Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5680
Peer-review started: October 23, 2021
First decision: January 22, 2022
Revised: March 28, 2022
Accepted: April 20, 2022
Article in press: April 20, 2022
Published online: June 16, 2022
Processing time: 228 Days and 17.5 Hours
The pedicle screw-laminar hook system has strong fixation and is conducive to bone graft fusion for lumbar spondylolysis. However, the current pedicle screw-laminar hook fixation system is not specifically designed for lumbar spon
To investigate the clinical effects of a new anatomical hook-rod-pedicle screw system in the treatment of lumbar spondylolysis in young adults.
We designed a new anatomic hook-rod-pedicle screw system for young patients with lumbar spondylolysis. The isthmus and the corresponding pedicle screw entry point were exposed through the intermuscular approach. Autogenous iliac bone graft was obtained to bridge the isthmus defect, and then the anatomic hook-rod-pedicle screw system was used to fix the isthmus in 15 young patients.
At 24 mo follow-up, the visual analogue scale score of low back pain decreased from 6.73 ± 0.88 to 0.73 ± 0.59, and the Oswestry disability index score decreased from 58.20 ± 8.99 to 7.87 ± 4.97. Computed tomography showed bilateral isthmic bone healing in 14 cases and unilateral isthmic bone healing in 1 case. Magnetic resonance imaging showed that the lumbar disc signal of diseased segment and adjacent segments had no change compared with that before surgery. The pain visual analogue scale score of the donor site was 0.20 ± 0.41 at the last follow-up. According to the Modified Macnab score, the excellent and good rate was 100%.
The application of this new anatomical hook-rod-pedicle screw system to treat young patients with lumbar spondylolysis has the advantages of less trauma, a simple operation and satisfactory clinical effects.
Core Tip: Lumbar spondylolysis is one of the common causes of low back pain in adolescents. The main indication for surgical repair of lumbar spondylolysis is that low back pain is not relieved after at least 6 mo of non-surgical treatment. Application of isthmus debridement, bone grafting and a new anatomical hook-rod-pedicle screw system fixation in young patients with lumbar spondylolysis has the advantages of less trauma, a simple operation and satisfactory curative effect.
- Citation: Li DM, Li YC, Jiang W, Peng BG. Application of a new anatomic hook-rod-pedicle screw system in young patients with lumbar spondylolysis: A pilot study. World J Clin Cases 2022; 10(17): 5680-5689
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5680.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5680
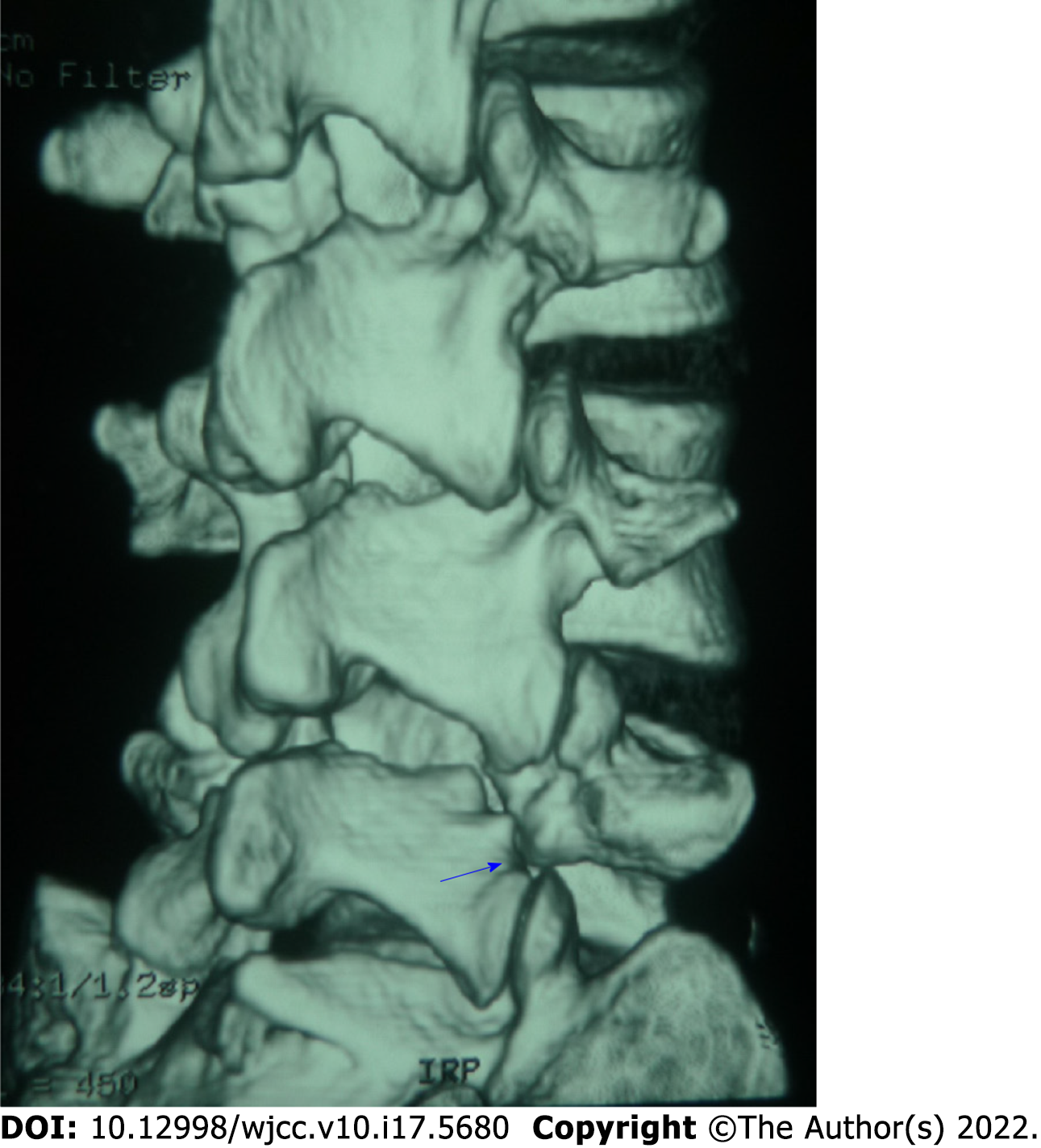
Spondylolysis is a bony defect in the pars interarticularis of a vertebra, which can be complete or incomplete, bilateral or unilateral and more commonly complete bilateral (Figure 1)[1-3]. It is often asymptomatic but quite common in young people and adolescents with low back pain[4,5]. These patients are usually treated conservatively with analgesics, lumbar orthoses, limitation of movement and physical therapy, and surgery is performed only when the pain persists[6,7]. For this young group of patients, spinal surgeons have paid more and more attention to how to minimize the impact on the range of motion of the spine and prevent the adjacent segments from producing excessive mechanical stress[8,9], so as to turn their attention to repairing the pars interarticularis, bone grafting and restoring the stability of the posterior arch[10,11]. Because the most common lesion of spondylolysis is acquired pseudarthrosis, bone grafting combined with internal fixation is a treatment that does not require arthrodesis. There are multiple reports on direct pars repair techniques in the literature[12-15]. Two common methods are: (1) Direct repair using a lamina/pars compression screw through the isthmic defect; and (2) Compression of the isthmic defect using a set of pedicle screw, rod and laminar hook assembly within the same segment.
More and more surgeons repair lumbar isthmus defects with bone grafting and the pedicle screw-laminar hook system to treat young patients with lumbar spondylolysis because of its firm fixation and good clinical effect[16-18]. However, the pedicle screw-laminar hook systems currently in use are not specifically designed for the treatment of lumbar spondylolysis. It has some disadvantages, such as incomplete matching between hook and lamina, difficulty in installation between rod and pedicle screw and large trauma. Complete exposure of the lamina is usually required, resulting in excessive paraspinal soft tissue dissection. To this end, we designed a new anatomical hook-rod-pedicle screw system for lumbar spondylolysis and observed its clinical efficacy.
From April 2017 to July 2018, 15 men with an average age of 22 (18-30 years) participated in the study. There were 11 cases of single segment, including L4 (1 case) and L5 (10 cases) and 4 cases of double segments, including L3 and L5 (1 case) and L4 and L5 (3 cases). All cases were bilateral isthmus defects. Inclusion criteria were: (1) The patient presented with severe low back pain and limited lumbar function but no radiating pain (sciatica) in the lower extremities; (2) Computed tomography (CT) of the lumbar spine showed spondylolysis but no spina bifida or missing lamina, and dynamic lumbar radiographs showed no lumbar instability and spondylolisthesis; (3) At isthmic defect and adjacent levels, there was no disc degeneration on magnetic resonance imaging (MRI); (4) Conservative treatment, such as restriction of movement, oral anti-inflammatory analgesics and physiotherapy for 3-6 mo, did not relieve symptoms; and (5) Positive diagnosis test (low back pain disappeared after injection of small dose local anesthetics into the isthmus defect site). Exclusion criteria were metabolic diseases or chronic inflammatory diseases, such as arthrolithiasis, rheumatoid arthritis or ankylosing spondylitis. Physical examination revealed limited lumbar motion, tenderness above and/or adjacent spinous processes and normal motor, sensory and tendon reflexes in both lower extremities.
The study was approved by the ethical review committee from The Third Medical Centre of Chinese PLA General Hospital, and the study was in accordance with the Helsinki Declaration. All patients gave informed written consent.
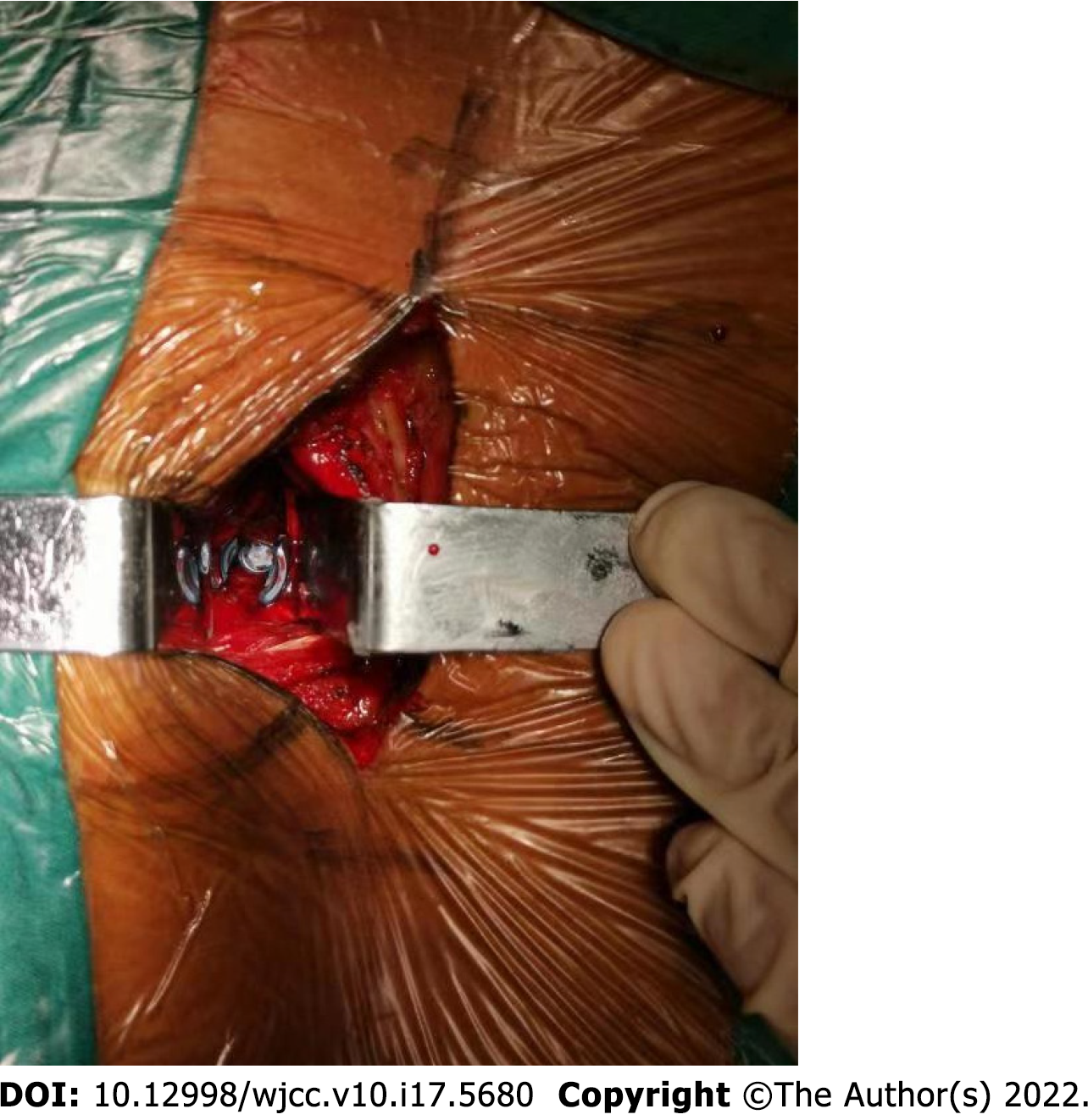
The patient was placed prone on the operating table under general endotracheal anesthesia, carefully cushioning all pressure points and keeping the neck in a neutral position. A midline incision was made, cutting the skin to the deep fascia layer. The deep fascia was cut longitudinally 1.5 cm outside the midline. The longissimus-multifidus muscle interval was bluntly dissected with a finger to avoid unnecessary tissue damage (Figure 2). Through the intermuscular approach, the isthmic defect site and the insertion point of the pedicle screw were exposed, and the fibrous tissue at the defect area was removed. A high-speed burr was used to debride sclerotic surfaces until bleeding bone surface was seen in the fractured pars. Gross motion was noted in the fissure area of the isthmus. Care was taken not to injure the facet joint capsule. Then a universal multiaxial pedicle screw was inserted into the corresponding vertebral body. Autogenous bone graft was obtained from the posterior superior iliac crest and implanted into the isthmus defect site, and the donor area of the posterior superior iliac crest was filled with allogeneic bone. After releasing the lower edge of the lamina with the ligamentum flavum stripper, the middle part of the hook rod was clamped with the rod holding forceps, and the hook could easily hook the lower edge of the lamina. The rod end of the anatomical hook was connected with the multiaxial pedicle screw. The construct was then loaded with compression force and tightened.
The contralateral anatomical hook-rod-pedicle screw was installed in the same way. After the installation of both sides, there was no loosening of the hook-rod-pedicle screw system and no movement of bone graft. Then the wound was rinsed with saline, the drainage tube was placed, and the incision was closed layer by layer. The average intraoperative blood loss was 40 mL (28-56 mL). On the second day after the operation, the drainage tube was pulled out, and the patient put on a lumbar brace and got out of bed for low back muscle function exercise. Three months after the operation, the brace can be removed for normal activity and exercise.
The visual analog scale (VAS) score (in the range of 0 = no pain to 10 = worst pain) was used to evaluate the severity of back pain and donor area pain. The Oswestry disability index (ODI) was used for functional assessment. The measures were recorded preoperatively and 3, 6, 12 and 24 mo after surgery. Functional status was qualified as “excellent,” “good,” “fair” and “poor” according to the Modified Macnab criteria[19] and recorded at 3, 6, 12 and 24 mo postoperatively.
Lumbar plain radiographs, CT and MRI were re-examined at 3, 6, 12 and 24 mo after operation. Lumbar plain radiographs were used to evaluate whether the internal fixation was loose and broken. CT was used to evaluate the fusion of the isthmic fracture and the osteogenesis of the iliac crest donor site. MRI was used to evaluate the degeneration of the intervertebral disc in the corresponding segment of lumbar spondylolysis.
Data were expressed as the mean ± standard error of the mean. Statistical analyses were carried out using SPSS 22.0 (IBM Corporation, Armonk, NY, United States). The VAS score and ODI before and after operation were compared using the paired t-test. The significance level was set to 0.05.
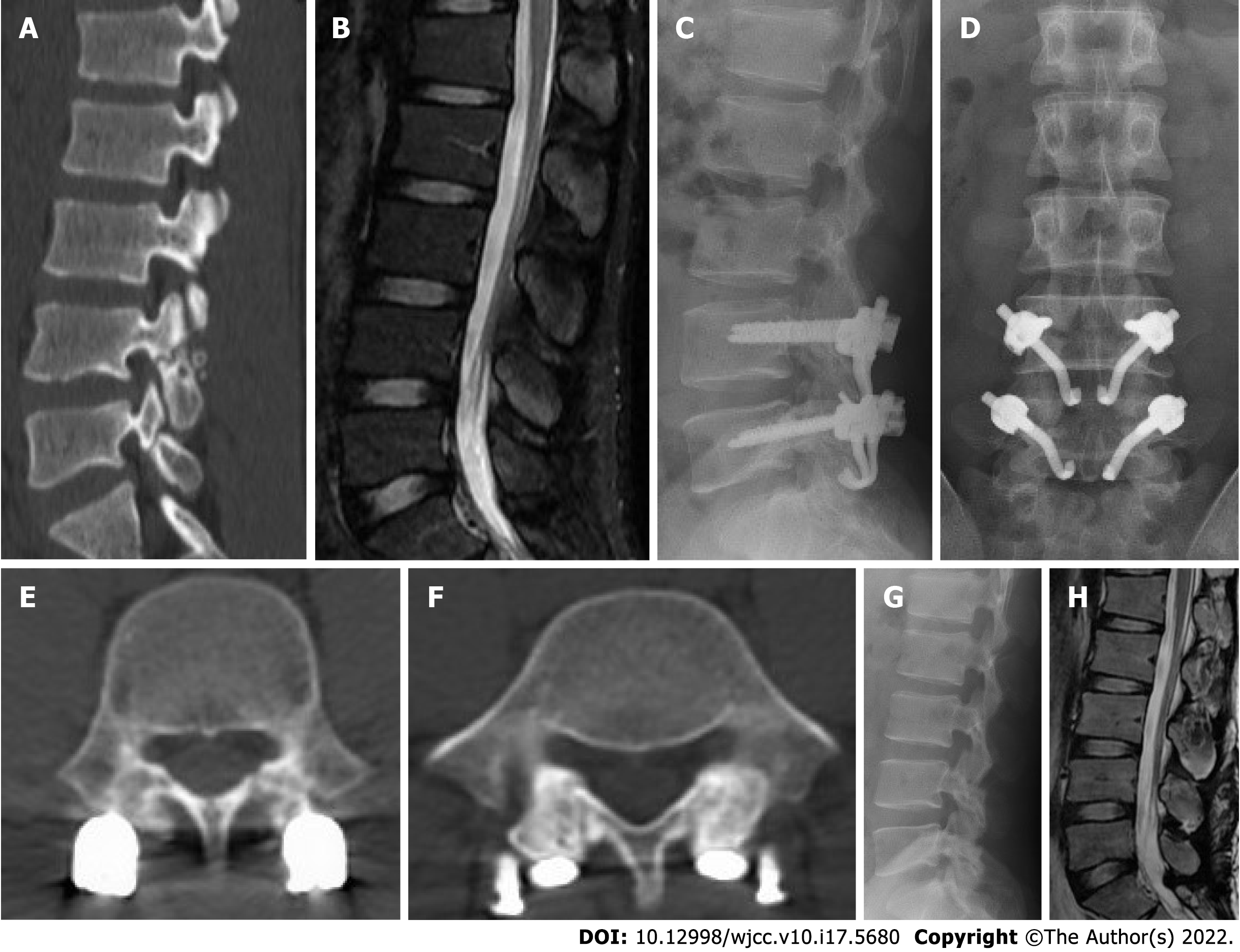
During the follow-up period of 24 mo, no patient developed sciatica or motor or sensory disturbance. The VAS score of low back pain and ODI score at 3, 6, 12 and 24 mo postoperatively significantly improved compared with those before surgery (P < 0.05, Table 1). At 24 mo after operation, the VAS score of low back pain decreased from 6.73 ± 0.88 preoperatively to 0.73 ± 0.59 postoperatively, and the ODI score decreased from 58.20 ± 8.99 preoperatively to 7.87 ± 4.97 postoperatively (Table 1). CT showed bilateral isthmus bone fusion in 14 cases and unilateral isthmus bone fusion in 1 case. The signs of intervertebral discs in diseased and adjacent segments had no change on MRI. The VAS score of donor site pain was 0.20 ± 0.41. Allogeneic bone filling in the bone donor site showed osteogenesis (Figure 3). According to the Modified Macnab standard, the excellent and good rate of operation was 100% at 24 mo follow-up (Table 2). A typical case was shown in Figure 4.
| Postoperative time | Excellent | Good | Fair | Poor |
| 3 mo | 5 (33) | 7 (47) | 3 (20) | 0 |
| 6 mo | 6 (40) | 8 (53) | 1 (7) | 0 |
| 12 mo | 8 (53) | 7 (47) | 0 | 0 |
| 24 mo | 10 (67) | 5 (33) | 0 | 0 |
Lumbar spondylolysis is one of the common causes of low back pain in adolescents[4]. The incidence rate is 3%-10% in adolescents and 6% in adults[20,21]. More than 80% of lumbar spondylolysis appears in L4 and L5[4]. Patients with lumbar spondylolysis mostly like sports or engage in sports, dancing and other industries. The specific cause of spondylolysis may be stress fractures caused by long-term fatigue on the basis of isthmic dysplasia. For the treatment of symptomatic lumbar spondylolysis in adolescents, active measures should be taken to avoid further problems such as intervertebral disc degeneration, herniation, lumbar instability or spondylolisthesis. If early diagnosis of lumbar spondylolysis is made in adolescents, measures such as wearing a lumbosacral brace and restricting movement will most likely result in isthmic healing[7], but those who do not heal should be actively treated by surgery. The main indication for surgical repair of lumbar spondylolysis is that low back pain is not relieved after at least 6 mo of non-surgical treatment, including activity modification, bracing and physical therapy. Aggravation of pain, deterioration of neurological symptoms and progressive listhesis also are indications for surgical consideration. In the present study, our patient group, due to severe low back pain, failure of conservative treatment for more than 3 mo, isthmus dissection, osteosclerosis and nonunion, needed surgical treatment.
There are many surgical methods for lumbar spondylolysis. In 1968, Kimura[22] described an isolated bone graft that directly repaired the isthmus defect without internal fixation and retained segmental activity but required a postoperative cast and long bed rest. Later, Scott[23] proposed the use of wire under the lamina and transverse processes, which has been improved by several authors over the years[24,25]. In 1970, Buck[26] first used screw internal fixation and bone grafting to repair defects directly, and subsequently other approaches with special constructs and temporary fixations were reported[27,28]. There were also posterolateral bone graft fusion, cross-segmental pedicle screw fixation and other methods. Patients with spondylolisthesis or disc herniation can be treated with pedicle screw fixation and interbody fusion[29].
The treatment of young patients with lumbar spondylolysis with isthmus debridement, bone grafting and pedicle screw laminar hook fixation has achieved satisfactory results[16-18], which proves that the pedicle screw-laminar hook system has strong fixation and is conducive to bone graft fusion. It is an intrasegmental fixation and does not affect the lumbar interbody movement and the kinematics of the adjacent segment. Studies[30-32] have reached a consensus that the lumbar intramuscular approach can reduce the dissection of paravertebral muscles, reduce the denervation of paravertebral muscles, preserve the structure of muscle ligament complex, reduce postoperative pain and recover quickly. However, the current pedicle screw-laminar hook fixation system is not specifically designed for lumbar spondylolysis but mainly for the correction of scoliosis. Before the hook is installed, the muscles around the spinous process and lamina need to be separated, resulting in severe tissue damage. At the same time, the installation of the system is difficult because the lamina, hook and pedicle screw are not on the same plane.
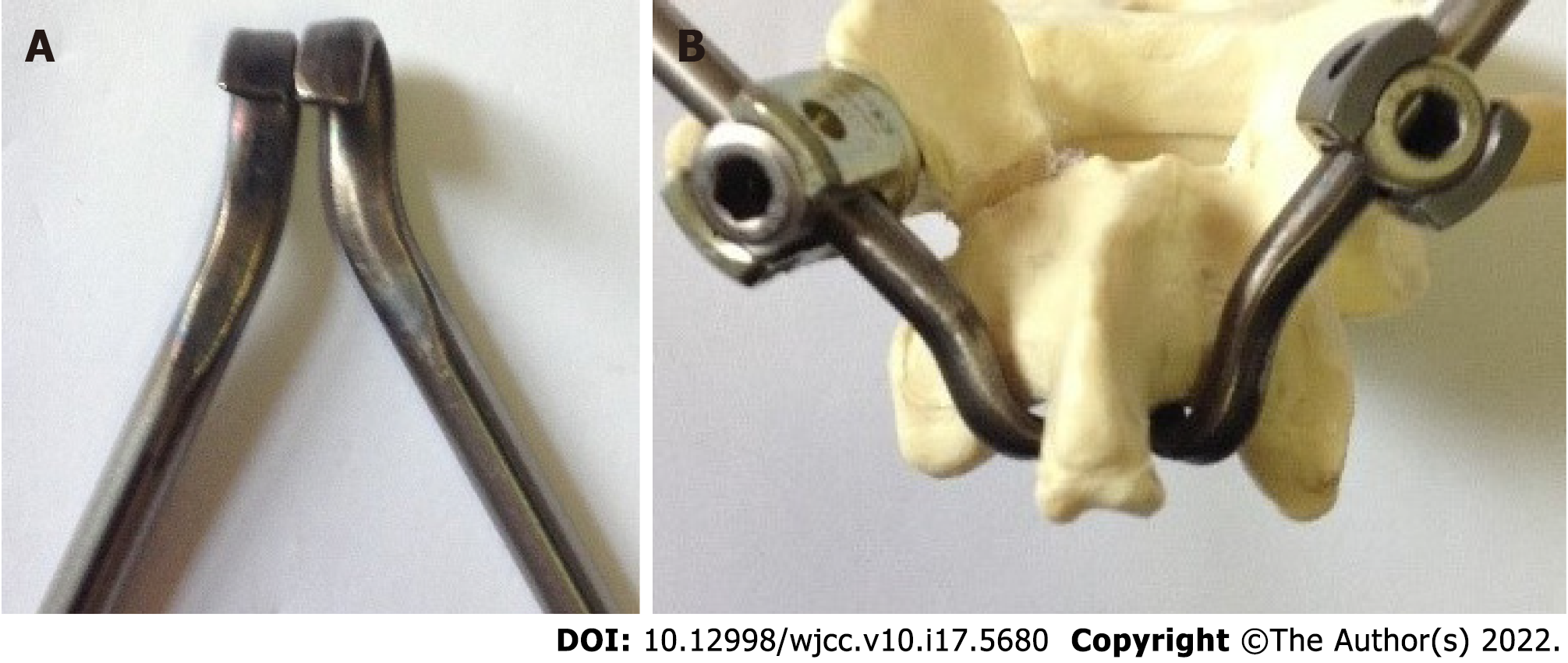
To solve these problems, we designed a new anatomical hook-rod instrument (Figure 5), which combined with pedicle screw to form anatomical hook-rod-pedicle screw system. The system can be installed by the intermuscular approach, which has the advantages of less trauma and convenient operation. At the same time, the system is firmly fixed, which is favorable for bone graft fusion. According to the anatomy of the lumbar spine, the spinous process is at a certain angle with the lamina, the lamina is inclined backward and upward, and the lower edge of lamina and the tail of pedicle screw are at a certain angle with the sagittal plane. According to the above anatomical features, the hook and the rod are inclined in these three directions. The hook is completely matched with the lamina, which is conducive to the installation of the hook at the lower edge of the lamina, and the rod is easy to connect with the universal pedicle screw. Of course, the angles of L4 and L5 are different. We have designed a series of hook-rods with different angles, which are convenient for operation. Of course, in terms of our new implant design, the fundamental principle of this system is only slightly novel compared with the traditional segmental pedicle screw rod and hook. However, according to our literature review, the design of this implant is unique so far.
In this study, 15 cases of young patients with lumbar spondylolysis were treated with isthmus repair, bone grafting and anatomical hook-rod-pedicle screw fixation and achieved satisfactory results. At the same time, the injury was small, and the operation was simple and convenient. However, in all 15 patients with lumbar spondylolysis who underwent repair of the isthmic defect, 1 patient with L5 bilateral isthmic defect had no bone healing on one side. Most of the isthmus defects occurred in preschool, and a few occurred in adulthood. Isthmus rupture will no longer occur in adulthood. After the occurrence of lumbar isthmus defect, the defect usually does not heal spontaneously. In this way, the broken ends of bone on both sides of the defect will atrophy and harden. In this case, nonunion after repair of the isthmus defect is a common complication. Because this is an intrasegmental fixation, the implant usually does not need to be removed. If unilateral nonunion occurs, the implant must not be removed.
Autologous iliac bone graft is the “gold standard” in bone grafting[33], and pain in the iliac bone donor area is a common complication after iliac bone removal[34]. There are many reasons for postoperative pain in the donor area, such as bone defect, adhesion, osteoporosis and cutaneous nerve injury in the donor area. A bone block with cortex and cancellous bone is taken from the posterior superior iliac spine and can be trimmed to a suitable size to meet the needs of bone grafting in the isthmus. To solve the problem of donor site pain, we used the allogeneic bone with tissue-engineered human bone morphogenetic proteins to fill the defect area of posterior superior iliac spine. Allogeneic bone contains bone morphogenetic proteins, which can induce new bone formation and promote bone growth. During the follow-up, bone growth was found in the defect of the posterior superior iliac spine, as shown in (Figure 3), and the pain in the bone donor area disappeared.
The application of isthmus debridement, bone grafting and anatomical hook-rod-pedicle screw system fixation in young patients with lumbar spondylolysis has the advantages of less trauma, a simple operation and satisfactory curative effect. However, it is not suitable for the cases of lumbar spondylolysis with spondylolisthesis. In addition, it is also not suitable for the cases with missing lamina, bone dysplasia and lumbar disc degenerative diseases. This new hook-rod-pedicle screw system is undergoing biomechanical testing and has been patented in China (Patent No.: ZL201721043286.7). This is a small sample observation study, and further large sample and prospective studies are needed to prove the superiority and reliability of the system.
Compared with the use of the traditional instrument, the application of this new anatomical hook-rod-pedicle screw system to treat young patients with lumbar spondylolysis has the advantages of less trauma, a simple operation and satisfactory clinical effects.
The pedicle screw-laminar hook system has strong fixation and is conducive to bone graft fusion for lumbar spondylolysis. However, the current pedicle screw-laminar hook fixation system is not specifically designed for lumbar spondylolysis.
The pedicle screw-laminar hook system currently in use is not specifically designed for the treatment of lumbar spondylolysis. It has some disadvantages, such as incomplete matching between hook and lamina, difficulty in installation between rod and pedicle screw and large trauma. Complete exposure of the lamina is usually required, resulting in excessive paraspinal soft tissue dissection.
To investigate the clinical effects of a new anatomical hook-rod-pedicle screw system in the treatment of lumbar spondylolysis in young adults.
We designed a new anatomic hook-rod-pedicle screw system for young patients with lumbar spondylolysis. The isthmus and the corresponding pedicle screw entry point were exposed through the intermuscular approach. Autogenous iliac bone graft was obtained to bridge the isthmus defect, and then the anatomic hook-rod-pedicle screw system was used to fix the isthmus in 15 young patients.
At 24 mo follow-up, the visual analogue scale score of low back pain decreased from 6.73 ± 0.88 to 0.73 ± 0.59, and the Oswestry disability index score decreased from 58.20 ± 8.99 to 7.87 ± 4.97. Computed tomography showed bilateral isthmic bone healing in 14 cases and unilateral isthmic bone healing in 1 case. Magnetic resonance imaging showed that the lumbar disc signal of the diseased segment and adjacent segments had no change compared with that before surgery. The pain visual analogue scale score of the donor site was 0.20 ± 0.41 at the last follow-up. According to the Modified Macnab score, the excellent and good rate was 100%.
The application of this new anatomical hook-rod-pedicle screw system to treat young patients with lumbar spondylolysis has the advantages of less trauma, a simple operation and satisfactory clinical effects.
The new anatomical hook-rod-pedicle screw system should be evaluated in a large sample multicenter randomized controlled study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Augustin G, Croatia; Nanda SN, India S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Farfan HF, Osteria V, Lamy C. The mechanical etiology of spondylolysis and spondylolisthesis. Clin Orthop Relat Res. 1976;40-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res. 1976;23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 28] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Chen MR, Moore TA, Cooperman DR, Lee MJ. Anatomic variability of 120 L5 spondylolytic defects. Global Spine J. 2013;3:243-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Hensinger RN. Spondylolysis and spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1989;71:1098-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 130] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Nachemson A. Repair of the spondylolisthetic defect and intertransverse fusion for young patients. Clin Orthop Relat Res. 1976;101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Blanda J, Bethem D, Moats W, Lew M. Defects of pars interarticularis in athletes: a protocol for nonoperative treatment. J Spinal Disord. 1993;6:406-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 118] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 7. | Steiner ME, Micheli LJ. Treatment of symptomatic spondylolysis and spondylolisthesis with the modified Boston brace. Spine (Phila Pa 1976). 1985;10:937-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 115] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 8. | Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). 1988;13:375-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 542] [Cited by in RCA: 462] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 9. | Yang SW, Langrana NA, Lee CK. Biomechanics of lumbosacral spinal fusion in combined compression-torsion loads. Spine (Phila Pa 1976). 1986;11:937-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 78] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Cyron BM, Hutton WC. The fatigue strength of the lumbar neural arch in spondylolysis. J Bone Joint Surg Br. 1978;60-B:234-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 164] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Green TP, Allvey JC, Adams MA. Spondylolysis. Bending of the inferior articular processes of lumbar vertebrae during simulated spinal movements. Spine (Phila Pa 1976). 1994;19:2683-2691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 55] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Hefti F, Seelig W, Morscher E. Repair of lumbar spondylolysis with a hook-screw. Int Orthop. 1992;16:81-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Pavlovcic V. Surgical treatment of spondylolysis and spondylolisthesis with a hook screw. Int Orthop. 1994;18:6-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Ohmori K, Suzuki K, Ishida Y. Translamino-pedicular screw fixation with bone grafting for symptomatic isthmic lumbar spondylolysis. Neurosurgery. 1992;30:379-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod-screw construct and bone grafting of the pars defect. Spine (Phila Pa 1976). 1999;24:1252-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 70] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 16. | Tokuhashi Y, Matsuzaki H. Repair of defects in spondylolysis by segmental pedicular screw hook fixation. A preliminary report. Spine (Phila Pa 1976). 1996;21:2041-2045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 58] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Roca J, Iborra M, Cavanilles-Walker JM, Albertí G. Direct repair of spondylolysis using a new pedicle screw hook fixation: clinical and CT-assessed study: an analysis of 19 patients. J Spinal Disord Tech. 2005;18 Suppl:S82-S89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Debusscher F, Troussel S. Direct repair of defects in lumbar spondylolysis with a new pedicle screw hook fixation: clinical, functional and Ct-assessed study. Eur Spine J. 2007;16:1650-1658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | He L, Ni J, Wu B, Yue J, Cao G, Guo Y, Yang L. Coblation annuloplasty in cervical discogenic pain without radiculopathy. Wideochir Inne Tech Maloinwazyjne. 2020;15:305-312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Rajasekaran S, Kamath V, Avadhani A. Bucks fusion. Eur Spine J. 2010;19:343-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Smith JA, Hu SS. Management of spondylolysis and spondylolisthesis in the pediatric and adolescent population. Orthop Clin North Am. 1999;30:487-499, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 47] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Kimura M. [My method of filing the lesion with spongy bone in spondylolysis and spondylolistesis]. Seikei Geka. 1968;19:285-296. [PubMed] |
| 23. | Askar Z, Wardlaw D, Koti M. Scott wiring for direct repair of lumbar spondylolysis. Spine (Phila Pa 1976). 2003;28:354-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Hambly MF, Wiltse LL. A modification of the Scott wiring technique. Spine (Phila Pa 1976). 1994;19:354-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J Bone Joint Surg Br. 1992;74:426-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52:432-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 181] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg. 1984;103:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 105] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Louis R. [Pars interarticularis reconstruction of spondylolysis using plates and screws with grafting without arthrodesis. Apropos of 78 cases]. Rev Chir Orthop Reparatrice Appar Mot. 1988;74:549-557. [PubMed] |
| 29. | Zhang S, Ye C, Lai Q, Yu X, Liu X, Nie T, Zhan H, Dai M, Zhang B. Double-level lumbar spondylolysis and spondylolisthesis: A retrospective study. J Orthop Surg Res. 2018;13:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | Vialle R, Wicart P, Drain O, Dubousset J, Court C. The Wiltse paraspinal approach to the lumbar spine revisited: an anatomic study. Clin Orthop Relat Res. 2006;445:175-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 31. | Suk KS, Lee HM, Kim NH, Ha JW. Unilateral versus bilateral pedicle screw fixation in lumbar spinal fusion. Spine (Phila Pa 1976). 2000;25:1843-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 114] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Whitecloud TS 3rd, Roesch WW, Ricciardi JE. Transforaminal interbody fusion versus anterior-posterior interbody fusion of the lumbar spine: a financial analysis. J Spinal Disord. 2001;14:100-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Dhawan A, Kuklo TR, Polly DW Jr. Analysis of iliac crest bone grafting process measures. Am J Orthop (Belle Mead NJ). 2006;35:322-326. [PubMed] |
| 34. | Delawi D, Dhert WJ, Castelein RM, Verbout AJ, Oner FC. The incidence of donor site pain after bone graft harvesting from the posterior iliac crest may be overestimated: a study on spine fracture patients. Spine (Phila Pa 1976). 2007;32:1865-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |