Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3773
Peer-review started: July 5, 2021
First decision: July 26, 2021
Revised: July 26, 2021
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: April 26, 2022
Processing time: 290 Days and 1.5 Hours
Evaluation of the effectiveness of melatonin is necessary to prevent the development of delirium in hospitalized patients. Melatonin (N-acetyl-5-methoxytryptamine) is a hormone produced by the pineal gland of the brain from the amino acid tryptophan. Synthetic melatonin supplements have been used for various medical conditions, especially sleep-related diseases, and have proved to be successful.
To determine the effect of melatonin on the prevention of delirium in hospitalized patients.
A literature search of the CNKI, Wanfang Database, VIP Database, China Biomedical Literature Database, PubMed, Embase, Cochrane Library, Web of Science, and other databases was conducted. The CNKI, Wanfang Database, VIP Database (VIP), and China Biomedical Literature Database were searched for Chinese studies, and PubMed, Embase, Cochrane Library, Web of Science and other databases were searched for international studies. It will be established in June 2021 in a randomized controlled trial (RCT) whether melatonin treatment for 6 mo prevents delirium in hospitalized patients. Literature screening, quality review, and data extraction were carried out using the Cochrane Manual 5.1.0 systematic evaluation method, and Stata 15.0 software and Review Manager 5.3 were used for meta-analysis and processing.
A total of 18 new RCT articles and 18 experimental subjects were identified. The results of the meta-analysis showed that following the occurrence of delirium, melatonin reduced the incidence of delirium in patients (RR = 0.69, 95%CI: 0.60-0.80), which is of significance, but heterogeneity was significant I2 = 62%. Subgroup analysis was performed to examine the source of heterogeneity, and it was found that different patient types were the source of heterogeneity; the research on subgroup analysis was of high quality and homogeneous. To determine the reliability and robustness of the research results, a sensitivity analysis was carried out. The results showed that after excluding individual studies one by one, the effect size was still within 95%CI, which strengthened the reliability of the original meta-analysis results. Melatonin has a significant preventive effect on delirium in hospitalized medical patients [RR = 0.60, 95%CI: 0.47-0.76), P < 0.001].
Melatonin can reduce the rate of delirium in medical patients, and the role of melatonin in reducing the incidence of delirium in surgical patients and critical care unit patients requires further study.
Core Tip: Melatonin was shown to be effective in preventing delirium in hospitalized patients in this meta-analysis. Eighteen studies were reviewed involving 2137 patients and it was found that melatonin significantly reduced the incidence of delirium in hospitalized medical patients, but the effectiveness of melatonin in reducing the incidence of delirium in hospitalized surgical patients and intensive care unit patients requires further research.
- Citation: You W, Fan XY, Lei C, Nie CC, Chen Y, Wang XL. Melatonin intervention to prevent delirium in hospitalized patients: A meta-analysis. World J Clin Cases 2022; 10(12): 3773-3786
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3773.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3773
Delirium, also known as the state of conscious confusion, is a disorder of consciousness (which is the clarity of perceiving the environment), changes in consciousness (including changes in thinking), cognitive disorders, mental illness, and sleep-wake movements. The delirium is a recognized Complications of medical diseases, especially elderly patients, which is related to the mortality rate, and increase in Hospital costs[1,2]. In the palliative care setting, it is reported that the prevalence of delirium on admission is 20%-42%, and as high as 88% in the last few hours or days of life. Delirium is an acute neurocognitive disorder, in which a person's awareness of the surrounding environment is reduced, and attention disorder is its core feature; other mental deficits and perceptual abnormalities may also occur[3]. The collective symptoms of delirium can affect patients due to these characteristics and accompanying changes in psychomotor dysfunction or attention deficit hyperactivity disorder. Delirium is a symptomatic disorder, and its clinical management is challenging, especially when psychomotor agitation is present. This is especially true in the case of advanced disease and hospice care, where the patient's physical and functional decline can lead to a high degree of vulnerability to delirium (such as infections and adverse drug reactions)[5-6]. When delirium appears, it is associated with a mortality rate of 10% to 75%, although death may be more related to both advanced age and delirium. It is estimated that drug-induced delirium accounts for 22% to 39% of all cases. A study involving elderly hospitalized patients found that in their study population, the most likely cause of delirium was drug use[7-10]. Antipsychotics and anti-anxiety agents are FDA-approved therapies for the treatment or prevention of delirium; however, data have revealed their lack of efficacy and the risk of serious side effects[11].
Melatonin (N-acetyl-5-methoxytryptamine) is a hormone produced by the pineal gland in the brain from the amino acid tryptophan. Synthetic melatonin supplements have been used for various medical conditions, especially sleep-related diseases, and have proved to be successful[12]. Delirium is characterized by a disturbance in the circadian sleep-wake cycle, which leads to the hypothesis that the neurotransmitter melatonin and associated metabolic changes are involved in the pathogenesis of delirium. After admission, especially after admission to the intensive care unit (ICU), the metabolism of melatonin is disturbed, all of which are factors that cause delirium. These characteristics suggest an association between melatonin abnormalities and delirium. Although there is still a lack of evidence of causality[2], melatonin regulates the body’s sleep-wake cycle, season, and circadian rhythm[13]. It is a sleep-improving substance. Oral melatonin has been widely used nationally and internationally. Although melatonin depletion is considered to be one of the mechanisms of delirium, there have been some studies on the effect of melatonin on the prevention of delirium; however, there are differences in the various research results. Therefore, this study analyzed randomized controlled trials (RCTs) of melatonin interventions to prevent delirium using a meta-analysis, aiming to quantitatively synthesize the results of multiple studies to provide more reliable quantitative results and to target patients in different situations. The best intervention measures to prevent delirium in hospitalized patients are recommended to provide evidence-based data and serve as a basis for the prevention and clinical treatment of delirium in hospitalized patients.
The search was conducted using operating system principles (P: PIC, which stands for the research object; I: Search strategy, which stands for the search object); C: Comparison strategy, realization; O: Search research design, research design. The databases PubMed, Web of Science, Cochrane Library, Embase, and Chinese databases, including China Biomedical Literature Database, Wanfang Data Medical Journal Library, Weipu Database, CNKI, etc. were searched. The search period was from establishment of the database through June 2021. Chinese database search terms were: (Melatonin) and (OR delirium neurocognitive impairment) and (randomized controlled trial or randomized controlled or randomized) and English database search terms were "melatonin" and "Delirium" and 'randomized controlled trials' or 'randomized controlled trials' or 'randomized'.
The following search terms were used: ("Delirium" [Mesh]) OR (title) (acute subdelirium [title/abstract]) OR (delirium, sub [title/abstract]) OR (delirium, acute sub [title/abstract] OR (Sub-Delirium [title/abstract]) or (Mixed Origin Delirium [abstract]) OR (Mixed Origin Delirium [title/abstract]) OR (Mixed Origin Delirium [title/abstract]) AND (Melatonin [title/abstract]) AND (Randomized Controlled Trial [Publication Type] OR (Randomized [title/abstract] AND Control [title/abstract] AND Trial [title/abstract]). This study has been registered on the PROSPERO website (No. CRD42021264902).
Inclusion criteria were: (1) Research subjects: clinically hospitalized patients, including patients in surgery, internal medicine, and ICU, the criteria for diagnosing delirium were determined by the CAM = Delirium Confusion Assessment (CAM) criteria[14,15]; (2) Intervention measures: The selected study was an RCT, and there were no significant differences between the experimental group and the control group before the experiment; and (3) Outcome indicators: the main observation indicator was RR (Relative risk).
The exclusion criteria included: reviews, conference papers, systematic reviews, dissertations, animal experiments, repeat publications, unavailable full text or incomplete data extraction, low quality of the literature or obvious research flaws; already suffering from mental illness before admission, patients with abnormalities, severe sensory disturbances, history of depression or delirium, or long-term use of antipsychotic drugs.
Two researchers who had received systematic evidence-based training performed the literature assessment and data extraction. They independently read, screened, and retrieved relevant content based on the inclusion and exclusion criteria. Excel entry was used to extract data, the first author Wei You completed the literature screening, and data extraction was completed by author Xiaoyu Fan. After completion, cross-checking was carried out. If there was disagreement, this was resolved by discussion or joint negotiation with the third author Cheng Lei. The relevant data extracted from the included studies were the title, first author, publication time, research country (region), sample size, intervention time, evaluation indicators, and other information.
