for blood transfusion was assessed based on intraoperative blood loss and postoperative routine blood tests. Patients with osteoporosis received anti-osteoporosis treatment within 1 mo after surgery, and only then were they allowed to get out of bed. The time to ambulation was prolonged to 1.5 mo after surgery for those with severe osteoporosis. In addition, these patients were required to wear waist braces within the first 3 mo of ambulation.
The observation indicators were blood loss, incision length, operation time, intraoperative X-rays, length of hospital stay, anterior vertebral height ratio, posterior vertebral height ratio, Cobb angle, and canal-occupying ratio of the affected vertebra.
Quality of life (QOL) was scored in the two groups before treatment and at 2 mo after surgery. The total score of each item ranged from 0 to 60: scores < 20, extremely poor; 20-50, fair; and 51-60, good[5].
All statistical analyses were performed using SPSS 22.0 software. Measurements were expressed as mean ± SD and analyzed by the t-test. Counts were expressed as n (%) and analyzed by the χ2 test. P < 0.05 indicated a significant difference.
Blood loss was greater and the operation time was longer in group 1 than in group 2, with significant difference (P < 0.05). Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups (P > 0.05) (Table 2).
| Groups | Blood loss (mL) | Incision length (cm) | Operating time (min) | Intraoperative X-rays | Length of hospital stay (d) |
| Group 1 (n = 60) | 748.28 ± 74.69 | 6.97 ± 0.62 | 145.79 ± 14.63 | 18.77 ± 1.63 | 12.89 ± 1.67 |
| Group 2 (n = 60) | 625.71 ± 62.43 | 7.14 ± 0.75 | 125.28 ± 12.07 | 19.05 ± 1.52 | 12.48 ± 1.43 |
| t value | 9.753 | 1.353 | 8.376 | 0.973 | 1.444 |
| P value | 0.001 | 0.179 | 0.001 | 0.332 | 0.151 |
There were no significant differences in the preoperative function of the affected vertebrae between the two groups (P > 0.05). Significant improvement was achieved in both groups after surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2 (P < 0.05). The canal-occupying ratio of the affected vertebrae was not significantly different between the two groups (P > 0.05) (Table 3).
| Group | Anterior vertebral height ratio of the affected vertebra (%) | Posterior vertebral height ratio of the affected vertebra (%) | Cobb angle (°) | Canal-occupying ratio of the affected vertebra (%) | ||||
| Before | After | Before | After | Before | After | Before | After | |
| Group 1 (n = 60) | 61.86 ± 6.20 | 91.97 ± 7.12 | 89.74 ± 8.51 | 97.52 ± 1.66 | 27.54 ± 2.71 | 5.11 ± 0.53 | 66.12 ± 6.17 | 13.09 ± 1.23 |
| Group 2 (n = 60) | 61.57 ± 6.25 | 89.20 ± 6.16 | 89.43 ± 8.62 | 95.40 ± 2.35 | 27.68 ± 2.62 | 7.09 ± 0.75 | 66.63 ± 6.41 | 12.87 ± 1.45 |
| t value | 0.255 | 2.279 | 0.198 | 5.708 | 0.288 | 16.700 | 0.444 | 0.896 |
| P value | 0.799 | 0.024 | 0.843 | 0.001 | 0.774 | 0.001 | 0.658 | 0.372 |
Before surgery, there was no significant difference in the QOL scores between the two groups (P > 0.05). The above indicators in each group were significantly improved after surgery compared with before surgery. In addition, these indicators were much better in group 1 than in group 2 after surgery (P < 0.05) (Table 4).
| Group | Activities of daily living | Spirit | Sleep | Appetite | ||||
| Before | After | Before | After | Before | After | Before | After | |
| Group 1 (n = 60) | 35.78 ± 5.61 | 51.13 ± 2.04 | 32.91 ± 6.23 | 48.72 ± 5.45 | 36.47 ± 4.52 | 50.87 ± 1.69 | 33.96 ± 5.12 | 52.41 ± 1.37 |
| Group 2 (n = 60) | 36.02 ± 5.77 | 44.81 ± 3.62 | 33.80 ± 6.14 | 42.36 ± 5.22 | 36.68 ± 4.31 | 45.12 ± 2.78 | 34.03 ± 5.08 | 46.89 ± 2.65 |
| t value | 0.200 | 10.203 | 0.683 | 5.653 | 0.226 | 11.856 | 0.065 | 12.413 |
| P value | 0.842 | 0.001 | 0.497 | 0.001 | 0.822 | 0.001 | 0.948 | 0.001 |
Severe spinal fractures caused by high-energy trauma have become increasingly common in recent years. Spinal fractures, damaged spine structure, spinal dislocation, and space occupation by a large number of fractured blocks in the spinal canal may cause spinal cord compression and nerve injury[6,7]. At present, the clinical treatment for such a disorder aims to achieve sufficient spinal decompression, restore the support and immobilize the vertebrae, and hence promote bone union and recovery of nerve function. However, the conventional posterior approach may fail to achieve these goals[8,9].
Surgical treatment for thoracolumbar fractures is usually intended to reconstruct the normal spinal structure and spinal stability, relieve compression, prevent late-stage thoracolumbar deformity and secondary nerve injury, and offer mechanical protection for recovery of nerve function[10,11]. Posterior spinal surgery is an invasive surgery, and the surgical indications of patients should be carefully assessed to prevent complications and ensure surgical success[12,13]. Given these facts, posterior open spinal surgery is generally intended to treat thoracolumbar fractures with spinal instability. Spinal instability is a disorder where the spine does not maintain normal anatomy when resisting loads. As a result, the nerve roots may have a secondary injury or mechanical injury, which further changes the spine structure and induces fracture malunion[14,15]. Certain rules should be followed during surgery, and the surgical approach is selected depending on the position of spinal compression. In addition, a pedicle screw-rod internal fixation system is used to improve surgical outcomes[16,17]. The present study showed that blood loss was greater and the operation time was longer in group 1 than in group 2 (P < 0.05). Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups (P > 0.05). In each group, the patients' condition was significantly improved after surgery compared with before surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2 (P < 0.05). However, the canal-occupying ratio of the affected vertebra was not significantly different between the two groups (P > 0.05). Each group of patients achieved significant improvement after surgery. All of the relevant indicators in group 1 were significantly higher than those in group 2 after surgery (P < 0.05). The reasons for these results might be due to the larger incision, greater blood loss, longer operation time, and difficulty in vertebral exposure. Anterior spinal surgery has the following advantages compared with the posterior approach: More thorough spinal decompression, lower risk of fixation loosening and disruption, removal of the fixation system after artificial joint fusion is unnecessary, and less likelihood of vertebral deformity, paralysis and sequelae after surgery[18,19]. The following defects have been reported for posterior spinal surgery: Degeneration and stenosis of the affected vertebrae and the superior adjacent intervertebral disc; multiple micromovements of the pedicle screws under excessive loading, which further causes loosening before bony fusion[20,21]; postoperative cutting of the screws within the cancellous bone, leading to reduction loss in those for whom osteoporosis is not confirmed before surgery; and fatigue fracture of the pedicle screws and implants due to overload[9]. Despite the above defects, posterior spinal surgery also has the following advantages. It is easier to perform surgery via this approach; only the superior and inferior adjacent segments of the affected vertebrae are immobilized with pedicle screws. In this way, the number of segments to be immobilized is reduced, while the motor function of the spine is preserved maximally[17]. This approach allows for posterior laminectomy with direct decompression. In addition, a well-designed implant enables sufficient stretching of the anterior and posterior longitudinal ligaments of the fibrous ring under the physiological curvature through three-dimensional adjustment. The implant can effectively achieve the reduction of fractured blocks in the vertebral canal in burst fractures through traction. Hence, indirect decompression is achieved without further damaging the stability of the bony structure[16]. The posterior approach not only allows bone grafting for fusion, but also fusion of the anterior affected bone via the pedicle. The combined anterior-posterior surgery integrates the advantages of both the anterior and posterior approaches. The combined approach can directly manage the displacement of a posterior column fracture and offer pre-support to assist in anterior reduction. The adjacent segments can be temporarily stabilized. In addition, the cage for anterior bone fusion can be conveniently placed by pressurizing and tightening. Moreover, excessive tilting or subsidence of the titanium mesh cage can be prevented. Therefore, the normal physiological loading state before the injury can be best reproduced[22]. Our study showed that the combined anterior-posterior surgery outperformed the posterior spinal surgery in promoting the functional recovery of the affected vertebrae and improved the patients’ QOL. The combined approach effectively restored the height of the affected vertebrae and corrected kyphosis. The combined approach also allows for sufficient anterior decompression, and the simple anterior approach does not enable temporary fixation, auxiliary reduction, and three-column fixation according to Denis' three-column concept. Therefore, the latter is usually associated with an unfavorable microenvironment for callus regeneration.
However, our study also has some limitations. First, this was a single-center study with limited number of patients enrolled, and the novel surgical approach is still expected to be attempted in more centers. Second, the follow-up was short in our study, and the long-term efficacy of the novel surgical approach remains to be further documented.
One-stage combined anterior-posterior surgery can effectively improve the function of affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury. This surgical approach is worthy of promotion in clinical use.
Thoracolumbar fractures are usually accompanied by spinal cord injury, and anterior or combined anterior-posterior surgery is preferred for severe thoracolumbar fractures.
We have performed one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury at our center, and the outcomes are expected to be reported.
This study aimed to investigate the effectiveness and postoperative rehabilitation of one-stage combined anterior-posterior surgery for severe thoracolumbar fractures with spinal cord injury.
One hundred and twenty patients with severe thoracolumbar fractures and spinal cord injury treated at our hospital from February 2020 to February 2021 were randomly enrolled, which were randomly divided into group 1 (one-stage combined anterior-posterior surgery) and group 2 (one-stage anterior-approach surgery). Blood loss, incision length, operation time, intraoperative X-rays, length of hospital stay, anterior vertebral height ratio, posterior vertebral height ratio, Cobb angle, canal-occupying ratio of the affected vertebra, and quality of life scores were compared between the two groups.
Blood loss was greater and the operation time was longer in group 1 than in group 2, with significant difference. Incision length, intraoperative X-rays, and length of hospital stay were not significantly different between the two groups. Preoperative function of the affected vertebrae was not significantly different between the two groups. In each group, the patients showed significant improvement after surgery. The anterior vertebral height ratio and the posterior vertebral height ratio in group 1 after surgery were significantly higher than those in group 2. The Cobb angle after surgery was significantly lower in group 1 than in group 2. The canal-occupying ratio of the affected vertebrae was not significantly different between the two groups. Before surgery, there was no significant difference in the quality of life scores between the two groups. The above indicators were significantly improved after surgery compared with before surgery in each group. In addition, these indicators were markedly better in group 1 than in group 2 after surgery.
One-stage combined anterior-posterior surgery effectively improves the function of the affected vertebrae and the life quality of patients with severe thoracolumbar fractures and spinal cord injury.
One-stage combined anterior-posterior surgery is worthy of popularization in clinical use.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Goudeau YR, United States; Middleton AH, United States S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Zhang ZW, Rao XH, Tian JQ. One-stage combined anterior and posterior approach for severe thoracolumbar and lumbar spine fracture. Zhonguo Jizhu Jisui Zazhi. 2010;20:228-234. [DOI] [Full Text] |
| 2. | Fu TY, Liu Y, Zhang W. Comparison of efficacy of the anterior and posterior approaches for surgical treatment of thoracolumbar fractures with spinal cord injury. Zhongguo Zhongyi Gushangke Zazhi. 2020;28:76-79. |
| 3. | Allain J. Anterior spine surgery in recent thoracolumbar fractures: An update. Orthop Traumatol Surg Res. 2011;97:541-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Wang J, Liu P. Analysis of surgical approaches for unstable thoracolumbar burst fracture: minimum of five year follow-up. J Pak Med Assoc. 2015;65:201-205. [PubMed] |
| 5. | Jiang XY, Zhang ZB. Analysis of the short-term efficacy of simple short posterior segmental percutaneous pedicle screw fixation for type A1-A3 thoracolumbar fractures. Shiyong Linchuang Yixue. 2021;18:139-142. |
| 6. | Jiang P, Li NH, Wei C. Observational study on the treatment of ankylosing spondylitis with thoracolumbar fracture with posterior long segmental percutaneous fixation. Zhonguo Jizhu Jisui Zazhi. 2019;29:303-309. |
| 7. | He RK, Cao Y. Research progress in the surgical treatment of thoracolumbar fractures via the posterior approach. Guoji Gukexue Zazhi. 2020;41:100-103. |
| 8. | Liu FQ, Zhang SM. An observation of the clinical effect of posterior single segmental pedicle screw internal fixation in the affected vertebra to treat thoracolumbar fractures. Zhonghua Yixue Zazhi. 2020;55:753-756. |
| 9. | Ko S, Choi W, Lee J, Song S, Nam J. Relationship between the time from injury to surgery and the degree of fracture reduction by ligamentotaxis in a posterior instrumentation without fusion for thoracolumbar unstable burst fracture: a retrospective cohort study. Curr Orthop Pract. 2021;32:124-129. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Kapoen C, Liu Y, Bloemers FW, Deunk J. Pedicle screw fixation of thoracolumbar fractures: conventional short segment versus short segment with intermediate screws at the fracture level-a systematic review and meta-analysis. Eur Spine J. 2020;29:2491-2504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 11. | Wang W, Duan K, Ma M, Jiang Y, Liu T, Liu J, Hao D. Tranexamic Acid Decreases Visible and Hidden Blood Loss Without Affecting Prethrombotic State Molecular Markers in Transforaminal Thoracic Interbody Fusion for Treatment of Thoracolumbar Fracture-Dislocation. Spine (Phila Pa 1976). 2018;43:E734-E739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Gumussuyu G, Islam NC, Kose O, Gungor M, Ozcan H. Comparison of Two Segment Combined Instrumentation and Fusion versus Three Segment Posterior Instrumentation in Thoracolumbar Burst Fractures: A Randomized Clinical Trial with 10 Years of Follow Up. Turk Neurosurg. 2019;29:555-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Spiegl UJ, Devitt BM, Kasivskiy I, Jarvers JS, Josten C, Heyde CE, Fakler HM. Comparison of combined posterior and anterior spondylodesis versus hybrid stabilization in unstable burst fractures at the thoracolumbar spine in patients between 60 and 70 years of age. Arch Orthop Trauma Surg. 2018;138:1407-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Yang M, Zhao Q, Hao D, Chang Z, Liu S, Yin X. Comparison of clinical results between novel percutaneous pedicle screw and traditional open pedicle screw fixation for thoracolumbar fractures without neurological deficit. Int Orthop. 2019;43:1749-1754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Harding AT, Weeks BK, Lambert C, Watson SL, Weis LJ, Beck BR. Exploring thoracic kyphosis and incident fracture from vertebral morphology with high-intensity exercise in middle-aged and older men with osteopenia and osteoporosis: a secondary analysis of the LIFTMOR-M trial. Osteoporos Int. 2021;32:451-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Morrissey PB, Shafi KA, Wagner SC, Butler JS, Kaye ID, Sebastian AS, Schroeder GD, Kepler CK, Aarabi B, Oner FC, Vaccaro AR. Surgical Management of Thoracolumbar Burst Fractures: Surgical Decision-making Using the AOSpine Thoracolumbar Injury Classification Score and Thoracolumbar Injury Classification and Severity Score. Clin Spine Surg. 2021;34:4-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Piccone L, Cipolloni V, Nasto LA, Pripp C, Tamburrelli FC, Maccauro G, Pola E. Thoracolumbar burst fractures associated with incomplete neurological deficit in patients under the age of 40: Is the posterior approach enough? Injury. 2020;51:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Park SJ, Lee CS, Park JS, Lee KJ. Should Thoracolumbar Junction Be Always Avoided as Upper Instrumented Vertebra in Long Instrumented Fusion for Adult Spinal Deformity? Spine (Phila Pa 1976). 2020;45:686-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 19. | Li T, Zheng YH, Xu ZW, Hao DJ, Qian LX. Outcomes of Thoracolumbar Burst Fracture in Patients With Osteoporosis Without Neurologic Symptoms: Analysis of Three Different Surgical Approaches. J Biomater Tissue Eng. 2019;9:1052-1057. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Jang HD, Bang C, Lee JC, Soh JW, Choi SW, Cho HK, Shin BJ. Risk factor analysis for predicting vertebral body re-collapse after posterior instrumented fusion in thoracolumbar burst fracture. Spine J. 2018;18:285-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 21. | Wang W, Pei B, Pei Y, Shi Z, Kong C, Wu X, Wu N, Fan Y, Lu S. Biomechanical effects of posterior pedicle fixation techniques on the adjacent segment for the treatment of thoracolumbar burst fractures: a biomechanical analysis. Comput Methods Biomech Biomed Engin. 2019;22:1083-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 22. | He D, Wu L, Chi Y, Zhong S. Facet joint plus interspinous process graft fusion to prevent postoperative late correction loss in thoracolumbar fractures with disc damage: finite element analysis and small clinical trials. Clin Biomech (Bristol, Avon). 2011;26:229-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |