Published online May 6, 2022. doi: 10.12998/wjcc.v10.i13.3981
Peer-review started: July 16, 2021
First decision: October 18, 2021
Revised: October 26, 2021
Accepted: March 14, 2022
Article in press: March 14, 2022
Published online: May 6, 2022
Processing time: 287 Days and 17 Hours
In this review intended for medical staff involved in patient rehabilitation, we provided an overview of the basic methods for managing amputation stumps. After the amputation surgery, it is imperative to optimize the remaining physical abilities of the amputee through rehabilitation processes, including postoperative rehabilitation, desensitization, and continuous application of soft or rigid dressings for pain reduction and shaping of the stump. Depending on the situation, a prosthesis may be worn in the early stage of recovery or an immediate postoperative prosthesis may be applied to promote stump maturation. Sub
Core Tip: Postoperative complications after amputation surgery include pain, hematomas, infection and tissue necrosis, joint contracture, muscle weakness, and phantom sensations or pain; in this regard, proper post-surgical management of the amputation stump is imperative. This review provides an overview of the basic methods for managing amputation stumps. Our review is expected to contribute to the establishment of basic protocols that will be useful for stump management from the time of completion of amputation surgery to the fitting of a prosthesis to optimize patient recovery.
- Citation: Choo YJ, Kim DH, Chang MC. Amputation stump management: A narrative review. World J Clin Cases 2022; 10(13): 3981-3988
- URL: https://www.wjgnet.com/2307-8960/full/v10/i13/3981.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i13.3981
Limb amputation refers to partial or total loss or removal of the upper or lower limbs. Among the causes of upper limb amputation, physical trauma is the most common, whereas peripheral artery disease is the leading cause of lower limb amputation. Other reasons for amputation include congenital limb defects, tumors, and chronic osteomyelitis[1,2]. Postoperative complications after amputation surgery include pain, hematomas, infection and tissue necrosis, joint contracture, muscle weakness, and phantom sensations or pain; in this regard, proper post-surgical management of the amputation stump is imperative[3]. Additionally, it is important to maintain the shape of the stump after amputation surgery, and essential for the amputee to undergo training for the wearing and use of a prosthesis. Therefore, the aim of this review was to provide a comprehensive overview of stump management methods for medical staff to optimize patient recovery.
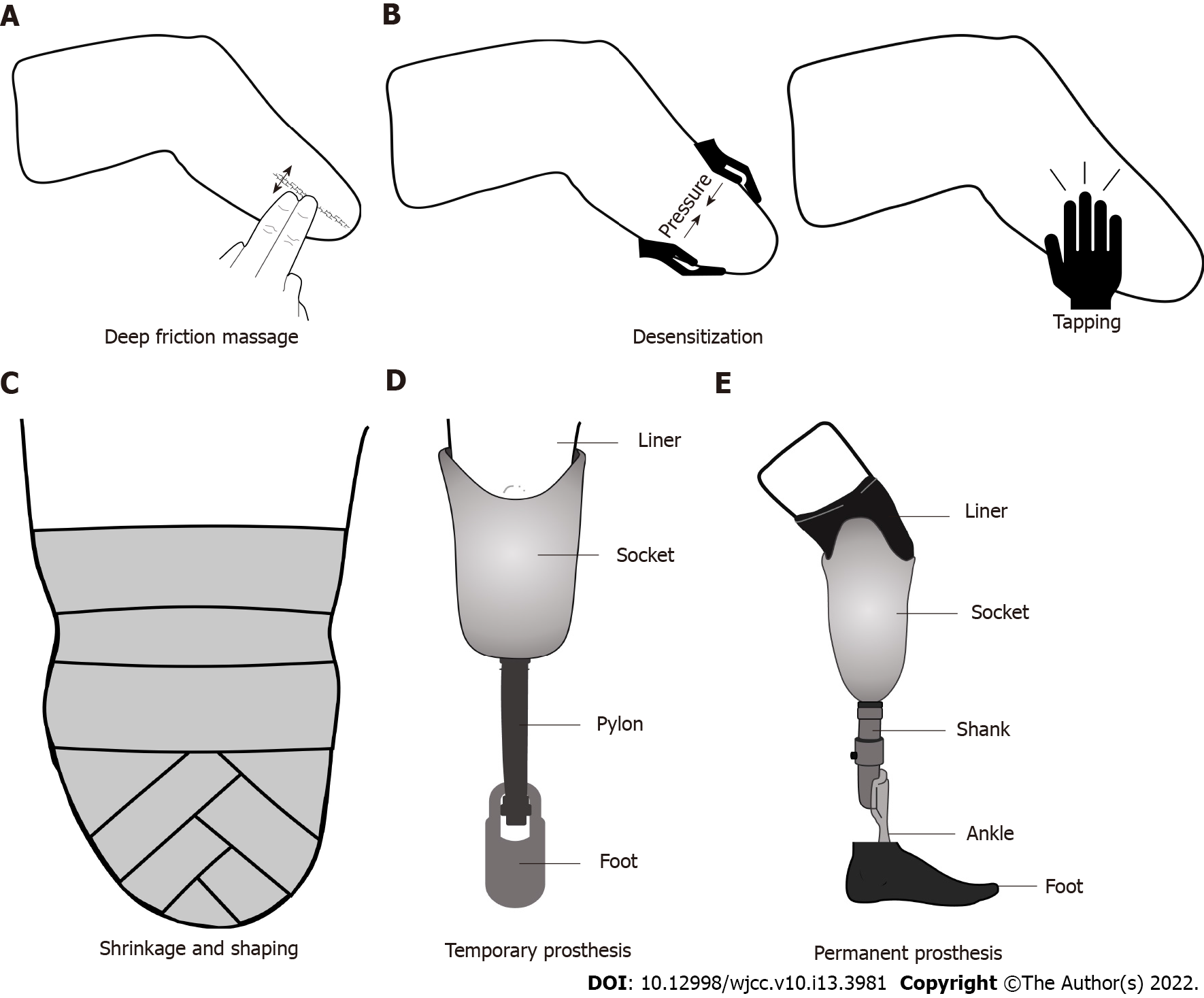
Desensitization is performed to eliminate or minimize the physical or psychological responses to a stimulus. In the case of amputation, the stump is highly sensitive after surgery, necessitating desensitization procedures, which may include gentle massage, light tapping, vibration, constant pressure, and the application of various fabrics to the sensitive area. After the stump is completely healed, active massage therapy is recommended to prevent skin adhesion and to allow additional sensory transmission to the stump, as massaging the area trains the patient to tolerate the pressure associated with contact between the stump and socket in the later stage of recovery[4]. Although it is recom-mended that desensitization be performed two to three times a day for at least 5 min, as there are no standardized guidelines outlining when to proceed with desensitization. The method and timing of desensitization may vary on an individual basis, depending on the state of the stump, and appropriate methods need to be selected and applied based on discussions with the rehabilitation team.
In 2018, Horne et al[4] investigated the effect of desensitization on pain, depression, and anxiety in 13 patients who had undergone lower limb amputation. In that study, desensitization was performed by gentle massage and stump tapping once every three hours, leading to an average reduction in pain scores of 1.92 points (measured using the Short-Form McGill Pain Questionnaire-2, range: 0-10 points) from postoperative day two to six, and an average reduction in depression and anxiety scores of 1.65 and 1.49 points, respectively (measured using the Hospital Anxiety and Depression Scale, range: 0-21 points). Thus, desensitization was shown to be significantly effective, and 85% of the patients indicated that desensitization helped control their pain after amputation surgery.
Shrinkage and shaping of the stump are the most important parts of the rehabilitation program prior to wearing a prosthesis, as improper shrinkage and shaping can impair blood circulation and wound healing. Four representative shrinkage and shaping methods include the application of soft, semi-rigid, or rigid dressings, as well as the fitting of a temporary prosthesis.
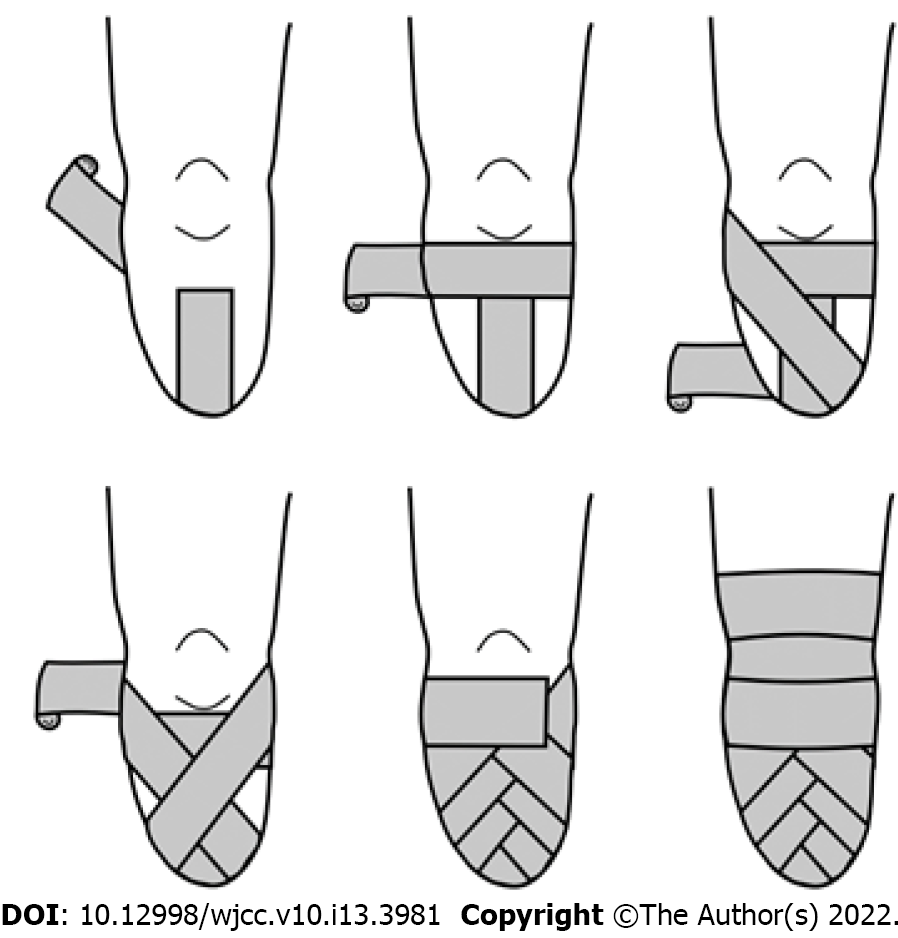
The purpose of a soft dressing is to fix the stump by wrapping it in a figure-8 shape, using an elastic or rubber bandage to promote healing and maturation of the stump after amputation surgery (Figure 1). This method reduces stump edema, prevents the occurrence of hematomas, facilitates conical shaping, and reduces exposure to bacteria to prevent infection or inflammation from external factors. When applying a soft dressing, care must be taken to ensure blood flow is not restricted by applying an optimal amount of pressure, and to establish the conical shape of the stump, the distal part should be wrapped more tightly than the proximal part. In the case of upper limb and below-the-knee amputations, a 10 cm-wide bandage is typically used, whereas for above-the-knee amputations, a 15 cm-wide bandage is used. When wrapping upper arm amputations, the bandage is applied up to the rib cage, and in a case of forearm amputation, the upper arm is bandaged as well. Bandages should be applied to the pelvis in above-the-knee amputations and to the femur in below-the-knee amputations. The bandages should be replaced three to five times daily to maintain adequate pressure on the stump and to reduce edema. Soft dressing is a commonly used stump fixation method; however, when the dressing is applied incorrectly, wound healing may be delayed or the affected area may become irregularly shaped, which may delay the wearing of a prosthesis[5]. Additionally, it is difficult to achieve early stump maturation to facilitate the wearing of a prosthesis with elastic bandages alone; in such cases, the stump may also be inadequately positioned, leading to difficulties in preventing joint contracture.
The application of a semi-rigid dressing is another fixation method employed to reduce edema and facilitate stump maturation. This method exploits the advantages of a rigid dressing and uses elastic materials to fix the stump, aiding in the healing process. A representative type of semi-rigid dressing is the air splint (Figure 2). The air splint method refers to the wearing of a splint containing a pocket of air over a bandaged stump, which compresses the stump and facilitates proper shrinkage. This method is advantageous in that the air splint is easy to wear, the state of the stump is easily visualized, and the method is psychologically reassuring to the patient. Balance training is possible when an air splint is applied in lower limb amputation; however, because the splint functions essentially as a pylon, proper gait training is impossible[6].
Rigid dressings involve fixing the stump using a plaster bandage after the amputation surgery. The goal of a rigid dressing is the same as that of a soft dressing, while providing the stump with better protection from trauma as a result of the harder surface. Additionally, rigid dressings are more effective than elastic bandages in preventing edema and hematomas, and early stump maturation can be achieved more easily. However, there are also disadvantages to rigid dressings; for example, they are heavier than soft dressings, separation from the stump may cause abrasions due to friction, and the state of the stump is not directly visible[5]. Therefore, to check the maturity of the stump, assess the wound healing process, or control the temperature and humidity of the stump and its surrounding environment, frequent replacement of the plaster bandage is an inconvenient requirement. If the temperature and humidity under a plaster bandage are not controlled and discharge is secreted from the stump or the wound is not healed, bacterial infection is likely to occur, requiring special care and attention.
While waiting for a stump wound to heal completely after an amputation, a temporary prosthesis may be worn to help train the patient prior to the wearing of a permanent prosthesis. This method can fix the stump much more effectively than wrapping with an elastic bandage, and it also serves as a means of evaluating an amputee’s rehabilitation potential. Additionally, in the case of lower limb amputation, rather than using crutches, walking while wearing a prosthesis facilitates adaptation, accelerating the time needed to achieve bipedal walking. This technique acts as a positive motivator for the amputee; it simplifies complex exercise programs, and increases the likelihood of a quick discharge and social reintegration. When fabricating a temporary prosthesis, it should resemble, as much as possible, the permanent prosthesis that will ultimately be used; this includes matching the alignment of the body positions and using the same materials to make the orthosis and other detailed parts. The temporary prostheses should not be used for residual limbs with burns, skin grafts, open wounds, infections, painful stumps, and dermatological conditions[7].
Immediate postoperative prosthesis (IPOP) is a method mainly employed in recovery from lower limb amputation. After amputation surgery, the stump is fixed with a rigid dressing and the pylon is connected with a foot prosthesis, allowing the amputee to proceed with training activities, such as sitting, standing, and walking as soon as possible. Depending on the situation, this method can be applied within two weeks following amputation surgery to reduce stump edema, and the psychological reassurance of being able to control weight-bearing activities and walking can prevent or reduce problems associated with phantom pain. Additionally, this method protects the stump from trauma, such as falls, and flexion contracture of joints can be controlled or prevented. By using the prosthesis and various parts early after the surgery, the amputee can gain experience with the prosthesis in advance, allowing his or her expectations to better align with the later reality of wearing the permanent prosthesis and improving the healing process. This experience facilitates the amputee’s ability to achieve independence in performing activities of daily living, enabling faster social reintegration and shortening the hospitalization period, which would entail an economic and a social advantage. However, in actual clinical practice, this is the least employed method of recovery due to various factors, such as the fear of wearing a prosthesis designed with rigid materials without sufficient preparation of the affected area or the feeling of repulsion resulting from one’s unfamiliarity with the treatment method[8].
Mueller[9], Evi et al[10], and Janchai et al[11] reported a significant decrease in stump edema in patients who received a combination of soft and rigid dressings compared with those who received soft dressings alone. Baker et al[12] reported that the rehabilitation period of patients receiving rigid dressings was considerably shorter than that of patients treated with soft dressings. Similarly, Vigier et al[13] reported that the wound healing and hospitalization periods after amputation were shorter when rigid dressings were applied than when soft dressings were used, and Moore et al[14] and Schon et al[15] reported that the incidence of complications, such as residual limb infections, bruises, necrosis, or ulcers was lower in patients using an IPOP than in patients using the soft or rigid dressings. Therefore, the literature suggests that compared with the soft dressings, the use of a rigid dressing or IPOP facilitates faster stump recovery and leads to fewer post-surgical complications.
With inadequate positioning or without continuous efforts to maintain recommended positions, joint contracture may occur that is difficult to correct and can cause difficulties when setting the alignment of the prosthesis. Following lower limb amputation, to prevent contracture and maintain a good position at rest, it is advisable not to sit or use a wheelchair for a prolonged period of time. On the bed after the surgery, a pillow should not be placed under the stump such that there is no flexion in the hip and knee joints. In the case of above-the-knee amputation, the prone position should be assumed whenever possible to ensure that extension of the hip joint can be maintained. When assuming the lateral position, the unaffected side should be facing downward to prevent abduction of the affected side. Additionally, care must be taken to maintain the horizontal orientation of the pelvis to prevent abduction contracture of the hip joint. When sitting following below-the-knee amputation surgery, prolonged flexion of the knee should be avoided, and when using a wheelchair, it is recommended to keep the knee joint extended by using a leg rest or leg board. Even after upper limb amputations, it is necessary not to place a pillow under the stumps. Additionally, following upper limb amputations, contractures can easily be prevented by performing joint range of motion exercises as soon as the pain subsides (about seven days after the surgery), regardless of the amputation level. About 2-3 wk after the surgery, performing light muscle-strengthening exercises can help prevent contractures[16]. The components of deformities that develop after amputations of each type are as follows: (1) For foot amputation: Equinus contracture; (2) For below-the-knee amputation: Knee flexion contracture; (3) For above-the-knee amputation: Hip joint abduction, external rotation, and flexion contracture; (4) For forearm amputation: Elbow flexion contracture; and (5) For upper arm amputation: Shoulder flexion, adduction, and internal rotation contracture[17].
Continuous exercise before wearing a prosthesis improves blood flow and enhances limb muscle strength and range of motion. Exercise can also help prevent joint contracture or correct contractures that have already occurred, in addition to reducing edema and improving cardiorespiratory fitness. Typically, essential exercises include those focused on improving balance, muscle-strengthening exercises to facilitate self-control of the amputated area, and training to perform activities of daily living, such as mobility-related tasks, dressing and undressing, and the use of utensils. Since the type of training exercise required prior to the wearing of a prosthesis differs for each amputated area, the appropriate methods should be adopted based on consultation with a physician. However, there are certain warm-up exercises that must be performed in all cases, regardless of the amputated area. For example, seven days after the amputation surgery, joint and isometric exercises should be performed at an intensity that the patient can tolerate for at least three weeks. In these exercises, the amputee adopts a pose, breathes deeply, and alternates between tensing and relaxing the stump’s muscles for about three minutes, with the purpose of this isometric exercise being to help maintain flexibility or strengthen the muscles. An isotonic exercise to increase muscle strength should be initiated after the pain or edema of the stump has decreased, which typically occurs approximately three weeks after the surgery.
Elastic resistance bands, such as TheraBand are mainly used for these exercises in clinical practice. The bands come in eight colors, depending on the amount of resistance, allowing one to select a band according to individual fitness levels. The TheraBand resistance bands can be applied in various ways for stump exercises. For example, when performing the lower extremity exercise, one side of the band is fixed to a rigid structure and the other side is made into a ring shape and wrapped around the stump, then adduction, abduction, flexion, and extension motions are repeatedly performed. For upper limb amputations, the muscles that are the main targets for exercise to help maintain muscle strength, body coordination, and endurance are the residual deltoid, biceps brachii, trapezius, serratus anterior, and pectoralis major. For lower limb amputations, the target muscles are the gluteus muscles, quadriceps femoris, biceps femoris, semitendinosus, and semimembranosus.
For all amputated body parts, special attention should be provided for skin care. To prevent adhesion of the surgical incision scar on the stump after the surgery, a deep friction massage is performed vertically around the scar line. The prosthesis is worn following stump maturation through desensitization and stump reduction. At this time, since the stump is inserted in the socket of the prosthesis, problems related to friction, such as abrasion, blisters, edema, furuncles, or boils, as well as bacterial infections may arise; therefore, proper hygiene is necessary. Of these complications, the management of edema is especially important. If edema is left untreated, discoloration, blisters, or ulcers may occur. As edema is exacerbated at high temperatures, care must be taken to control the temperature in the stump, bandage, and socket. General edema management methods include stretching, compression using elastic bandages, pneumatic or cooling compression, lymph node massage, and the application of high-voltage pulsed current. In severe cases of edema, the use of medications, such as anti-inflammatory drugs or more invasive methods, such as corticosteroid injections are adopted[18]. To prevent the aggravation of other skin problems, the skin and socket must be washed regularly to keep them clean, and the stockinette, socks, or elastic bandage worn on the stump must be properly dried after washing before use. Also, shaving should be avoided as much as possible, as it may create new scars on the skin surface. Cleansing products or perfumes containing alcohol should not be used on the amputated area, as the skin may become dry, resulting in cracking or peeling[19]. Additionally, wounds and ulcers on residual limbs can be healed using a vacuum-assisted socket suspension system, which can prevent the daily loss of stump volume that occurs with conventional sockets and minimize skin irritation of the stump by reducing shear stress[20].
Phantom limb pain is a common complication of amputation, and its prevalence has been reported to be 75%-80%[21]. Although the exact cause and pathophysiology of phantom limb pain are not elucidated, it is often considered as neuropathic pain due to dysfunction of the central and peripheral nervous systems[21]. Phantom limb pain has a high level of pain intensity and reduces the quality of life of amputees; it is challenging to manage and treat[22]. Methods of minimizing phantom limb pain include analgesics, mirror therapy, stump liners, acupuncture, targeted muscle reinnervation, repetitive transcranial magnetic stimulation, and transcranial direct current stimulation (tDCS). Others include imaginary phantom limb exercises, virtual and augmented reality, eye movement desensitization and reprocessing therapy, and plasma radiofrequency ablation. The commonly used methods are mirror therapy and transcranial magnetic stimulation[21-23]. Mirror therapy is a visual therapy that reflects the unaffected body of a unilateral amputated patient on a mirror and makes the patient think that they have limbs in the amputated area[24]. Through this method, patients have the illusion that the amputated body moves without pain. Cases of successful pain reduction through mirror therapy have been reported in patients with phantom limb pain[24,25]. tDCS is a brain stimulation method that is used to modulate cortical excitability, producing facilitatory or inhibitory effects[26]. tDCS can improve motor function in the upper or lower limbs and can be applied to patients with psychiatric problems to improve symptoms[27]. Mirror therapy and tDCS are non-invasive methods that cause reorganization of neuroplasticity for functional coordination and recovery of the brain[24,26].
In 2021, Gunduz et al[28] and Segal et al[27] investigated the effects of mirror therapy and tDCS for the management of phantom limb pain. Gunduz et al[28] compared the effects of mirror therapy only, sham tDCS, tDCS, and the combination of these in 112 patients with traumatic lower limb amputation. Treatment was performed for four weeks, and changes in pain were evaluated. The interventions were active or covered mirror therapy for four weeks combined with two weeks of either active or sham tDCS applied to the contralateral primary motor cortex. There was no interaction between mirror therapy and tDCS (P = 0.13), and among the four interventions, active tDCS was the most effective in reducing pain. Segal et al[27] compared the effects of mirror therapy only vs mirror therapy combined with tDCS. A total of 30 participants were recruited and randomly assigned to the mirror therapy group, mirror therapy and sham tDCS group, and mirror therapy and tDCS group. Treatment was carried out for two weeks, and pain intensity was measured. After three months of the treatment, the degree of pain in the group that received combined mirror therapy and tDCS was significantly reduced compared with that of the groups that received mirror therapy only, mirror therapy, and sham tDCS (P < 0.001).
There are no absolute rules for the selection of stump management methods, including exercises or skin care regimens, or the optimal timing for beginning to wear a prosthesis. Management decisions should be personalized for individual amputees based on various factors, such as his or her physical or mental state, the state and characteristics of the stump, and the purpose and timing of surgery. In general, a few points should be considered when determining if the patient is ready to begin wearing a prosthesis. For example, the stump must be well healed to minimize pain and reduce the risk of infection. Additionally, the stump should be conical in shape to prevent difficulties encountered with fitting the stump in the socket. Additionally, after beginning to wear a prosthesis, it is necessary to continue training to ensure muscle strength and balance are sufficient to allow for independent movement, and to minimize the risk of falls in the case of lower limb amputations. Figure 3 shows the stump management procedures for the period after amputation surgery to wearing the prosthesis.
This review summarized the methods for optimal stump management after amputation, providing useful information for medical staff to help establish and conduct rehabilitation programs for amputees.
Although many studies have been reported on stump management after upper arm, forearm, upper leg and lower leg amputations, studies have been insufficient on detailed management of a minor amputation (fingers or toes). Thus, future studies should address stump management methods after minor amputations. Additionally, general guidelines are used as management methods in all patients with amputation. There is no specific information on which management and treatment should be applied to certain situations after amputation. Different patients would require different management protocols, depending on their unique characteristics. Therefore, future studies should present management guidelines, according to demographic characteristics and symptoms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu C, China; Romano L, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Maduri P, Akhondi H. Upper Limb Amputation. 2022 Jan 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [PubMed] |
| 2. | Miller R, Ambler GK, Ramirez J, Rees J, Hinchliffe R, Twine C, Rudd S, Blazeby J, Avery K. Patient Reported Outcome Measures for Major Lower Limb Amputation Caused by Peripheral Artery Disease or Diabetes: A Systematic Review. Eur J Vasc Endovasc Surg. 2021;61:491-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 3. | Jirangkul P, Kosiyatrakul A, Gajaseni P. Late Presentation of Recurrent Symptomatic Amputation Neuroma. J Orthop Case Rep. 2020;10:28-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (3)] |
| 4. | Horne CE, Engelke MK, Schreier A, Swanson M, Crane PB. Effects of Tactile Desensitization on Postoperative Pain After Amputation Surgery. J Perianesth Nurs. 2018;33:689-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Kay HW. Wound dressings-soft, rigid, or semirigid. Orthot Prosthet. 1975;29:59-68. |
| 7. | Selvam PS, Sandhiya M, Chandrasekaran K, Rubella DH, Karthikeyan S. Prosthetics for Lower Limb Amputation. Orthot Prosthet. 2021;. [DOI] [Full Text] |
| 8. | Walsh T. Custom Removable Immediate Postoperative Prosthesis. JPO J Prosthe Orthot. 2003;15:158-161. |
| 9. | Mueller MJ. Comparison of removable rigid dressings and elastic bandages in preprosthetic management of patients with below-knee amputations. Phys Ther. 1982;62:1438-1441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Evi RNH, Elida I, Murdana INN, Tarigan THE, Werdhani RA. Efficacy of removable rigid dressing after transtibial amputation in diabetes mellitus patients. Med J Indonesia. 2013;22:16. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Janchai S, Boonhong J, Tiamprasit J. Comparison of removable rigid dressing and elastic bandage in reducing the residual limb volume of below knee amputees. J Med Assoc Thai. 2008;91:1441-1446. [PubMed] |
| 12. | Baker WH, Barnes RW, Shurr DG. The healing of below-knee amputations: a comparison of soft and plaster dressing. Am J Surg. 1977;133:716-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Vigier S, Casillas JM, Dulieu V, Rouhier-Marcer I, D'Athis P, Didier JP. Healing of open stump wounds after vascular below-knee amputation: plaster cast socket with silicone sleeve vs elastic compression. Arch Phys Med Rehabil. 1999;80:1327-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Moore WS, Hall AD, Lim RC Jr. Below the knee amputation for ischemic gangrene. Comparative results of conventional operation and immediate postoperative fitting technic. Am J Surg. 1972;124:127-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Schon LC, Short KW, Soupiou O, Noll K, Rheinstein J. Benefits of early prosthetic management of transtibial amputees: a prospective clinical study of a prefabricated prosthesis. Foot Ankle Int. 2002;23:509-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Bowker JH, Keagy RD, Poonekar PD. Musculoskeletal complications in amputees: Their prevention and management. In: Bowker J, Michael. Atlas of Limb Prosthetics: Surgical, Prosthetic, and Rehabilitation Principles, 2nd ed. Bethesda: O&P Library 1992: 665-680. |
| 17. | Bowker JH, Michael JH. Atlas of limb prosthetics. Surgical, Prosthetic, and Rehabilitation Principles. 1992: 453-478. |
| 18. | Miller LK, Jerosch-Herold C, Shepstone L. Effectiveness of edema management techniques for subacute hand edema: A systematic review. J Hand Ther. 2017;30:432-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 19. | Highsmith MJ, Kahle JT, Bongiorni DR, Sutton BS, Groer S, Kaufman KR. Clarification of content. Re: Highsmith MJ, Kahle JT, Bongiorni DR, Sutton BS, Groer S and Kaufman KR. Safety, energy efficiency, and cost efficacy of the C-Leg for transfemoral amputees: a review of the literature. Prosthet Orthot Int 2010; 34(4):362-377. Prosthet Orthot Int. 2011;35:113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Traballesi M, Delussu AS, Fusco A, Iosa M, Averna T, Pellegrini R, Brunelli S. Residual limb wounds or ulcers heal in transtibial amputees using an active suction socket system. A randomized controlled study. Eur J Phys Rehabil Med. 2012;48:613-623. [PubMed] |
| 21. | Li H, Li Y, Guo Z, Hao L, Tang Y, Guo Y, Zhang D, He L, Wang Y, Meng Y, Li F, Ni J. Low-temperature plasma radiofrequency ablation in phantom limb pain: A case report. Brain Circ. 2018;4:62-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Mioton LM, Dumanian GA, Shah N, Qiu CS, Ertl WJ, Potter BK, Souza JM, Valerio IL, Ko JH, Jordan SW. Targeted Muscle Reinnervation Improves Residual Limb Pain, Phantom Limb Pain, and Limb Function: A Prospective Study of 33 Major Limb Amputees. Clin Orthop Relat Res. 2020;478:2161-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 23. | Aternali A, Katz J. Recent advances in understanding and managing phantom limb pain. F1000Res. 2019;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 24. | Cárdenas K, Aranda M. [Psychotherapies for the Treatment of Phantom Limb Pain]. Rev Colomb Psiquiatr. 2017;46:178-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Folch A, Gallo D, Miró J, Salvador-Carulla L, Martínez-Leal R. Mirror therapy for phantom limb pain in moderate intellectual disability. A case report. Eur J Pain. 2022;26:246-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Thair H, Holloway AL, Newport R, Smith AD. Transcranial Direct Current Stimulation (tDCS): A Beginner's Guide for Design and Implementation. Front Neurosci. 2017;11:641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 161] [Cited by in RCA: 321] [Article Influence: 40.1] [Reference Citation Analysis (0)] |
| 27. | Segal N, Pud D, Amir H, Ratmansky M, Kuperman P, Honigman L, Treister R. Additive Analgesic Effect of Transcranial Direct Current Stimulation Together with Mirror Therapy for the Treatment of Phantom Pain. Pain Med. 2021;22:255-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 28. | Gunduz ME, Pacheco-Barrios K, Bonin Pinto C, Duarte D, Vélez FGS, Gianlorenco ACL, Teixeira PEP, Giannoni-Luza S, Crandell D, Battistella LR, Simis M, Fregni F. Effects of Combined and Alone Transcranial Motor Cortex Stimulation and Mirror Therapy in Phantom Limb Pain: A Randomized Factorial Trial. Neurorehabil Neural Repair. 2021;35:704-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (1)] |