Two researchers who had undergone rigorous evidence-based training assessed the quality of the literature. The quality of the included studies was assessed using the bias risk assessment approach provided by the Cochrane Handbook 5.1.0, and discrepancies were addressed through discussion or by third-party researchers. The evaluated items included: (1) The generation of a random allocation plan; (2) Whether to carry out the allocation plan; (3) Whether to blind the subjects and researchers; (4) Whether to blind the evaluators; (5) Incomplete results; (6) Selectively reported research results; and (7) Other sources of bias. The evaluation result of "yes" indicated that the risk of bias was low; the result of "no" indicated that the risk of bias in the study was higher; "unclear" indicated that the study did not mention or did not have sufficient information to evaluate whether bias was present. Publication bias was tested using Egger's Funnel plots.
Review Manager 5.3 and Stata 15.0 software were used to conduct a meta-analysis on the extracted data. Subgroup analysis was conducted to analyze the heterogeneity of the included study results, and the corresponding effect model was selected based on the results: if P ≥ 0.1 and I2 < 50%, this indicated that the statistical heterogeneity between the studies was acceptable. A fixed-effects model was chosen for data merging; if P < 0.1 and I2 ≥ 50%, this indicated that the clinical heterogeneity between studies was large, and the source of heterogeneity was assessed or a random-effects model was chosen for data merging. Two categories of delirium incidence and relative risk (RR) were selected for analysis, and the 95%CI was calculated. When necessary, a sub-analysis of potential heterogeneity factors was performed, as well as an analysis to test the data.
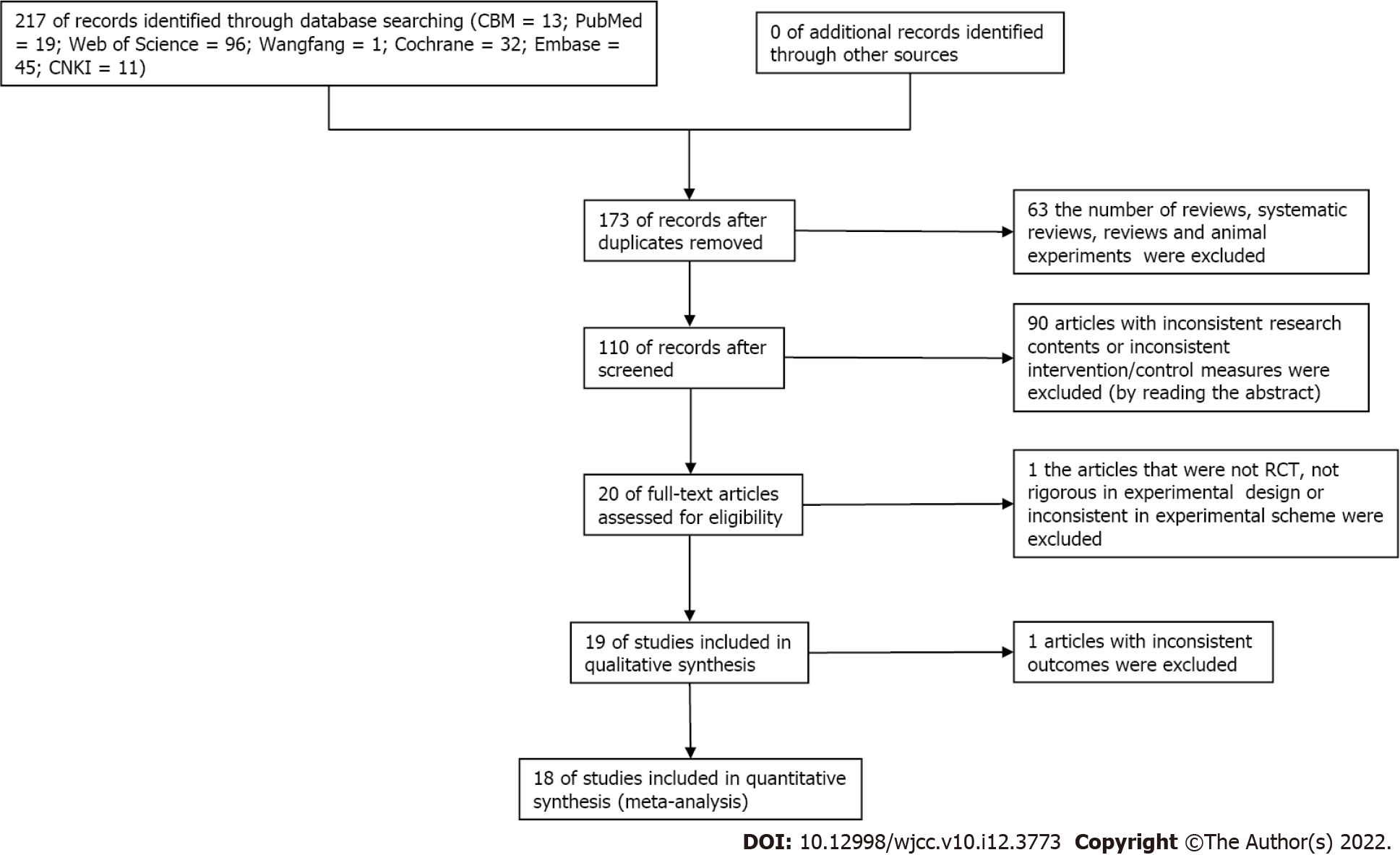
The flowchart of the research selection process is shown in Figure 1. The literature search retrieved 217 related documents from the Chinese and English databases. The document management software deleted 173 duplicate documents, read the titles and abstracts, and eliminated a total of 63 articles including reviews, systematic reviews, reviews, and animal experiments. Further research included reading the full text, deleting contents with inconsistent research data or inconsistent intervention measures/control measures (90 documents), excluding non-RCT literature (1), and one study with inconsistent outcome indicators was excluded. A total of 18 articles were finally re-analyzed, and the functions of the re-study are shown in Table 1. The basic characteristics of the literature in 18 articles were reviewed[16-33] and published in 2010-2021. The languages of the included literature are English and Chinese, and the study included 16 English articles and 2 Chinese articles. A total of 521 studies were involved. All included studies were divided into the control group and experimental group. The intervention in the experimental group was melatonin, and the intervention in the control group was a placebo (Table 1).
| Ref. | Sample size (example) | Intervention | Age | Diagnostic criteria | |||
| T | C | T | C | T | C | ||
| Sultan et al[16], 2010 | 53 | 49 | Melatonin | Placebo | 70.4 ± 7.1 | 72.3 ± 6.4 | CAM |
| de Jonghe et al[17], 2014 | 186 | 192 | Melatonin | Placebo | 84.1 ± 8.0 | 83.4 ± 7.5 | CAM |
| Wang et al[18], 2018 | 30 | 30 | Melatonin | Placebo | 70.7 ± 4.3 | 69.9 ± 4.5 | CAM |
| Prabhat et al[19], 2019 | 50 | 50 | Melatonin | Placebo | 69.30 ± 4.05 | 70.64 ± 3.76 | CAM |
| Ford et al[20], 2018 | 98 | 104 | Melatonin | Placebo | 69 ± 8.3 | 67.6 ± 8.0 | CAM |
| Chen et al[21], 2020 | 45 | 45 | Melatonin | Placebo | 71.36 ± 7.12 | 73.56 ± 6.65 | CAM |
| Javaherforoosh Zadeh et al[22], 2019 | 30 | 30 | Melatonin | Placebo | 60.26 ± 9.50 | 62.9 ± 8.08 | CAM |
| Oh et al[23], 2020 | 33 | 38 | Melatonin | Placebo | 71.3 ± 5.1 | 71.6 ± 5.2 | CAM |
| Al-Aama et al[24], 2010 | 61 | 61 | Melatonin | Placebo | 84.3 ± 5.9 | 84.6 ± 6.2 | CAM |
| Hatta et al[25], 2014 | 33 | 34 | Melatonin | Placebo | 78.2 ± 6.6 | 78.3 ± 6.8 | CAM |
| Agar et al[26], 2016 | 14 | 16 | Melatonin | Placebo | 76.3 ± 5.6 | 76.0 ± 5.3 | CAM |
| Jaiswal et al[27], 2018 | 36 | 33 | Melatonin | Placebo | 75.3 ± 5.3 | 75.6 ± 5.7 | CAM |
| Lawlor et al[28], 2020 | 30 | 30 | Melatonin | Placebo | 67 ± 5.9 | 67 ± 6.0 | CAM |
| Mengel et al[29], 2021 | 164 | 164 | Melatonin | Placebo | 74 ± 1.3 | 73 ± 1.5 | CAM |
| Vijayakumar et al[30], 2015 | 26 | 30 | Melatonin | Placebo | 36.9 ± 10.3 | 38 ± 14.4 | CAM |
| Nishikimi et al[31], 2017 | 45 | 43 | Melatonin | Placebo | 68.0 ± 5.1 | 68.0 ± 5.3 | CAM |
| Abbasi et al[32], 2018 | 67 | 70 | Melatonin | Placebo | 52.5 ± 18.4 | 49.9 ± 19 | CAM |
| Jaiswa et al[33], 2019 | 59 | 58 | Melatonin | Placebo | 58.1 ± 14.1 | 56.1 ± 15.8 | CAM |
The experimental group was given melatonin to prevent delirium, and the control group was given placebo to prevent delirium.
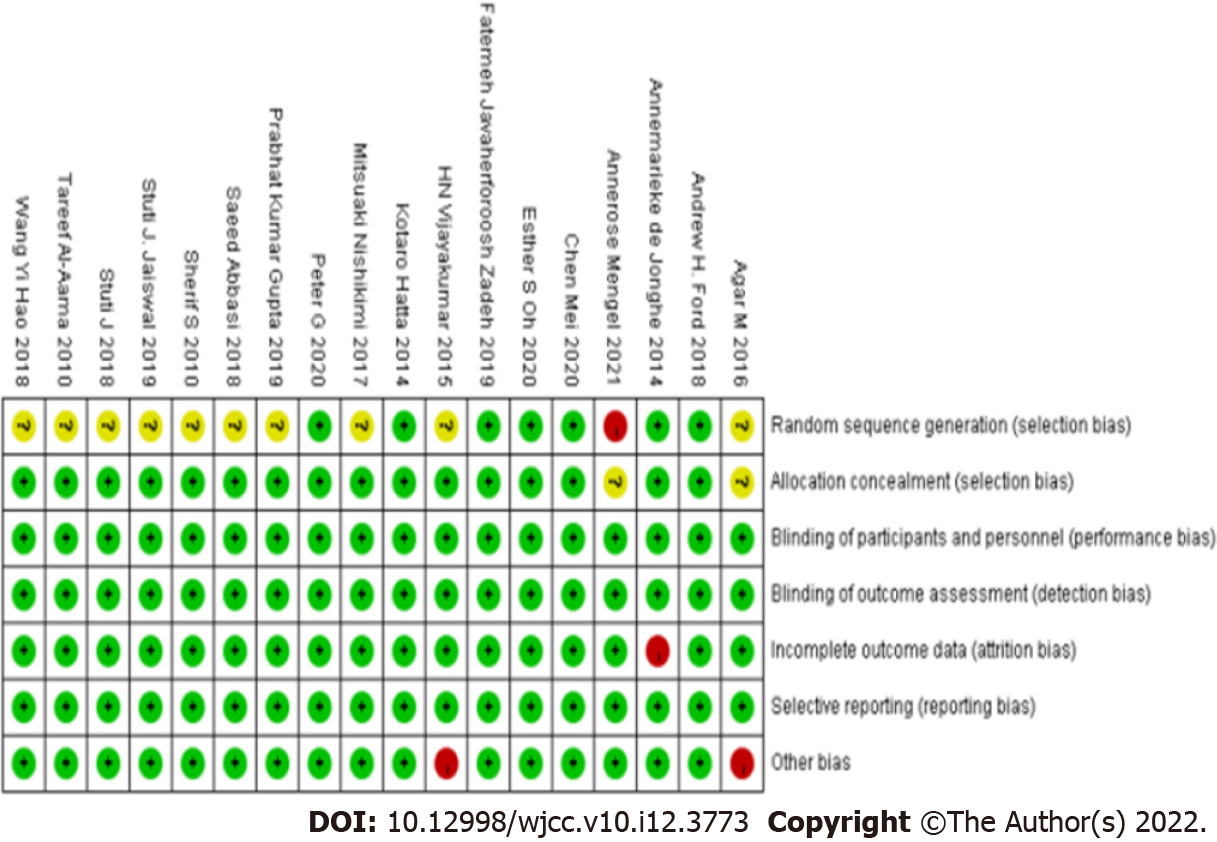
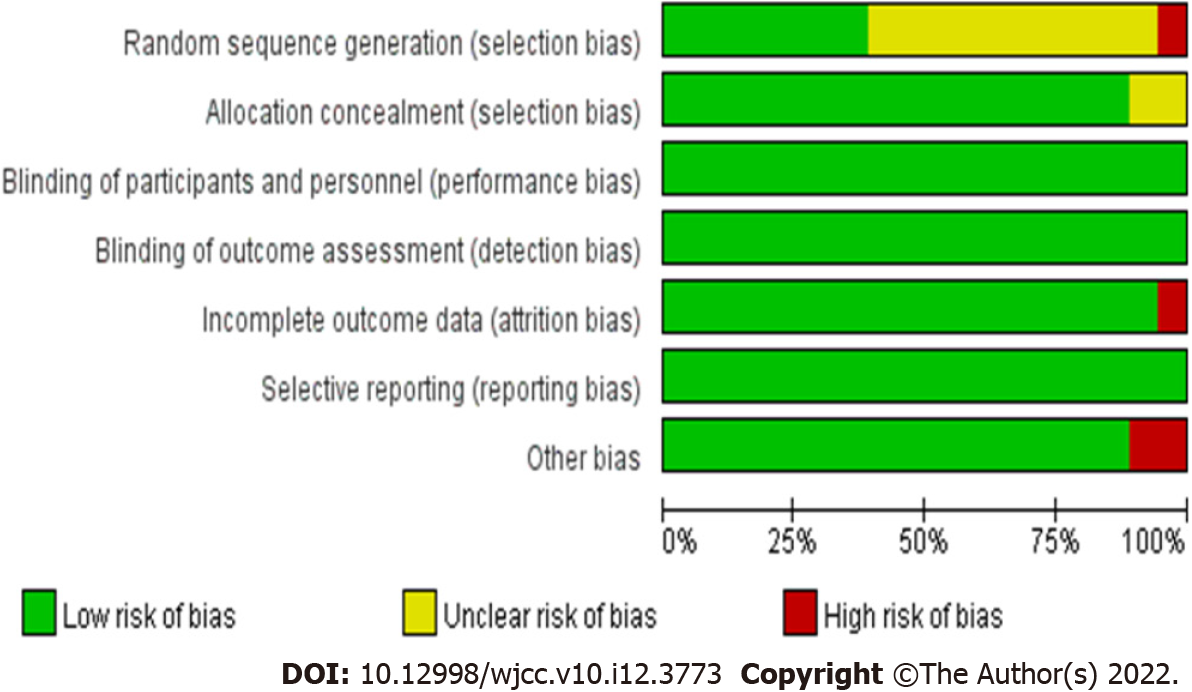
This study included 18 RCTs, 18 of which were of high quality, 6 of which scored 6 points, 7 of which described the method of random allocation sequence in full, and 18 assessed subjects using a blind approach. All trials provided complete data and no other potential risk of bias. The risk of bias in selective reporting was low. As shown in Figure 2, the standard was "+" and the standard "-" was not met. Figure 3 shows a statistical chart of the proportion of each item in the literature quality evaluation. See Figure 2 and Figure 3 for details.
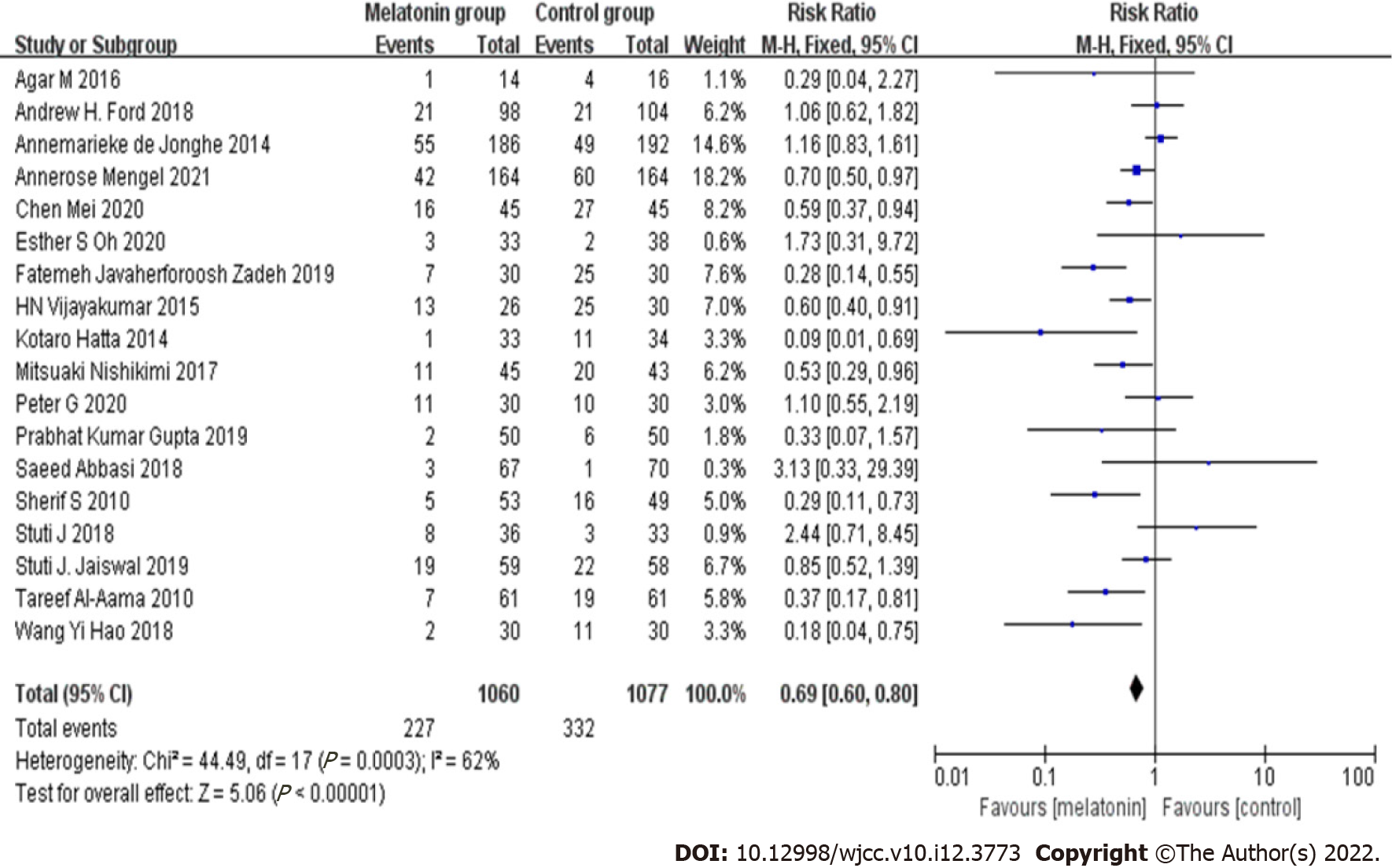
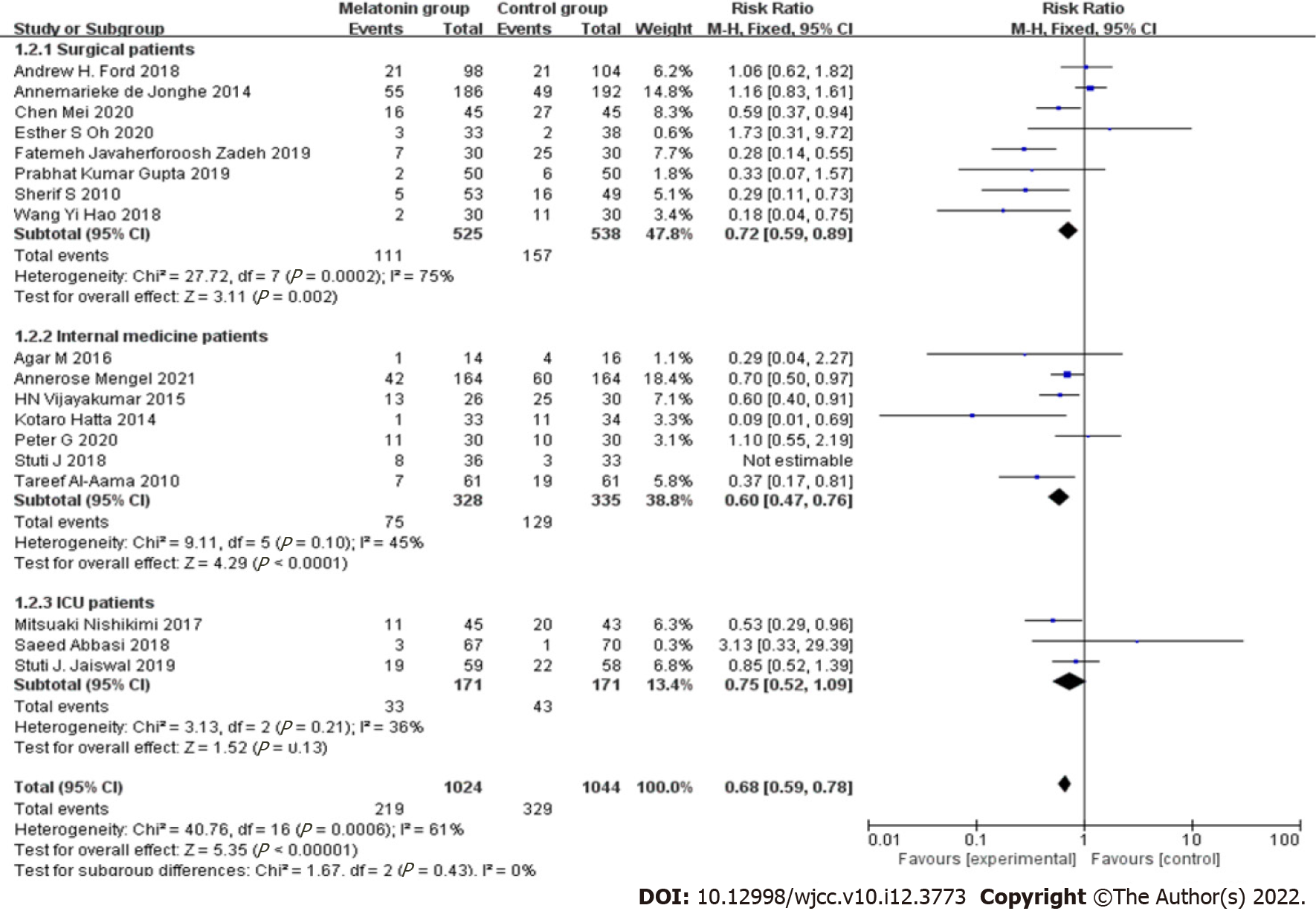
The overall effect of melatonin in all selected samples showed that it prevented delirium in hospitalized patients. Overall homogeneity (I2 = 62%, P < 0.0003) indicated multiple studies, and there was heterogeneity between the data; therefore, the random-effects model was used for analysis, but subgroup analysis was needed to determine the heterogeneity between multiple sets of data in this meta-analysis, as shown in Table 2 and Figure 4 (Forest map).
| Independent sample | Homogeneity test | Two-tailed test | Effect size and 95% confidence interval | ||||
| χ2 | P | I2 | Z | P | |||
| Random effects model | 2137 | 44.49 | P < 0.0003 | 62% | 5.06 | P < 0.00001 | 0.69 (0.60, 0.80) |
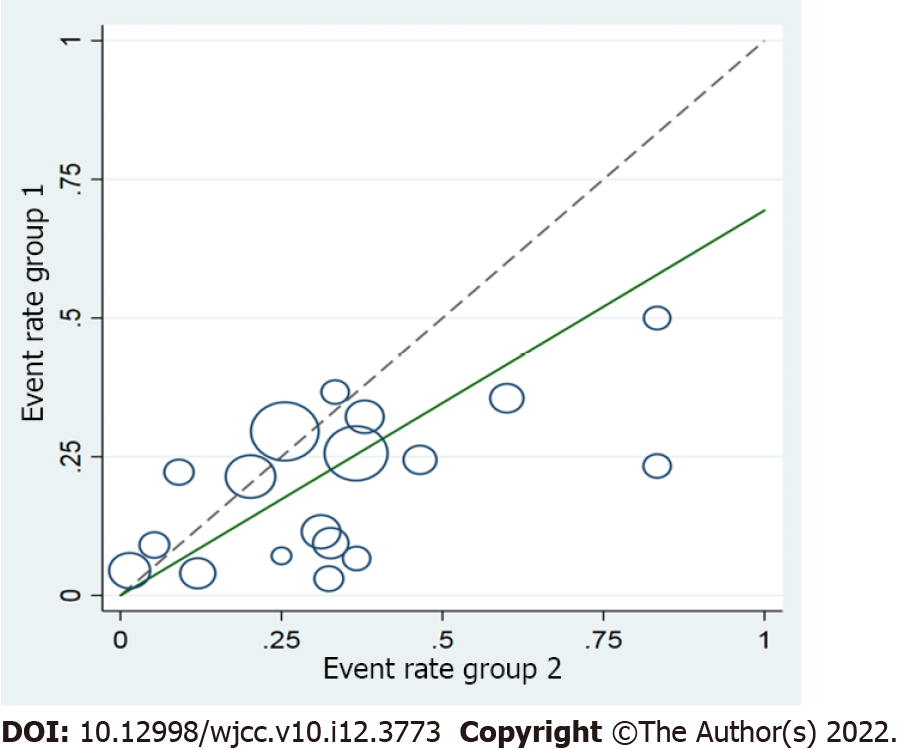
The 18 documents in this study were tested for heterogeneity, and it was found that I2 = 62% > 50%, and the Q test showed P = 0.0003 < 0.1, suggesting that the documents selected in this study were heterogeneous. Further investigation using Rabe diagrams and star diagrams indicated that there was a strong possibility of heterogeneity in the literature with regard to different patient types (Figures 5 and 6). Therefore, heterogeneity testing was required.
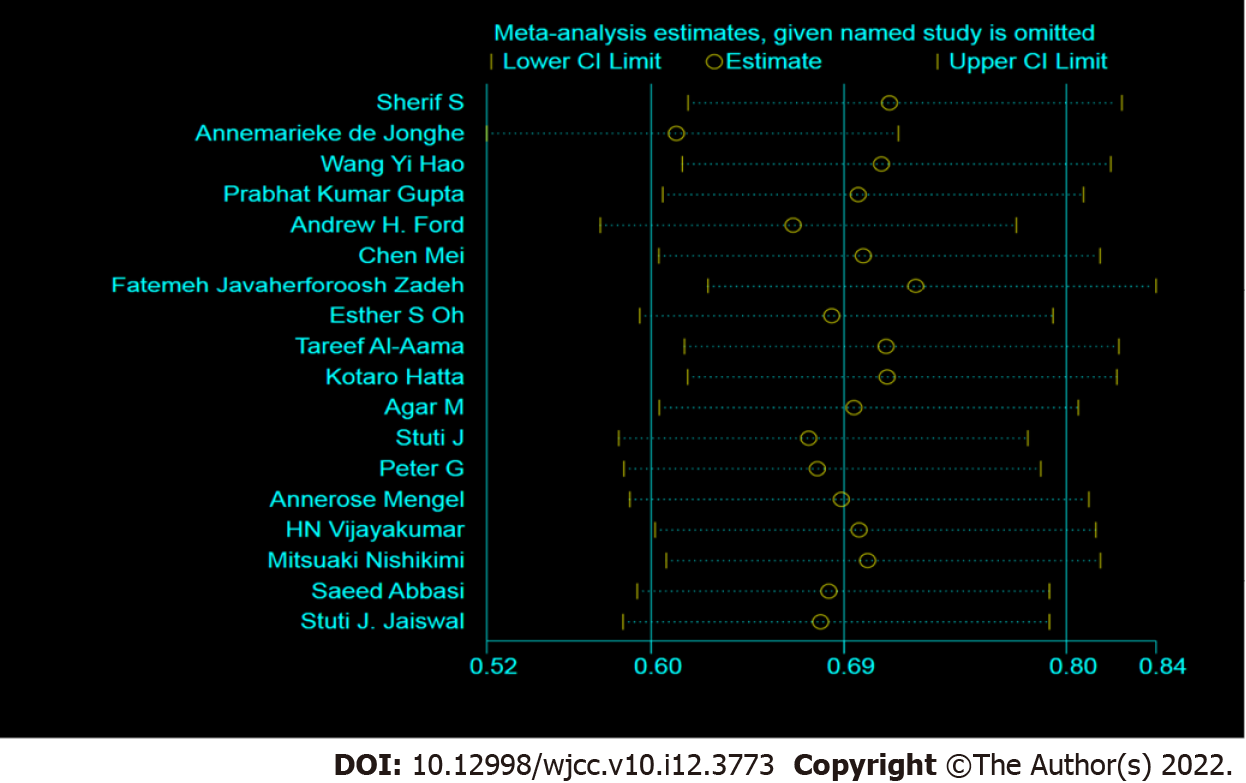
Sensitivity analysis is a method of testing the stability of results obtained under certain assumptions by changing some important factors that affect the combined results, such as inclusion criteria, literature evaluation, loss to follow-up, and different effect sizes, and then re-analyzing the data. The results before and after changing the conditions were compared, to judge the stability of the meta-analysis conclusions. A sensitivity analysis of the 18 articles found that different types of hospitalized patients had a greater impact on the heterogeneity, and it was necessary to further determine the source of heterogeneity (Figure 7).
Subgroup analysis is also a commonly used method to identify heterogeneity in a meta-analysis. It investigates the source of heterogeneity from the perspectives of clinical and methodological heterogeneity, and it can incorporate the issue of effect size by referring to homogeneity research. According to the characteristics that may cause heterogeneity, the different types of experimental patients were analyzed in subgroups. In terms of the grouping of patients, the patients were divided into three subgroups: inpatient surgical patients, inpatient medical patients, and inpatient ICU patients. This is shown in the Forest diagram. Both the surgical group and the internal medicine group demonstrated statistical significance (P < 0.05), but not the ICU group (P > 0.05). Sensitivity analysis was performed on the analysis results. Two effect models (fixed and random) were used. After each study was eliminated one by one, the meta-analysis was performed again. The results found that the surgical group had high heterogeneity, indicating that the source of heterogeneity was not the research literature. Considering that many factors cause delirium, it is not possible to blindly adopt the random effect model to merge the effect size; following exclusion of the article by Stuti[27] in the internal medicine group, the combined effect size of the meta-analysis changed markedly, indicating that the source of heterogeneity in the internal medicine group was due to Stuti J, suggesting that the results of this study were robust. Individual studies were excluded one by one following subgroup analysis, and the sensitivity analysis approach of analyzing the difference between the combined effect size and the total effect size of the remaining studies, also known as impact analysis, was used. Among hospitalized patients in internal medicine, the effect sizes after excluding studies one by one were all within the 95%CI value of the total effect size. Therefore, they had little effect on the total combined effect size and were acceptable. The original meta-analysis results were strengthened to make them more convincing.
In the groups of patient (surgery, internal medicine, ICU), their I2 were 75%, 45%, and 36%, respectively, indicating that there was no obvious heterogeneity in internal medicine patients in the subgroups; but if the three subgroups were combined, I2 was 61% indicating that there was heterogeneity, the intervention effect of melatonin in preventing delirium in different hospitalized patients was inconsistent, and the different types of hospitalized patients were the source of the heterogeneity. Melatonin had a stronger effect in reducing the incidence of delirium in hospitalized medical patients, according to subgroup analysis (P < 0.01) as shown in Figure 8. Therefore, Stuti's[27] article was eliminated. Following removal of this study, the heterogeneity test was performed again. The results showed that the remaining 6 documents did not demonstrate heterogeneity (I2 = 45% < 50%, P = 0.1). After elimination of this study, the fixed-effects model was used to combine the effect size.
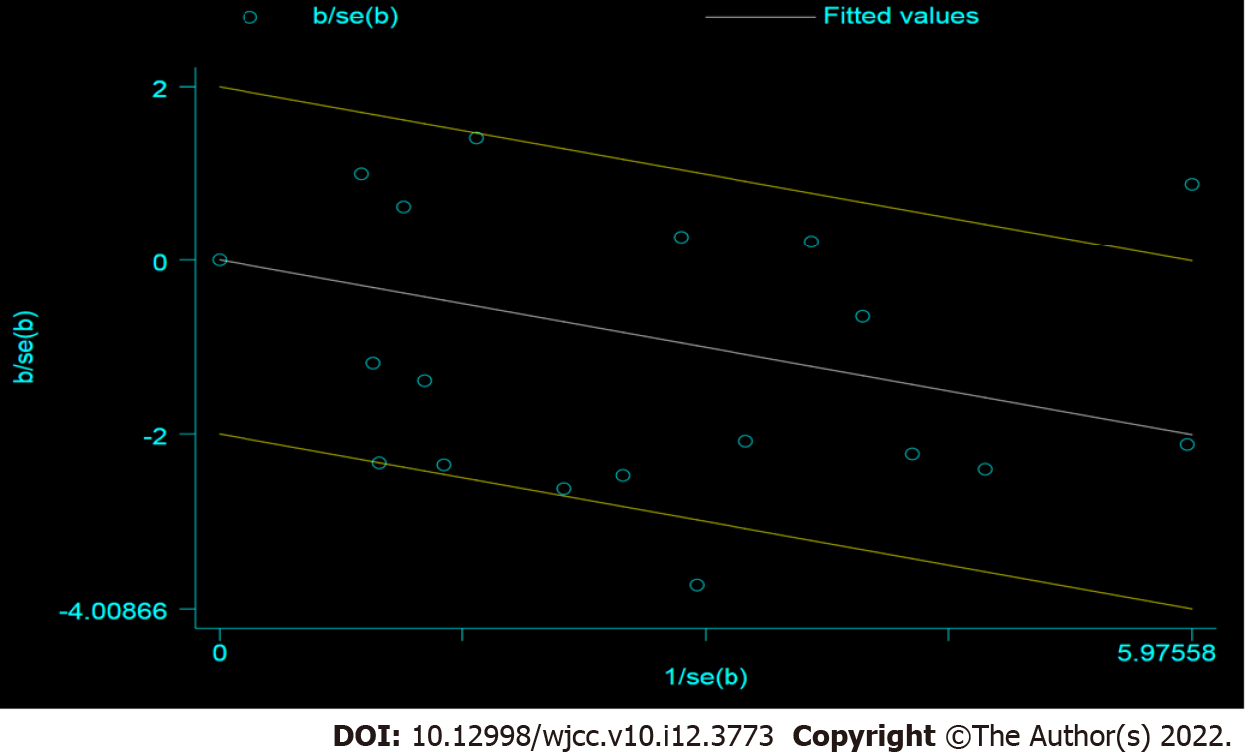
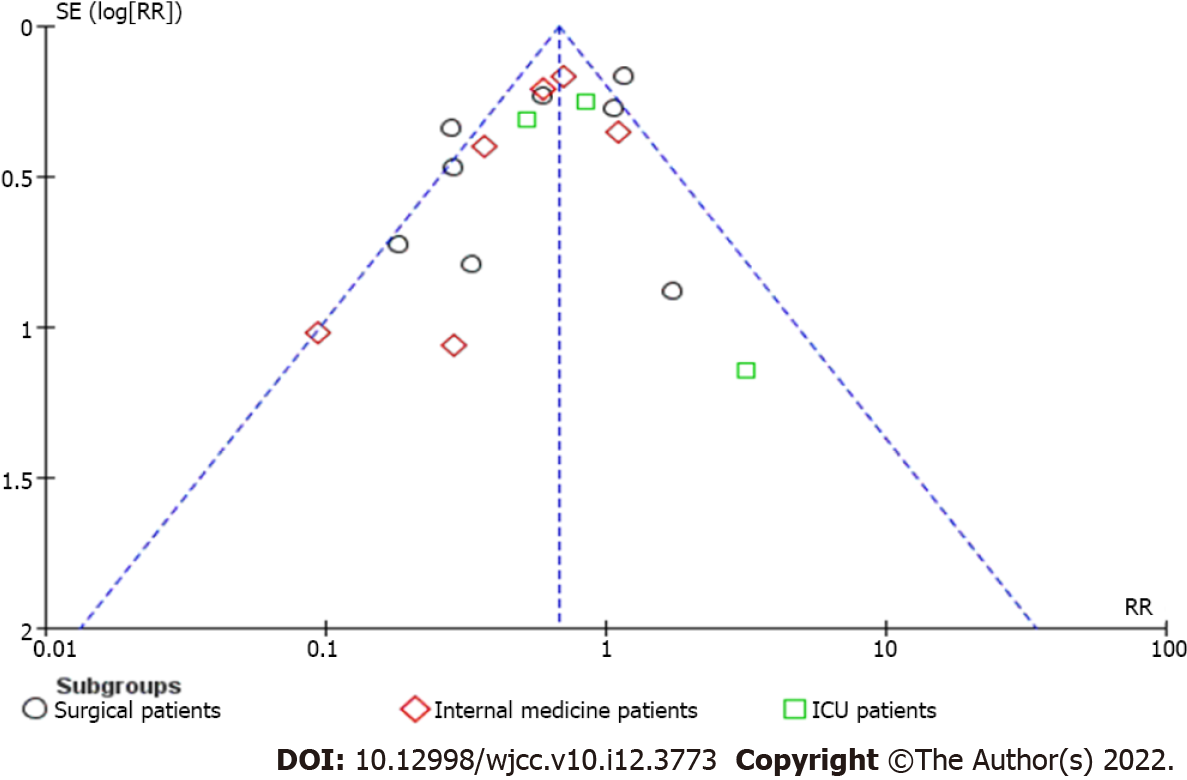
To determine whether there was publication bias in this study, a funnel chart was developed. The funnel chart for this study is shown in Figure 9. The funnel chart results of hospitalized patients in internal medicine showed a symmetrical distribution, suggesting that the publication bias of the included literature was small.
Delirium is characterized by dramatic changes in cognition, which are accompanied by changes in consciousness and in mental state, and these changes will fluctuate over time[34]. The incidence of delirium on admission is 11%-33%. The number of elderly patients in the emergency department, internal medicine, and surgery wards of general hospitals has increased by 6%[35-37].
In palliative care, the clinical management strategy for delirium episodes is to identify and treat correctable precipitating factors if they are consistent with the patient's desired treatment objectives; when the desired care goals are completely focused on comfort or delirium, the clinical management method is to identify and treat correctable precipitating factors. When episodes are difficult to treat, the therapeutic intervention must focus on symptomatic management of painful symptoms, such as perceptual disturbance or agitation. Antipsychotic drugs have been advocated for the first-line pharmacological treatment of painful delirium symptoms[38,39]. However, there is evidence that antipsychotic drugs have no preventive effect on delirium in hospitalized adults, and their therapeutic effects are limited[12,40,41]; in a recent trial of palliative care patients, antipsychotic drugs were less effective than placebo. Exacerbation of mild to moderate delirium can occur[42]. The proposed overall management approach is shifting to larger preventive measures, especially non-pharmacological interventions, and minimizing the use of antipsychotic drugs[43]. Multi-component non-pharmacological interventions, including maintenance of sleep hygiene, have significant effects in preventing delirium in the elderly[44,45], but in studies of palliative care populations, similar interventions plus suppressive therapy have not been effective in preventing delirium. Sleep-wake cycle disorder is not the core diagnostic criterion for the diagnosis of delirium, but it is reported that the prevalence of delirium in cancer patients is between 75% and 100%[46,47]. Although the pathophysiology of delirium is complex and not fully understood, melatonin disorders and related sleep-wake cycle disturbances are thought to be contributing factors to delirium. This is consistent with the initiation and maintenance of sleep; it plays an important role in the regulation and synchronization of the sleep-wake cycle and circadian rhythm[48]. According to reports, melatonin circadian rhythm disorders are found in postoperative patients and critically ill patients, especially in sepsis patients[49-51]. Melatonin disorders have therefore been confirmed in the majority of clinical patients with the highest risk of delirium, and this is the main hypothetical basis for the exogenous use of melatonin to prevent delirium. Postoperative delirium is closely related to postoperative cognitive dysfunction. In addition, postoperative delirium is considered to be a predictor of postoperative cognitive decline[52].
Although there is increasing attention on the effects of melatonin and melatonin receptor agonists in promoting sleep and preventing delirium in critically ill patients and other high-risk populations[53], the heterogeneity of melatonin supplementation to prevent delirium has ruled out broad concluding recommendations[54].
A total of 18 studies and 2137 patients were included in this systematic review and meta-analysis. The results of the study suggest that melatonin has a more significant effect in preventing delirium in hospitalized patients (P < 0.01), but no outstanding advantages have been observed in surgery and ICU patients, especially in surgical patients, although the effect was significant (P < 0.01). However, the heterogeneity in each study was strong. Melatonin cannot yet be considered effective in preventing delirium in surgical (post-surgery) patients; in ICU patients, the effectiveness of melatonin in preventing delirium in patients was not significant (P > 0.01), and there are currently few RCT-based studies on the effect of melatonin in the prevention of delirium in ICU patients. Multi-center, large-sample randomized controlled experimental data are still required to support these findings. Melatonin can be used to prevent delirium in hospitalized patients. However, it is unknown whether it is worthy of clinical recommendation, and the results of this study should be treated with caution.
This systematic study only retrieved publically available Chinese and English publications, and there are limitations in the retrieval of other languages and grey literature, which may cause certain publication bias. However, many predisposing factors of delirium were taken into account (for example, higher age, cognitive impairment, and dementia) and predisposing factors (for example, infections, drugs, and electrolyte disorders). Future studies should consider different subgroups of medical, surgical, and trauma patients, and patients with a higher incidence of delirium, such as the elderly, to evaluate which subgroup benefits most from exogenous melatonin supplementation. Larger RCTs should assess the possible differential melatonin effects in different patient subtypes to determine which subgroups of patients can benefit from melatonin to prevent delirium and which dose and duration of melatonin management are the most effective.
Melatonin may reduce the incidence of delirium in medical patients, but did not significantly reduce the occurrence of delirium in surgical and ICU patients.
From an evidence-based perspective, this study examined the influence of melatonin on the prevention of delirium in hospitalized patients. The results suggest that in patients with delusional behavior and dermatology ward (ICU) patients, the effect of melatonin on delirium was confirmed. Thus, melatonin may be a treatment option for delirium with careful design for different types of respondents, and more standardized options.
Recently, research on the effect of melatonin on the occurrence of delirium in hospitalized patients has attracted more and more attention. However, it is unknown whether melatonin can play a role in different types of hospitalized patients. The use of melatonin to prevent delirium has aroused increasing interest in doctors. However, whether melatonin can play a role in different types of hospitalized patients needs further research.
We conducted a meta-analysis, mainly for one purpose. It was based on high-quality studies with a large enough sample size to calculate a reliable estimate of the incidence of melatonin in preventing delirium in hospitalized patients, and to evaluate the role of melatonin in reducing the incidence of delirium in different types of patients.
Various databases were searched and relevant studies on the incidence of delirium treated with melatonin in hospitalized patients were retrieved. In our meta-analysis, fixed-effects and random-effects models were used to estimate the incidence of delirium in hospitalized patients. Publication and sensitivity bias analysis was used to test the robustness of the data.
A total of 18 studies involving 2137 patients were eligible for this review. Melatonin was shown to be more effective in reducing the incidence of delirium in hospitalized medical patients, and the findings were statistically significant (P < 0.01).
Melatonin can reduce the incidence of delirium in medical patients, but its impact on reducing the incidence of delirium in patients with behavioral disorders and ICU patients is unclear.
Our meta-analysis showed that melatonin can reduce the incidence of delirium in hospitalized medical patients. Unfortunately, limited research has shown that the benefit is not seen in surgical patients or ICU patients. Further study to determine the role of melatonin in reducing the incidence of delirium in surgical and ICU patients is required.
We would like to thank the doctors from the School of Public Health and Management and the Department of Biosensing, Chongqing Medical University for their help.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research, and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Byeon H, South Korea; Glumac S, Croatia S-Editor: Wu YXJ L-Editor: Webster JR P-Editor: Wu YXJ
| 1. | Gray SL, Lai KV, Larson EB. Drug-induced cognition disorders in the elderly: incidence, prevention and management. Drug Saf. 1999;21:101-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 117] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304:443-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1200] [Cited by in RCA: 1362] [Article Influence: 90.8] [Reference Citation Analysis (0)] |
| 3. | Baker KG. Evaluation of DSM-5 and IWG-2 criteria for the diagnosis of Alzheimer's disease and dementia with Lewy bodies. Diagnosis (Berl). 2016;3:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Breitbart W, Gibson C, Tremblay A. The delirium experience: delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics. 2002;43:183-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 412] [Cited by in RCA: 375] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 5. | Gagnon B, Lawlor PG, Mancini IL, Pereira JL, Hanson J, Bruera ED. The impact of delirium on the circadian distribution of breakthrough analgesia in advanced cancer patients. J Pain Symptom Manage. 2001;22:826-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Lawlor PG, Bush SH. Delirium in patients with cancer: assessment, impact, mechanisms and management. Nat Rev Clin Oncol. 2015;12:77-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Espino DV, Jules-Bradley AC, Johnston CL, Mouton CP. Diagnostic approach to the confused elderly patient. Am Fam Physician. 1998;57:1358-1366. [PubMed] |
| 8. | Parikh SS, Chung F. Postoperative delirium in the elderly. Anesth Analg. 1995;80:1223-1232. [DOI] [Full Text] |
| 9. | Carter GL, Dawson AH, Lopert R. Drug-induced delirium. Incidence, management and prevention. Drug Saf. 1996;15:291-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Inouye SK. The dilemma of delirium: clinical and research controversies regarding diagnosis and evaluation of delirium in hospitalized elderly medical patients. Am J Med. 1994;97:278-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 419] [Cited by in RCA: 386] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 11. | Neufeld KJ, Yue J, Robinson TN, Inouye SK, Needham DM. Antipsychotic Medication for Prevention and Treatment of Delirium in Hospitalized Adults: A Systematic Review and Meta-Analysis. J Am Geriatr Soc. 2016;64:705-714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 364] [Cited by in RCA: 272] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 12. | Caumo W, Torres F, Moreira NL Jr, Auzani JA, Monteiro CA, Londero G, Ribeiro DF, Hidalgo MP. The clinical impact of preoperative melatonin on postoperative outcomes in patients undergoing abdominal hysterectomy. Anesth Analg. 2007;105:1263-1271, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Tordjman S, Chokron S, Delorme R, Charrier A, Bellissant E, Jaafari N, Fougerou C. Melatonin: Pharmacology, Functions and Therapeutic Benefits. Curr Neuropharmacol. 2017;15:434-443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 420] [Cited by in RCA: 506] [Article Influence: 63.3] [Reference Citation Analysis (0)] |
| 14. | Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113:941-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3380] [Cited by in RCA: 3479] [Article Influence: 99.4] [Reference Citation Analysis (0)] |
| 15. | Ryan K, Leonard M, Guerin S, Donnelly S, Conroy M, Meagher D. Validation of the confusion assessment method in the palliative care setting. Palliat Med. 2009;23:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Sultan SS. Assessment of role of perioperative melatonin in prevention and treatment of postoperative delirium after hip arthroplasty under spinal anesthesia in the elderly. Saudi J Anaesth. 2010;4:169-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 138] [Cited by in RCA: 137] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 17. | de Jonghe A, van Munster BC, Goslings JC, Kloen P, van Rees C, Wolvius R, van Velde R, Levi M, de Haan RJ, de Rooij SE; Amsterdam Delirium Study Group. Effect of melatonin on incidence of delirium among patients with hip fracture: a multicentre, double-blind randomized controlled trial. CMAJ. 2014;186:E547-E556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 122] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 18. | Wang YH. Effect of exogenous melatonin intervention on postoperative delirium and serum S100 in elderly patients β The impact of. Dalian Yike Daxue Zazhi. 2018;6:533-536. [DOI] [Full Text] |
| 19. | Prabhat K. The Effect of Ramelteon on Postoperative Delirium in Elderly Patients: A Randomised Double-Blind Study. J Clin Diag Res. 2019;12:17-20. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Ford AH, Flicker L, Passage J, Wibrow B, Anstey M, Edwards M, Almeida OP. The Healthy Heart-Mind trial: melatonin for prevention of delirium following cardiac surgery: study protocol for a randomized controlled trial. Trials. 2016;17:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Chen M. Effect of melatonin on prevention of postoperative delirium in elderly patients with major abdominal surgery. Guangdong Yike Daxue Xuebao. 2020;2:230-233. |
| 22. | Javaherforoosh Zadeh F, Janatmakan F, Shafaeebejestan E, Jorairahmadi S. Effect of Melatonin on Delirium After on-Pump Coronary Artery Bypass Graft Surgery: A Randomized Clinical Trial. Iran J Med Sci. 2021;46:120-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 23. | Oh ES, Leoutsakos JM, Rosenberg PB, Pletnikova AM, Khanuja HS, Sterling RS, Oni JK, Sieber FE, Fedarko NS, Akhlaghi N, Neufeld KJ. Effects of Ramelteon on the Prevention of Postoperative Delirium in Older Patients Undergoing Orthopedic Surgery: The RECOVER Randomized Controlled Trial. Am J Geriatr Psychiatry. 2021;29:90-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 24. | Al-Aama T, Brymer C, Gutmanis I, Woolmore-Goodwin SM, Esbaugh J, Dasgupta M. Melatonin decreases delirium in elderly patients: a randomized, placebo-controlled trial. Int J Geriatr Psychiatry. 2011;26:687-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 194] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 25. | Hatta K, Kishi Y, Wada K, Takeuchi T, Odawara T, Usui C, Nakamura H; DELIRIA-J Group. Preventive effects of ramelteon on delirium: a randomized placebo-controlled trial. JAMA Psychiatry. 2014;71:397-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 238] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 26. | Agar M. Randomised double blind placebo controlled phase ii trial of prolonged release melatonin for prevention of delirium in inpatients with advancedcancer. Palliativemedicine. 2016;6:NP20160611-NP20160612. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Jaiswal SJ, McCarthy TJ, Wineinger NE, Kang DY, Song J, Garcia S, van Niekerk CJ, Lu CY, Loeks M, Owens RL. Melatonin and Sleep in Preventing Hospitalized Delirium: A Randomized Clinical Trial. Am J Med. 2018;131:1110-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 28. | Lawlor PG, McNamara-Kilian MT, MacDonald AR, Momoli F, Tierney S, Lacaze-Masmonteil N, Dasgupta M, Agar M, Pereira JL, Currow DC, Bush SH. Melatonin to prevent delirium in patients with advanced cancer: a double blind, parallel, randomized, controlled, feasibility trial. BMC Palliat Care. 2020;19:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Mengel A, Zurloh J, Boßelmann C, Brendel B, Stadler V, Sartor-Pfeiffer J, Meisel A, Fleischmann R, Ziemann U, Poli S, Stefanou MI. Delirium REduction after administration of melatonin in acute ischemic stroke (DREAMS): A propensity score-matched analysis. Eur J Neurol. 2021;28:1958-1966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 30. | Vijayakumar HN, Ramya K, Duggappa DR, Gowda KV, Sudheesh K, Nethra SS, Raghavendra Rao RS. Effect of melatonin on duration of delirium in organophosphorus compound poisoning patients: A double-blind randomised placebo controlled trial. Indian J Anaesth. 2016;60:814-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 31. | Nishikimi M, Numaguchi A, Takahashi K, Miyagawa Y, Matsui K, Higashi M, Makishi G, Matsui S, Matsuda N. Effect of Administration of Ramelteon, a Melatonin Receptor Agonist, on the Duration of Stay in the ICU: A Single-Center Randomized Placebo-Controlled Trial. Crit Care Med. 2018;46:1099-1105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 32. | Abbasi S, Farsaei S, Ghasemi D, Mansourian M. Potential Role of Exogenous Melatonin Supplement in Delirium Prevention in Critically Ill Patients: A Double-Blind Randomized Pilot Study. Iran J Pharm Res. 2018;17:1571-1580. [PubMed] |
| 33. | Jaiswal SJ, Vyas AD, Heisel AJ, Ackula H, Aggarwal A, Kim NH, Kerr KM, Madani M, Pretorius V, Auger WR, Fernandes TM, Malhotra A, Owens RL. Ramelteon for Prevention of Postoperative Delirium: A Randomized Controlled Trial in Patients Undergoing Elective Pulmonary Thromboendarterectomy. Crit Care Med. 2019;47:1751-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 49] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 34. | Trull TJ, Vergés A, Wood PK, Jahng S, Sher KJ. The structure of Diagnostic and Statistical Manual of Mental Disorders (4th edition, text revision) personality disorder symptoms in a large national sample. Personal Disord. 2012;3:355-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Bucht G, Gustafson Y, Sandberg O. Epidemiology of delirium. Dement Geriatr Cogn Disord. 1999;10:315-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 77] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 36. | Inouye SK. Deliriuminolder persons. N Engl J Med. 2006;354:1157-1165. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 37. | Michaud L, Büla C, Berney A. Delirium Guidelines Development Group. Delirium: guidelines for general hospitals. J Psychosom Res. 2007;62:371-383. |
| 38. | Breitbart W, Alici Y. Evidence-based treatment of delirium in patients with cancer. J Clin Oncol. 2012;30:1206-1214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 100] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 39. | Irwin SA, Pirrello RD, Hirst JM, Buckholz GT, Ferris FD. Clarifying delirium management: practical, evidenced-based, expert recommendations for clinical practice. J Palliat Med. 2013;16:423-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 40. | Burry L, Mehta S, Perreault MM, Luxenberg JS, Siddiqi N, Hutton B, Fergusson DA, Bell C, Rose L. Antipsychotics for treatment of delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev. 2018;6:CD005594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 65] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 41. | Finucane AM, Jones L, Leurent B, Sampson EL, Stone P, Tookman A, Candy B. Drug therapy for delirium in terminally ill adults. Cochrane Database Syst Rev. 2020;1:CD004770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 42. | Agar MR, Lawlor PG, Quinn S, Draper B, Caplan GA, Rowett D, Sanderson C, Hardy J, Le B, Eckermann S, McCaffrey N, Devilee L, Fazekas B, Hill M, Currow DC. Efficacy of Oral Risperidone, Haloperidol, or Placebo for Symptoms of Delirium Among Patients in Palliative Care: A Randomized Clinical Trial. JAMA Intern Med. 2017;177:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 218] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 43. | Bush SH, Lawlor PG, Ryan K, Centeno C, Lucchesi M, Kanji S, Siddiqi N, Morandi A, Davis DHJ, Laurent M, Schofield N, Barallat E, Ripamonti CI; ESMO Guidelines Committee. Delirium in adult cancer patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2018;29 Suppl 4:iv143-iv165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 44. | Martinez F, Tobar C, Hill N. Preventing delirium: should non-pharmacological, multicomponent interventions be used? Age Ageing. 2015;44:196-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 118] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 45. |
Gagnon P, Allard P, Gagnon B, Mérette C, Tardif F.
Delirium prevention in terminal cancer: assessment of a multicomponent intervention |
| 46. | Bosisio M, Caraceni A, Grassi L; Italian Delirium Study Group. Phenomenology of delirium in cancer patients, as described by the Memorial Delirium Assessment Scale (MDAS) and the Delirium Rating Scale (DRS). Psychosomatics. 2006;47:471-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 47. | Meagher DJ, Moran M, Raju B, Gibbons D, Donnelly S, Saunders J, Trzepacz PT. Phenomenology of delirium. Assessment of 100 adult cases using standardised measures. Br J Psychiatry. 2007;190:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 187] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 48. | Cipolla-Neto J, Amaral FGD. Melatonin as a Hormone: New Physiological and Clinical Insights. Endocr Rev. 2018;39:990-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 364] [Article Influence: 52.0] [Reference Citation Analysis (0)] |
| 49. | Perras B, Kurowski V, Dodt C. Nocturnal melatonin concentration is correlated with illness severity in patients with septic disease. Intensive Care Med. 2006;32:624-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 50. | Seifman MA, Gomes K, Nguyen PN, Bailey M, Rosenfeld JV, Cooper DJ, Morganti-Kossmann MC. Measurement of serum melatonin in intensive care unit patients: changes in traumatic brain injury, trauma, and medical conditions. Front Neurol. 2014;5:237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 51. | Yoshitaka S, Egi M, Morimatsu H, Kanazawa T, Toda Y, Morita K. Perioperative plasma melatonin concentration in postoperative critically ill patients: its association with delirium. J Crit Care. 2013;28:236-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 52. | Glumac S, Kardum G, Karanovic N. Postoperative Cognitive Decline After Cardiac Surgery: A Narrative Review of Current Knowledge in 2019. Med Sci Monit. 2019;25:3262-3270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 53. | Mo Y, Scheer CE, Abdallah GT. Emerging Role of Melatonin and Melatonin Receptor Agonists in Sleep and Delirium in Intensive Care Unit Patients. J Intensive Care Med. 2016;31:451-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 54. | Choy SW, Yeoh AC, Lee ZZ, Srikanth V, Moran C. Melatonin and the Prevention and Management of Delirium: A Scoping Study. Front Med (Lausanne). 2017;4:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |