Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5805
Peer-review started: November 24, 2021
First decision: December 27, 2021
Revised: December 31, 2021
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: June 16, 2022
Processing time: 196 Days and 22.8 Hours
Heterotopic ossification (HO) is a rare clinical phenomenon that refers to bone formation in nonossifying tissues.
This report presents two cases of HO beneath the upper abdominal median incision after radical gastrectomy. The first patient had postoperative pain below the incision area. There were no signs of anastomotic leakage, and the wound healed. Computed tomography (CT) findings 2 wk postoperatively were negative for HO, but the 6-wk CT showed HO beneath the incision. The patient refused reoperation, and after conservative therapy, the pain was gradually relieved after 2 wk. In the second case, postoperative recovery was uneventful, and HO was only detected on routine follow-up CT after 4 mo. An anti-adhesion membrane was applied beneath the peritoneum in both patients. Our findings suggest that HO beneath the abdominal incision might form at approximately 1 mo postoperatively. It may cause intractable pain; however, reoperation is usually not required.
In our cases, we suspect that HO may be related to the use of foreign materials beneath the peritoneum, which needs to be further investigated.
Core Tip: Heterotopic ossification (HO) beneath the upper abdominal incision is a rare clinical phenomenon that refers to bone formation in nonossifying tissues. In our cases, we suspect that HO may be related to the use of foreign materials beneath the peritoneum, which needs to be further investigated.
- Citation: Zhang X, Xia PT, Ma YC, Dai Y, Wang YL. Heterotopic ossification beneath the upper abdominal incision after radical gastrectomy: Two case reports. World J Clin Cases 2022; 10(17): 5805-5809
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5805.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5805
Heterotopic ossification (HO) is a rare clinical phenomenon that refers to bone formation in nonossifying tissues. This is a unique phenomenon that has rarely been reported following abdominal surgery. HO of an incisional scar was first described by Askanazy in 1901 as a subset of myositis ossificans traumatica[1,2]. Since then, more than 100 cases have been reported worldwide[2-6]. These numbers are probably an underestimate of the actual incidence, because these ossifications are usually asymptomatic[3]. HO has been described as a benign postoperative complication in most studies.
Case 1: The first patient was a 62-year-old man, he underwent radical gastrectomy (Billroth I anastomosis) with a midline abdominal incision. Postoperatively, the patient experienced pain below the incisional area.
Case 2: A 57-year-old man also underwent distal gastroscopy (Billroth I anastomosis) due to gastric cancer with a midline abdominal incision. The patient had no other comorbidities.
The two patients underwent distal gastroscopy (Billroth I anastomosis) because of gastric cancer.
Case 1: The patient had a history of coronary stent implantation performed 3 mo ago.
Case 2: The patients had no significant past illness.
The patients had no significant personal and family history.
Case 1: There were no signs of anastomotic leakage, and the wound healed.
Case 2: Upon palpation, the incisional area was hard and firm.
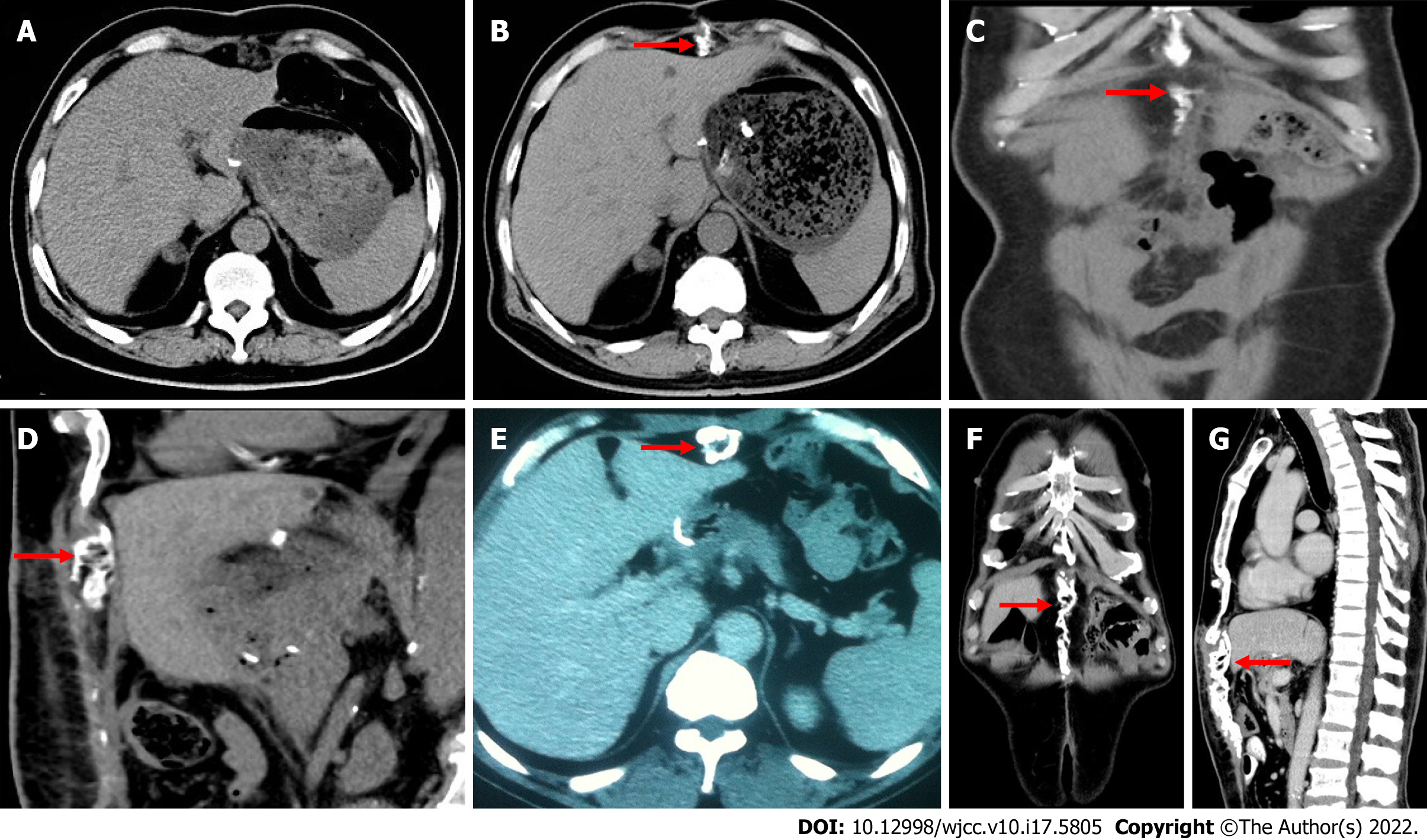
Case 1: Computed tomography (CT) 2 wk postoperatively showed no obvious abnormality (Figure 1A), but the 6-wk CT showed calcification beneath the incision (Figure 1B-D).
Case 2: In the 4-mo follow-up CT scan, calcified tissue was noted under the upper abdominal incision, extending from the immediate subxiphoid region to the umbilical region (Figure 1E-G).
The patients were diagnosed with ossification beneath the upper abdominal incision.
The patient of case 1 refused reoperation, and after conservative therapy (non-steroidal anti-inflammatory drugs), the pain was gradually relieved after 2 wk.
At a 1-year follow-up, the patients of case 1 had no signs of recurrence.
The following common features of ectopic ossification have been summarized in documented cases: (1) Male patients are more susceptible to ectopic ossification, and the male-to-female ratio is as high as 10:1[7]; (2) this pathology has mostly been reported in vertical scars; (3) the ectopic bone is generally formulated within the first year postoperatively; and (4) all cases in the literature occurred during primary healing, and neither wound complications nor changes in serum ion levels were noted. Both our cases fit all of these features. Moreover, the newly formed bone was detected in the first case 6 wk postoperatively, which is sooner than the earliest ectopic abdominal incision ossifications reported in the literature (2 mo)[1]. Our findings suggest that HO beneath the abdominal incision might form at approximately 1 mo postoperatively.
While no certain theory has yet been confirmed regarding etiology, several mechanisms have been studied to help explain this pathological process. Injury or, more specifically, surgical incision is considered a necessary trigger[4]. Three requisite components are involved in the pathogenesis[7]: (1) Inductive signaling pathways are activated by a stimulation factor released from the site of injury. These factors, including bone morphogenic proteins, have been implicated as potential signaling vehicles[8]; (2) then, inducible mesenchymal stem cells, which are located at the injury site, differentiate into osteoblasts or chondroblasts after receiving these signals. This process has been described as osteogenic induction[1,4]; and (3) a heterotopic environment conducive to osteogenesis must exist. HO of the abdominal wall is a subtype of myositis ossificans traumatica. Pieces of the periosteum or perichondrium of the xiphisternum or symphysis pubis may “plant” into the incision wound during the operation and then grow into bone in the scar[1,4]. During laparotomy, we extended the incision to the xiphisternum in both cases, which can be regarded as proof of this theory to some extent.
Tam et al[9] recently reported a case of HO in a patient after hernia repair. In the ectopically formed bone, they found an acellular dermal matrix that had been placed in the primary incision. In our case, we placed a sodium hyaluronate-based bioresorbable membrane (Seprafilm) under the peritoneum of each patient to prevent adhesion. It has been postulated that this type of anti-adhesion agent can cause inflammatory reactions as a severe postoperative complication[10-12]. Whether Seprafilm was the culprit in our case needs to be further investigated.
The main symptoms of HO include local pain and swelling[7]. In suspicious cases, CT or magnetic resonance imaging should be performed for diagnosis[2]. It is also important to exclude other postoperative complications, such as anastomotic leakage and tumor recurrence. In patients with intractable abdominal pain, conservative therapy, such as analgesic administration, parenteral transfusion, and physical therapy, should be initially performed. If conservative therapy fails, then complete excision of the lesion should be considered. Asymptomatic patients need no treatment apart from observation. The first patient in our experience had sustained abdominal pain postoperatively and was readmitted to the hospital twice. After 1 mo of conservative therapy, pain was immediately relieved before surgery was considered.
Non-steroidal anti-inflammatory drug therapy, radiotherapy, and diphosphate (ethindronate disodium) administration have been proposed to decrease heterotopic bone formation[1]. However, the routine application of these methods is controversial and unnecessary.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oley MH, Indonesia; Sharfman Z, Israel S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Reardon MJ, Tillou A, Mody DR, Reardon PR. Heterotopic calcification in abdominal wounds. Am J Surg. 1997;173:145-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Jacobs JE, Birnbaum BA, Siegelman ES. Heterotopic ossification of midline abdominal incisions: CT and MR imaging findings. AJR Am J Roentgenol. 1996;166:579-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Fennema EM, de Boer J, Mastboom WJ. Ossification of abdominal scar tissue: a case series with a translational review on its development. Hernia. 2014;18:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Hogan NM, Caffrey E, Curran S, Sheehan M, Joyce MR. Heterotopic ossification of the abdominal wall. Int J Surg Case Rep. 2012;3:489-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Ma JP, Xian MF, Liao B, Hong GX, He YL, Zhan WH. Postoperative heterotopic mesenteric and incision ossification. Chin Med J (Engl). 2013;126:3799-3780. [PubMed] |
| 6. | Lai HJ, Jao SW, Lee TY, Ou JJ, Kang JC. Heterotopic mesenteric ossification after total colectomy for bleeding diverticulosis of the colon--a rare case report. J Formos Med Assoc. 2007;106:S32-S36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Kaplan FS, Glaser DL, Hebela N, Shore EM. Heterotopic ossification. J Am Acad Orthop Surg. 2004;12:116-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 254] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 8. | McCarthy EF, Sundaram M. Heterotopic ossification: a review. Skeletal Radiol. 2005;34:609-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 251] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Tam V, Zelken J, Sacks JM. Total heterotopic ossification of an acellular dermal matrix used for abdominal wall reconstruction. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Klingler PJ, Floch NR, Seelig MH, Branton SA, Wolfe JT, Metzger PP. Seprafilm-induced peritoneal inflammation: a previously unknown complication. Report of a case. Dis Colon Rectum. 1999;42:1639-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Remzi FH, Oncel M, Church JM, Senagore AJ, Delaney CP, Fazio VW. An unusual complication after hyaluronate-based bioresorbable membrane (Seprafilm) application. Am Surg. 2003;69:356-357. [PubMed] |
| 12. | Huang JC, Yeh CC, Hsieh CH. Laparoscopic management for Seprafilm-induced sterile peritonitis with paralytic ileus: report of 2 cases. J Minim Invasive Gynecol. 2012;19:663-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |