Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5783
Peer-review started: November 13, 2021
First decision: December 10, 2021
Revised: December 18, 2021
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Processing time: 207 Days and 21.4 Hours
Adrenal tuberculosis usually presents with bilateral involvement. It has special characteristics in computed tomography (CT) images, such as small size, low attenuation in the center, and peripheral rim enhancement, which differ from those of primary tumors.
A 42-year-old female presented to the hospital with low back pain. She had been diagnosed with hypertension as well as pulmonary and cerebral tuberculosis but denied having any fever, fatigue, anorexia, night sweats, cough, or weight loss. Abdominal CT revealed an irregular 6.0 cm × 4.5 cm mass with uneven density in the right adrenal gland, while the left adrenal gland was normal. No abnorma
This is a case of unilateral adrenal tuberculosis with CT imaging characteristics mimicking those of a malignant tumor. Extended anti-tuberculosis therapy is recommended in such cases.
Core Tip: In this report, we report a female patient with unilateral adrenal tuberculosis whose CT image characteristics mimic those of a malignant tumor. After a long-term anti-tuberculosis regimen, the large mass in the right adrenal gland was reduced.
- Citation: Liu H, Tang TJ, An ZM, Yu YR. Unilateral adrenal tuberculosis whose computed tomography imaging characteristics mimic a malignant tumor: A case report. World J Clin Cases 2022; 10(17): 5783-5788
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5783.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5783
Tuberculosis (TB) is known to present with varied clinical features, but involvement of the adrenal glands in TB is rare[1]. Isolated adrenal TB accounts for under 2% of adrenal incidentalomas[2], while 75%-100% of patients with adrenal TB have bilateral involvement[3-5]. As a result, unilateral adrenal TB is considered a rare clinical entity. The computed tomography (CT) imaging characteristics of adrenal TB are significantly different from those of primary tumors, such as small size, low attenuation in the center, and peripheral rim enhancement[3,6,7]. Herein, we report an unusual case of unilateral adrenal TB whose imaging characteristics were extremely atypical and suggested a high likelihood of a malignant tumor. Fine-needle aspiration biopsy (FNAB) was used to confirm TB, and prolonged anti-TB treatment was given to stabilize her condition.
A 42-year-old female was admitted to our department after presenting with a half-year history of osphyalgia.
A 42-year-old female had low back pain for a half year, which was exaggerated when taking a deep breath or lying flat and relieved when standing. She denied frequent micturition, painful urination, fever, hematuria, or pyuria.
The patient had a remote history of hypertension. She had been diagnosed with pulmonary and cerebral TB four months before presentation, and she had started a regimen of anti-TB drugs (isoniazid 0.3 g QD, rifampicin 0.45 g QD, ethambutol 0.75 g QD, and ofloxacin 0.5 g QD) upon diagnosis.
Her personal and family history were insignificant.
Physical examination showed nothing special despite percussive pain in the right kidney area.
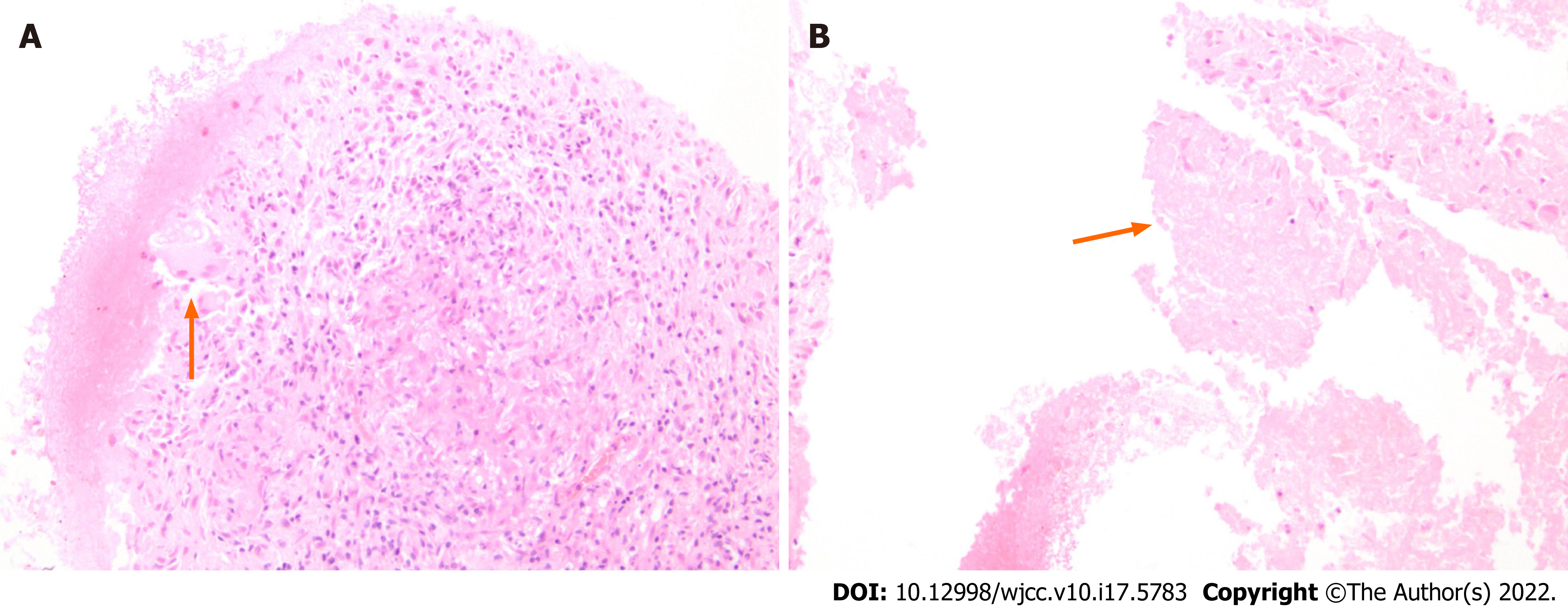
Laboratory tests yielded the following results: plasma total cortisol (8 am), 594.6 nmol/L (reference, 147.3-609.3 nmol/L); adrenocorticotropic hormone, 48.30 ng/L (reference, 5.0-78 ng/L); and aldosterone/renin ratio, 16.92 ng/dL per ng/mL/h. No abnormalities were observed in the blood and urine catecholamines. Routine blood tests, routine urine tests, and biochemical tests were roughly in the normal range. CT-guided Fine needle aspiration biopsy (FNAB) of the right adrenal gland was performed, and pathological examination detected granulomas and necrosis (Figure 1A and B).
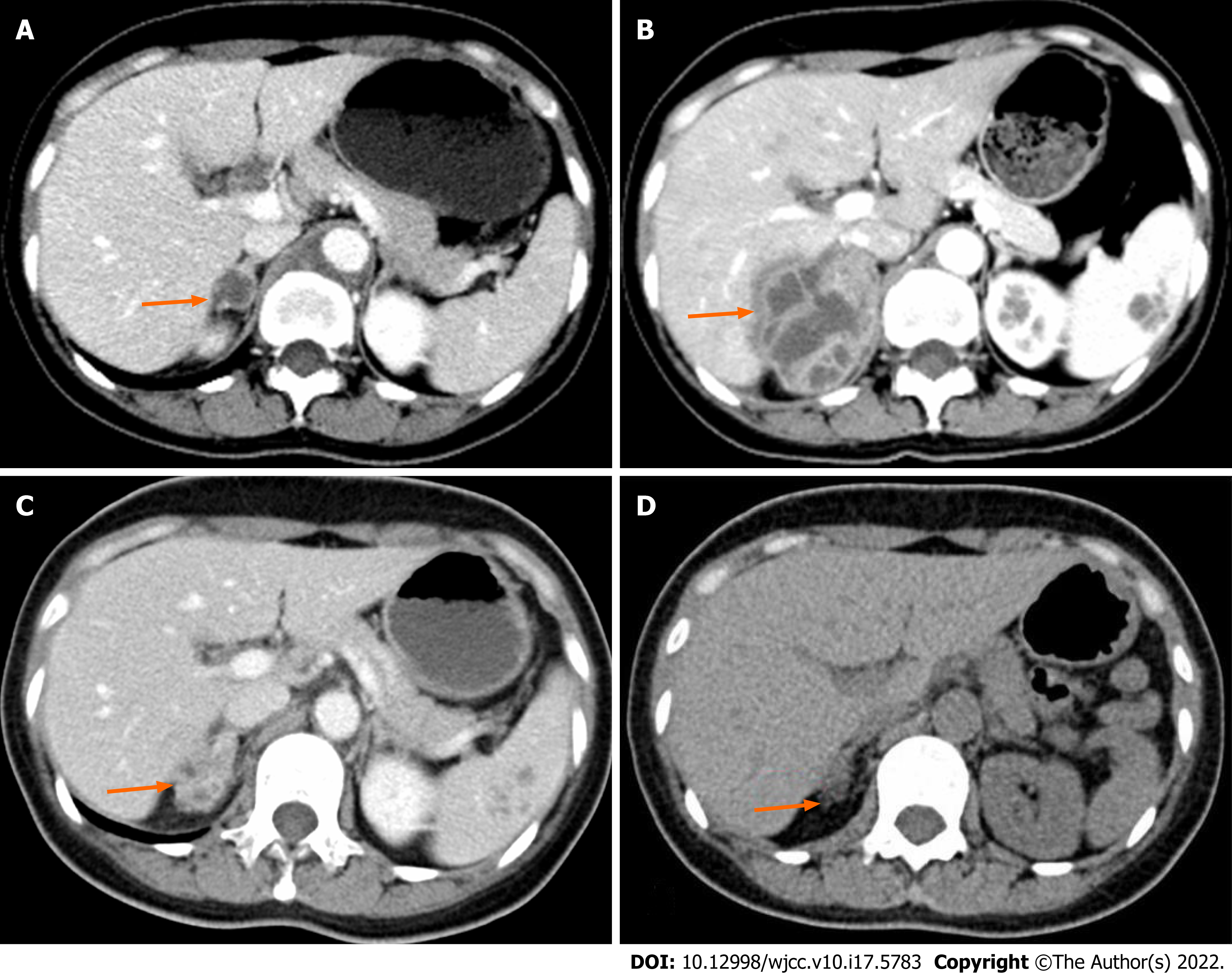
Four months prior to presentation, the patient had undergone an abdominal CT scan, which revealed a 1.5 cm isointense mass in the right adrenal gland (Figure 2A). On presentation to our department, she underwent another abdominal CT scan, which revealed a 6.0 cm × 4.5 cm irregular mass with uneven density in the right adrenal gland, while the left adrenal gland was normal (Figure 2B).
Unilateral adrenal tuberculosis.
Treatment with 4 anti-TB drugs was continued.
The patient’s low back pain was relieved, and abdominal CT (Figure 2C) demonstrated a significant reduction of the mass in the right adrenal gland (2.7 cm × 2.4 cm) after 15 mo of anti-TB therapy. Three years later, abdominal CT (Figure 2D) showed a slight enlargement of the right adrenal gland.
Extrapulmonary TB constitutes about 15%-20% of all TB patients[8]. The most frequent sites of extrapulmonary TB include the lymph nodes (19%), pleural cavity (7%), gastrointestinal tract (4%), bone (6%), central nervous system (3%), and genitourinary system (1%)[9]. Of the 370 reports of extrapulmonary TB in a systematic review spanning 10 years[1], only one case was shown to involve the adrenal gland, which demonstrated adrenal TB as a rare clinical entity. Bilateral involvement usually occurs because of hematogenous and lymph spread from the site of the primary mycobacterial infection to both adrenal glands, which are equally susceptible[10]. In our case, adrenal TB (lesions of 1.5 cm to 5 cm) was aggravated while the anti-TB regimen was continued. It is necessary to distinguish adrenal masses from adrenal tumors. Adrenal incidentalomas, adenomas, metastases, adrenocortical carcinomas, myelolipomas, and pheochromocytomas accounted for 41%, 19%, 10%, 9%, and 8%, respectively. The etiologies of these partly depend on the size, such that larger tumors are more likely to be malignant. Adrenal carcinomas and metastases comprise 25% and 18% of lesions and are larger than 6 cm, while adenomas account for only 18%[11]. For tumors smaller than 4 cm, adrenal carcinomas comprise 2% and adenomas comprise 65%[11]. Untreated TB lesions were smaller than primary tumors (2.8 cm ± 1.3 cm vs 3.5 cm ± 2.4 cm)[6], while the diameters of benign, malignant pheochromocytoma and adrenocortical carcinoma were 5.7 cm ± 2.3 cm, 8.3 cm ± 4.1 cm[12] and 11 cm ± 4 cm[13], respectively. It is difficult to provide evidence with regard to TB based on size (6.0 cm × 4.5 cm) in this case. The CT value, attenuation measurement, and reduced central area (7 ± 4 HU) compared to the peripheral area (32 ± 14 HU) were observed between unenhanced and contrast-enhanced scans in adrenal TB[3]. This characteristic of central necrosis surrounded by fibrous and granulomatous inflammatory tissue is much less common in primary adrenal tumors[6], owing to sufficient blood supply in the central area. Pheochromocytoma always has a high enhancement of > 110 HU in the arterial phase[14], while adrenocortical carcinoma is less likely to show an enhancement of >100 HU. In the present case, evidence from images could not rule out a malignant tumor in the adrenal gland. In addition, calcification preferentially occurred in the later stages of adrenal TB than in adrenal tumors (59% vs 8%), which helped with a proper diagnosis[6].
In addition to the ineffectiveness of FNAB in distinguishing adrenal adenoma from adenocarcinoma[11], it is considered advantageous due to its ease, cost-effectiveness, reduced time consumption, low complication rates, and high accuracy[15-17]. It is often used for suspected nonfunctional and nonneoplastic adrenal gland lesions, but not employed for pheochromocytomas[11,17] due to the risk of hemodynamic instability. In the present case, blood pressure was well controlled and had no abnormalities in blood and urine catecholamines, indicating a lower possibility of pheochromocytoma. Therefore, FNAB was performed to obtain histological evidence, which subsequently provides clear evidence regarding targeted therapy.
Patients with adrenal TB are usually treated with standard quadruple antitubercular treatment (such as isoniazid, rifampicin, pyrazinamide, and ethambutol)[18-20] for nearly 12 mo or longer. Adverse reactions to anti-TB drugs and their interactions with corticosteroids that are administered for replacement therapy remain challenging[21,22]. Firstly, rifampicin increases cortisol catabolism while isoniazid produces increased levels of cortisol via an opposite effect on the enzyme activity 6-Bhydroxylase; secondly, hepatitis, induced by isoniazid and worsened by rifampicin, leads to failure of 11-B-oxo-reductase, which converts cortisone to cortisol; and finally, tuberculous Addison’s disease might require increased amounts of hydrocortisone due to rifampicin administration[23]. Up to 70% of patients with active TB have subclinical adrenal insufficiency[24]. Anti-TB treatment might cause adrenal crisis[18], and patients should be closely monitored when starting this treatment. Most of the cases demonstrated a good response to anti-TB treatment. Early diagnosis and no delay in treatment initiation contributed to minimizing the high mortality rate[22,25]. Addison’s disease usually occurs when more than 90% of adrenal tissue has been destroyed[26]. Only a few patients with tuberculous Addison's disease showed recovery of adrenal function[27].
Unilateral adrenal tuberculous infection, although rare, should be considered in patients with unilateral adrenal mass but without Cushing syndrome, primary aldosteronism, or pheochromocytoma. FNAB assists in diagnosing TB, and early initiation and longer duration of anti-TB therapy are crucial to treating patients with unilateral adrenal tuberculous infection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Endocrinology and metabolism
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Huei TJ, Malaysia; Piltcher-da-Silva R, Brazil S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Edlin GP. Active tuberculosis unrecognised until necropsy. Lancet. 1978;1:650-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Lam KY, Lo CY. A critical examination of adrenal tuberculosis and a 28-year autopsy experience of active tuberculosis. Clin Endocrinol (Oxf). 2001;54:633-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Ma ES, Yang ZG, Li Y, Guo YK, Deng YP, Zhang XC. Tuberculous Addison's disease: morphological and quantitative evaluation with multidetector-row CT. Eur J Radiol. 2007;62:352-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Gupta P, Bhalla A, Sharma R. Bilateral adrenal lesions. J Med Imaging Radiat Oncol. 2012;56:636-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Guo YK, Yang ZG, Li Y, Ma ES, Deng YP, Min PQ, Yin LL, Hu J, Zhang XC, Chen TW. Addison's disease due to adrenal tuberculosis: contrast-enhanced CT features and clinical duration correlation. Eur J Radiol. 2007;62:126-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Yang ZG, Guo YK, Li Y, Min PQ, Yu JQ, Ma ES. Differentiation between tuberculosis and primary tumors in the adrenal gland: evaluation with contrast-enhanced CT. Eur Radiol. 2006;16:2031-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Alshahrani MA, Bin Saeedan M, Alkhunaizan T, Aljohani IM, Azzumeea FM. Bilateral adrenal abnormalities: imaging review of different entities. Abdom Radiol (NY). 2019;44:154-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Sharma SK, Mohan A, Kohli M. Extrapulmonary tuberculosis. Expert Rev Respir Med. 2021;15:931-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 10. | Kissane, John M. Anderson's Pathology. 1985. |
| 11. | Aron D, Terzolo M, Cawood TJ. Adrenal incidentalomas. Best Pract Res Clin Endocrinol Metab. 2012;26:69-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Khadilkar K, Sarathi V, Kasaliwal R, Pandit R, Goroshi M, Malhotra G, Dalvi A, Bakshi G, Bhansali A, Rajput R, Shivane V, Lila A, Bandgar T, Shah NS. Predictors of malignancy in patients with pheochromocytomas/paragangliomas: Asian Indian experience. Endocr Connect. 2016;5:89-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Zhang HM, Perrier ND, Grubbs EG, Sircar K, Ye ZX, Lee JE, Ng CS. CT features and quantification of the characteristics of adrenocortical carcinomas on unenhanced and contrast-enhanced studies. Clin Radiol. 2012;67:38-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Northcutt BG, Raman SP, Long C, Oshmyansky AR, Siegelman SS, Fishman EK, Johnson PT. MDCT of adrenal masses: Can dual-phase enhancement patterns be used to differentiate adenoma and pheochromocytoma? AJR Am J Roentgenol. 2013;201:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Patel S, Jinjuvadia R, Devara A, Naylor PH, Anees M, Jinjuvadia K, Al-Haddad M. Performance characteristics of EUS-FNA biopsy for adrenal lesions: A meta-analysis. Endosc Ultrasound. 2019;8:180-187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Kerimaa P, Marttila A, Hyvönen P, Ojala R, Lappi-Blanco E, Tervonen O, Blanco Sequeiros R. MRI-guided biopsy and fine needle aspiration biopsy (FNAB) in the diagnosis of musculoskeletal lesions. Eur J Radiol. 2013;82:2328-2333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Patil R, Ona MA, Papafragkakis C, Duddempudi S, Anand S, Jamil LH. Endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of adrenal lesions. Ann Gastroenterol. 2016;29:307-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Denny N, Raghunath S, Bhatia P, Abdelaziz M. Rifampicin-induced adrenal crisis in a patient with tuberculosis: a therapeutic challenge. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Shrestha B, Omran A, Rong P, Wang W. Successfully treated unusual case of primary adrenal and spinal tuberculosis with three years follow up. Pan Afr Med J. 2014;17:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Manso MC, Rodeia SC, Rodrigues S, Domingos R. Synchronous presentation of two rare forms of extrapulmonary tuberculosis. BMJ Case Rep. 2016;2016:10.1136/bcr-2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Thijs E, Wierckx K, Vandecasteele S, Van den Bruel A. Adrenal insufficiency, be aware of drug interactions! Endocrinol Diabetes Metab Case Rep. 2019;2019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Shah M, Reed C. Complications of tuberculosis. Curr Opin Infect Dis. 2014;27:403-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 23. | Kusuki K, Watanabe S, Mizuno Y. Tuberculous Addison's disease with increased hydrocortisone requirements due to administration of rifampicin. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Sarin BC, Sibia K, Kukreja S. Study of adrenal function in patients with tuberculosis. Indian J Tuberc. 2018;65:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Zhao N, Gao Y, Ni C, Zhang D, Zhao X, Li Y, Sun B. An autopsy case of unexpected death due to Addison's disease caused by adrenal tuberculosis. Eur J Med Res. 2021;26:137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Alevritis EM, Sarubbi FA, Jordan RM, Peiris AN. Infectious causes of adrenal insufficiency. South Med J. 2003;96:888-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Penrice J, Nussey SS. Recovery of adrenocortical function following treatment of tuberculous Addison's disease. Postgrad Med J. 1992;68:204-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |