Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5741
Peer-review started: October 28, 2021
First decision: December 27, 2021
Revised: January 14, 2022
Accepted: April 4, 2022
Article in press: April 4, 2022
Published online: June 16, 2022
Processing time: 223 Days and 17.4 Hours
Modified radical mastectomy (MRM) is the most common surgical treatment for breast cancer. General anesthesia poses a challenge in fragile MRM patients, including cardiovascular instability, insufficient postoperative pain control, nausea and vomiting. Thoracic paravertebral block (TPVB) is adequate for simple mastectomy, but its combination with interscalene brachial plexus block (IBPB) has not yet been proved to be an effective anesthesia method for MRM.
We describe our experience of anesthesia and pain management in 10 patients with multiple comorbidities. An ultrasound-guided TPVB was placed at T2-T3 and T5-T6, and combined with IBPB, with administration of 10, 15 and 5 mL of 0.5% ropivacaine, respectively. A satisfactory anesthetic effect was proved by the absence of ipsilateral tactile sensation within 30 min. Propofol 3 mg/kg/h and oxygen supplementation via a nasal cannula were administered during surgery. None of the patients required additional narcotics, vasopressors, or conversion to general anesthesia. The maximum pain score was 2 on an 11-point numerical rating scale. Two patients required one dose of celecoxib 8 h postoperatively and none reported nausea or emesis.
This case series demonstrated that combined two-site TPVB and small-volume IBPB with sedation can be used as an alternative anesthetic modality for MRM, providing good postoperative analgesia.
Core Tip: Thoracic paravertebral block (TPVB) has been proved to be adequate for simple mastectomy. However, TPVB combined with interscalene brachial plexus block (IBPB) has not yet been proved to be an effective anesthesia method for modified radical mastectomy (MRM). This case series demonstrated that combined two-site TPVB and small-volume IBPB with sedation can be used as an alternative anesthetic modality for MRM, which avoids the potential risks of general anesthesia and phrenic nerve paralysis especially in frail patients with multiple comorbidities, and provides extended postoperative analgesia.
- Citation: Hu ZT, Sun G, Wang ST, Li K. Combined thoracic paravertebral block and interscalene brachial plexus block for modified radical mastectomy: A case report. World J Clin Cases 2022; 10(17): 5741-5747
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5741.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5741
The National Breast Cancer Foundation has confirmed that breast cancer is the second most common cancer in women, with 3.8 million women diagnosed in the United States as of January 1, 2019[1]. Modified radical mastectomy (MRM) is the most common surgical treatment for breast cancer[2]. Modified radical mastectomy is frequently performed under general anesthesia. However, general anesthesia may pose challenges especially in elderly and frail patients with comorbidities. Furthermore, some components of general anesthesia are associated with chronic pain, vomiting and impaired respiratory function[3,4]. On the other hand, regional anesthesia is commonly believed to decrease cardiovascular, respiratory and gastrointestinal adverse events in high-risk patients[5,6], and attenuate immune suppression[7]. Accordingly, there is growing interest in loco-regional anesthesia as an alternative to general anesthesia for MRM.
Thoracic epidural anesthesia combined with interscalene brachial plexus block (IBPB) has been reported to be an adequate anesthesia technique for MRM[8]. Thoracic paravertebral block (TPVB) is efficacious for simple mastectomy surgery[9], but the efficacy of TPVB combined with IBPB has not yet been studied for MRM.
In this case series, we describe our experience of intraoperative anesthesia and postoperative pain management in ten elderly and fragile MRM patients who underwent ultrasound-guided two-site TPVB and small-volume IBPB combined with sedation.
Ten patients scheduled for elective MRM were anesthetized by the same expert in ultrasound-guided loco-regional anesthesia in our facility between January 2019 and March 2019.
All patients were identified as suitable candidates for loco-regional anesthesia using current anticoagulation recommendations.
Patient characteristics are shown in Table 1.
| Case | Sex | Age | BMI, kg/m2 | Comorbidities | Surgical procedure | Oncology state |
| Patient 1 | Female | 65 | 21.1 | HT, COPD | M + LND | T1N1M0 |
| Patient 2 | Female | 72 | 21.4 | HT | M + SNB | T2N1M0 |
| Patient 3 | Female | 65 | 24.4 | HT, COPD | M + LND | T2N3M0 |
| Patient 4 | Female | 78 | 24.2 | DM, AS | M | - |
| Patient 5 | Female | 73 | 20.2 | HT, DM, CI | M + LND | T2N1M0 |
| Patient 6 | Female | 73 | 30.4 | HT, DM, MI | M | - |
| Patient 7 | Female | 65 | 24.2 | HT, AS, MI | M | - |
| Patient 8 | Female | 68 | 21.9 | HT, MI | M + SNB | T1N0M0 |
| Patient 9 | Female | 65 | 33.6 | HT, DM | M + SNB | T2N0M0 |
| Patient 10 | Female | 79 | 24.5 | DM, MI, CI | M + SNB | T1N1M0 |
All of the ten cases were diagnosed as breast neoplasm by preoperative imaging examinations either by unltrasoud or computerized tomography, suspected to be malignant.
All patients were identified as suitable candidates for loco-regional anesthesia using current anticoagulation recommendations.
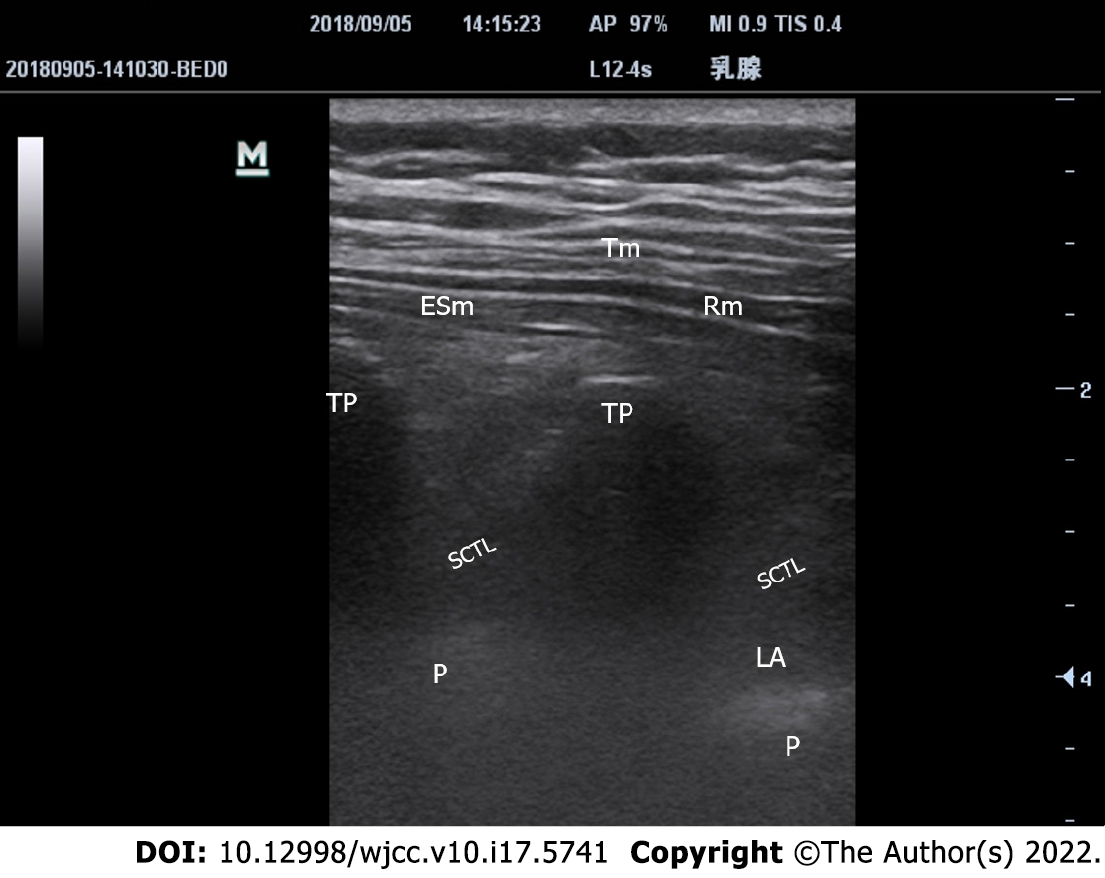
On arrival in the preoperative area, standard monitoring was conducted and the patients were placed in the lateral decubitus position and received intravenous sedation with midazolam. TPVB was then initiated. A 10 MHz linear array transducer was vertically placed in the sagittal, paramedian plane, approximately 2-2.5 cm lateral to the spinous process at the predetermined level, and the following structures were identified: transverse process, parietal pleura, superior costotransverse ligament and the desired paravertebral space. Following infiltration of the skin with 2% lidocaine, a 22-G × 50-mm needle was advanced using the out-of-plane technique. Eventually, a “pop” was felt as the needle tip penetrated the anterior border of the superior costotransverse ligament. Hydro dissection with normal saline was used to confirm correct placement of the needle tip by anterior displacement of the parietal pleura (Figure 1). Ten and 15 mL of 0.5% ropivacaine were injected at two thoracic (T) levels: T2-T3 and T5-T6, respectively[10,11]. TPVB was supplemented with ipsilateral IBPB using the in-plane technique at C6 Level with an injection of 5 mL ropivacaine (0.5%). Sensory blockade was assessed by pin prick testing using a 22-G short bevel needle. A satisfactory anesthetic effect was defined as the absence of ipsilateral tactile sensation covering the region between the clavicle and T7 dermatome, and from the ipsilateral parasternal area to the axilla within 30 min after local anesthetic administration. The time required to perform the blocks ranged from 5 to 10 min.
Patients were sedated with a continuous infusion of propofol 3 mg/kg/h, and oxygen supplementation via a nasal cannula during surgery. A bolus of 1 μg/kg fentanyl was available for intraoperative breakthrough pain. Conversion to general anesthesia was considered if required. The patients were offered 200 mg celecoxib orally as needed for moderate postoperative pain, and an intravenous bolus of 3 mg morphine for severe pain.
The average duration of surgery was 115 (± 21.7) min. None of the patients required intraoperative narcotics, or conversion to general anesthesia. The patients were hemodynamically stable and did not require vasopressors. No complications due to local anesthesia, such as allergic reaction, paresthesia, vascular injury and toxicity were observed. All patients were transferred to a regular nursing ward shortly after surgery.
Postoperative pain was well controlled. Eight patients reported a maximum pain score of 2 out of 10 points and did not require additional analgesics during a 12-h-interval follow-up in the first three postoperative days. Two patients needed one dose of celecoxib 8 h after surgery. None of the patients required morphine. All patients were satisfied with their anesthesia and pain management. All patients resumed normal food intake within 4 h and were able to use the surgical-side hand within 24 h. The recovery period was uneventful, with no reports of postoperative nausea and vomiting (PONV). Timeline of all cases are shown in Table 2.
| Case series | Ten elderly and fragile patients with multiple comorbidities scheduled for modified radical mastectomy |
| Interventions | Standard monitoring and sedation with midazolam in lateral decubitus position before regional anesthesia. 10 and 15 mL of 0.5% ropivacaine injected at T2-T3 and T5-T6 as thoracic paravertebral block by ultrasound-guided using the out-of-plane technique.5 mL of 0.5% ropivacaine injected as interscalene brachial plexus block using the in-plane technique |
| Results | Sensory blockade assessed by pin prick testing, covering the region between the clavicle and T7 dermatome, and from the ipsilateral parasternal area to the axilla. Only sedated with propofol and oxygen supplementation via a nasal cannula during surgery. Vasopressors, narcotics or general anesthesia was not applied but considered if required for surgery |
| Follow-up | Postoperative pain was well controlled as a 2 out of 10 points pain score without celecoxib or morphine. Normal food intake was resumed within 4 h and surgical-side hand were able to use within 24 h. Recovery period was uneventful, without complications or postoperative nausea and vomiting |
To the best of our knowledge, compared to single cases using TPVB for awake mastectomy[9], there are no previous reports on the combination of two-sites TPVB with IBPB as the sole anesthetic technique for MRM. In our 10 elderly patients with multiple comorbidities, this technique provided potent alternative anesthesia with extended postoperative analgesia, and avoided the use of opioids, vasopressors, neuromuscular blocking agents and mechanical ventilation. In addition, PONV, cardiovascular and pulmonary complications were not observed. A similar observation was confirmed by a single case report[12]. Also, thoracic epidural anesthesia combined with IBPB[8] provided similar anesthesia and analgesia compared to ultrasound-guided TPVB; however, the latter is a safer option. Although our technique requires expertise in ultrasound-guided loco-regional blocks and might not replace general anesthesia as routine for MRM, it remains a reliable alternative when general anesthesia is deemed undesirable or poses unacceptable risks.
With the assistance of real-time ultrasound, many high-risk regional blocks, such as TPVB, have become more popular and are safer. TPVB involves the injection of local anesthetics in the vicinity of spinal nerves emerging from the intervertebral foramina resulting in ipsilateral somatic and sympathetic nerve blockade in multiple contiguous dermatomes above and below the site of injection[13]. Although four or five site blocks provide reliable analgesia[14], this is not practical for MRM. One study showed that contrast dye spread to 4.5 dermatome segments vertically after a single paravertebral injection compared to 6 segments after double-level injections[13]. An improved analgesic effect was demonstrated with double-level TPVB compared to single-level[11]. Based on these previous reports, we decided to use two-level TPVB. Effective anesthesia of the axilla and pectoral major muscle are essential for MRM, and is not achieved by TPVB alone. This area is innervated by the lateral and medial pectoral nerves, long thoracic nerve and thoracodorsal nerve, all originating from the brachial plexus[15]. Accordingly, IBPB is an essential complement for TPVB in MRM.
Vigilance and continuous monitoring are mandatory, regarding potential complications such as inadvertent vascular puncture, epidural or intrathecal spread, pneumothorax, serious bradycardia, contralateral Harlequin syndrome and Horner’s syndrome[16]. Even though there is less possibility of spreading to the intervertebral foramen and phrenic nerve and extensive intramuscular deposition with 5 mL IBPB than with 20 mL[17], it is also much better to administer nasal oxygen for 12 h. Despite the aforementioned potential complications, regional anesthesia and analgesia enhance postoperative oral intake, ambulation and rehabilitation[5], and potentially increase patient tolerance to early chemotherapy as compared with general anesthesia.
Other superficial facial blocks have been reported in case reports of MRM despite the uncertainty of local anesthetic diffusion and patchy coverage. In order to ensure the anesthesia effect, serratus anterior plane block was often combined with remifentanil infusion and 3 supplementary subcutaneous infiltrations of the intercostobrachial nerve, medial branches of the intercostal nerve and superficial cervical plexus[18], or 30 mg ketamine[19]. It was confirmed that the erector spinae plane at T4 was feasible for MRM, however fentanyl supplementation was required in all cases[20]. The Pecs II nerve block with high volume and perfect diffusion may be an alternative to the combination of two-site TPVB and small-volume IBPB for further avoidance of respiratory depression[21]. Pecs II nerve block is aimed to block at least the pectoral nerves, the intercostobrachial, intercostals III-IV-V-VI and the long thoracic nerve. These nerves need to be blocked to provide complete analgesia during breast surgery, and it is an alternative or a rescue block if paravertebral blocks and thoracic epidurals failed, with the indications such as tumorectomies, extensive excisions, and axillary clearances.
The reliable impeccable anesthesia effect and simple and convenient operation associated with ultrasound-guided two-spot TPVB combined with small-volume IBPB has been highlighted and initially proved by the present ten cases. Regarding the thoracic dermatotome and breast MRM, ultrasound-guided TPVB provide thorough anesthetic effect similar to thoracic epidural anesthesia, with better visualization and higher successful rate. Two-sites TPVB guarantee more extensive anesthesia scope than single-site, especially for intercostobrachial nerve, avoiding neither tedious process nor puncture-related pain required by 3-5 sites injection. Because axillary dermatotome, pectoral major and minor muscles are dominated by nerve roots of bronchial plexus, IBPB is more straightforward, impeccable and efficient than terminal branch block and superficial plane block, such as serratus anterior plane block, Pecs II nerve block, medial bronchial cutaneous nerve block, which facilitate puncture operation and local anesthetics dosing. The fearful anxiety of phrenic nerve paralysis associated with IBPB, is also evitable when using 5 mL rather than routine volume of 20 mL, with equivalent effect. With the better visualization and higher successful rate provided by ultrasound-guided intervention technique, the method might be also feasible in the morbid obesity population.
Our observation was performed in a single site and restricted to 10 Chinese patients. Both efficacy and safety outcomes were highly related with anesthetist’s manipulation capability of ultrasound-guided regional anesthesia. Further multi-center randomized control trial with enough sample size is needed to finally determine the feasibility, efficiency and safety of the novel combinations. For further improvement, subcutaneous infiltration of the supraclavicular nerve might be supplemented for the dermatomal area around the clavicle, pectoralis major, and deltoid[12]. Further decrease of either concentration or volume of ropivacaine is worth of investigation with regard to the equivalent and safe alternative approach. Diaphragmatic activity monitoring by ultrasound, or pulmonary function test should be performed during perioperative period to provide authentic proof in terms of pulmonary function.
Two-spot TPVB combined with small-volume IBPB is considered a reliable and safe alternative anesthetic technique for MRM, which avoids the potential risks of general anesthesia especially in frail patients with multiple comorbidities, and provides extended postoperative analgesia.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Amornyotin S, Thailand; Spataru A, Canada S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, Siegel RL. Breast cancer statistics, 2019. CA Cancer J Clin. 2019;69:438-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1500] [Cited by in RCA: 2027] [Article Influence: 337.8] [Reference Citation Analysis (0)] |
| 2. | Jones C, Lancaster R. Evolution of Operative Technique for Mastectomy. Surg Clin North Am. 2018;98:835-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Shirakami G, Teratani Y, Segawa H, Matsuura S, Shichino T, Fukuda K. Omission of fentanyl during sevoflurane anesthesia decreases the incidences of postoperative nausea and vomiting and accelerates postanesthesia recovery in major breast cancer surgery. J Anesth. 2006;20:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Sessler DI, Pei L, Huang Y, Fleischmann E, Marhofer P, Kurz A, Mayers DB, Meyer-Treschan TA, Grady M, Tan EY, Ayad S, Mascha EJ, Buggy DJ; Breast Cancer Recurrence Collaboration. Recurrence of breast cancer after regional or general anaesthesia: a randomised controlled trial. Lancet. 2019;394:1807-1815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 257] [Article Influence: 42.8] [Reference Citation Analysis (0)] |
| 5. | Malik OS, Brovman EY, Urman RD. The Use of Regional or Local Anesthesia for Carotid Endarterectomies May Reduce Blood Loss and Pulmonary Complications. J Cardiothorac Vasc Anesth. 2019;33:935-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 6. | Ahn EJ, Kim HJ, Kim KW, Choi HR, Kang H, Bang SR. Comparison of general anaesthesia and regional anaesthesia in terms of mortality and complications in elderly patients with hip fracture: a nationwide population-based study. BMJ Open. 2019;9:e029245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 74] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 7. | Wall T, Sherwin A, Ma D, Buggy DJ. Influence of perioperative anaesthetic and analgesic interventions on oncological outcomes: a narrative review. Br J Anaesth. 2019;123:135-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 146] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 8. | Sundarathiti P, Pasutharnchat K, Kongdan Y, Suranutkarin PE. Thoracic epidural anesthesia (TEA) with 0.2% ropivacaine in combination with ipsilateral brachial plexus block (BPB) for modified radical mastectomy (MRM). J Med Assoc Thai. 2005;88:513-520. [PubMed] |
| 9. | Santonastaso DP, de Chiara A, Piccioni F, Tognù A, Agnoletti V. Awake mastectomy under ultrasound guided thoracic paravertebral block in elderly patients. J Clin Anesth. 2018;47:50-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Abdallah FW, Morgan PJ, Cil T, McNaught A, Escallon JM, Semple JL, Wu W, Chan VW. Ultrasound-guided multilevel paravertebral blocks and total intravenous anesthesia improve the quality of recovery after ambulatory breast tumor resection. Anesthesiology. 2014;120:703-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 112] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 11. | Kasimahanti R, Arora S, Bhatia N, Singh G. Ultrasound-guided single- vs double-level thoracic paravertebral block for postoperative analgesia in total mastectomy with axillary clearance. J Clin Anesth. 2016;33:414-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Nirmal CP, Gowrishankar C. Thoracic Paravertebral Block and Interscalene Brachial Plexus Block Superficial Cervical Plexus Block for Breast Surgery in A Patient with Ischemic Heart Disease. BLOOD PRESSURE. 2019;130:80. |
| 13. | Hara K, Sakura S, Nomura T, Saito Y. Ultrasound guided thoracic paravertebral block in breast surgery. Anaesthesia. 2009;64:223-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 14. | Naja ZM, El-Rajab M, Al-Tannir MA, Ziade FM, Tayara K, Younes F, Lönnqvist PA. Thoracic paravertebral block: influence of the number of injections. Reg Anesth Pain Med. 2006;31:196-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Kaya M, Oğuz G, Şenel G, Kadıoğulları N. Postoperative analgesia after modified radical mastectomy: the efficacy of interscalene brachial plexus block. J Anesth. 2013;27:862-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Batra RK, Krishnan K, Agarwal A. Paravertebral block. J Anaesthesiol Clin Pharmacol. 2011;27:5-11. [PubMed] |
| 17. | Stundner O, Meissnitzer M, Brummett CM, Moser S, Forstner R, Koköfer A, Danninger T, Gerner P, Kirchmair L, Fritsch G. Comparison of tissue distribution, phrenic nerve involvement, and epidural spread in standard- vs low-volume ultrasound-guided interscalene plexus block using contrast magnetic resonance imaging: a randomized, controlled trial. Br J Anaesth. 2016;116:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Sanllorente-Sebastián R, de Vicente-Lorenzo JM, Mediavilla-Herrera FJ, Gutiérrez-García S, Alario-Poza IS, Bustinza-Beaskoetxea Z. Case report: serratus intercostal plane block/BRILMA and sedation for mastectomy in a high risk patient. Rev Esp Anestesiol Reanim (Engl Ed). 2019;66:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Pedrosa FP, Cravo H. Serratus Anterior Plane Block for Awake Breast Surgery: A Case Report. A A Pract. 2020;14:e01354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Malawat A, Verma K, Jethava D, Jethava DD. Erector spinae plane block for complete surgical anaesthesia and postoperative analgesia for breast surgeries: A prospective feasibility study of 30 cases. Indian J Anaesth. 2020;64:118-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 21. | Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012;59:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 428] [Article Influence: 32.9] [Reference Citation Analysis (0)] |