Published online Apr 26, 2022. doi: 10.12998/wjcc.v10.i12.3720
Peer-review started: October 28, 2021
First decision: February 14, 2022
Revised: February 22, 2022
Accepted: March 25, 2022
Article in press: March 25, 2022
Published online: April 26, 2022
Processing time: 174 Days and 19.1 Hours
By analyzing the risk factors of postoperative complications in elderly patients with hip replacement, We aimed to develop a nomogram model based on preoperative and intraoperative variables and verified the sensitivity and specificity for risk stratification of postoperative complications in elderly with total hip replacement patients.
To develop a nomogram model for risk stratification of postoperative complications in elderly with total hip replacement patients.
A total of 414 elderly patients who underwent surgical treatment for total hip replacement hospitalized at the Affiliated Hospital of Guangdong Medical University from March 1, 2017 to August 31, 2019 were included into this study. Univariate and multivariate logistic regression were conducted to identify independent risk factors of postoperative complication in the 414 patients. A nomogram was developed by R software and validated to predict the risk of postoperative complications.
Multivariate logistic regression analysis revealed that age (OR = 1.05, 95%CI: 1.00-1.09), renal failure (OR = 0.90, 95%CI: 0.83-0.97), Type 2 diabetes (OR = 1.05, 95%CI: 1.00-1.09), albumin (ALB) (OR = 0.91, 95%CI: 0.83-0.99) were independent risk factors of postoperative complication in elderly patients with hip replacement (P < 0.05). For validation of the nomogram, receive operating characteristic curve revealed that the model predicting postoperative complication in elderly patients with hip replacement was the area under the curve of 0.8254 (95%CI: 0.78-0.87), the slope of the calibration plot was close to 1 and the model passed Hosmer-Lemeshow goodness of fit test (χ2 = 10.16, P = 0.4264), calibration in R Emax = 0.176, Eavg = 0.027, which all demonstrated that the model was of good accuracy.
The nomogram predicting postoperative complications in patients with total hip replacement constructed based on age, type 2 diabetes, renal failure and ALB is of good discrimination and accuracy, which was of clinical significance.
Core Tip: Predictive models refer to the use of multivariate methods in the design and analysis of prognostic studies to identify important predictors of outcomes and to provide a combination of outcome probabilities or tools for estimating such probabilities. Predictive models can be used in a variety of medical settings, primarily to predict the course (or risk) of an individual disease, and to guide doctors and patients in deciding together on further treatment. This study aims to establish prediction model of postoperative complications in elderly patients with total hip replacement is use individualized treatment to assist complex decision-making.
- Citation: Tan XJ, Gu XX, Ge FM, Li ZY, Zhang LQ. Nomogram to predict postoperative complications in elderly with total hip replacement. World J Clin Cases 2022; 10(12): 3720-3728
- URL: https://www.wjgnet.com/2307-8960/full/v10/i12/3720.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i12.3720
Hip replacement is a frequently done and highly successful surgical intervention[1]. More than one million hip arthroplasties are performed annually worldwide[2]. Kurtz et al[3] projected the demand for primary total hip arthroplasty (THA) to grow 174% to 572000 procedures per year by 2030. These procedures carry a complication rate estimated to be between 2% and 14%; higher complication rates are associated with more elderly and comorbid patient populations[4]. Numerous clinical tools have been developed to predict a variety of THA patient outcomes[5-7], but the risk calculator to be a poor predictor of postoperative complications in Chinese. This is likely due to the complexity of the environment, race and personal differences. As an anesthetist, when we go to the inpatient ward for preoperative evaluation, patient often ask: what is the proportion of risk in my surgery? The answer is perhaps or we don’t know. So we want to create a tool not only can predict the risk precisely, but also guide the clinical work. Therefore this study will analyze clinical data, explored the independent risk factors for postoperative complications in elderly patients undergoing total hip replacement, develop a nomogram for accurate risk stratification of postoperative complications based on preoperative and intraoperative variables, and verify whether this tool would have good predictive for patients undergoing total hip replacement in our hospital.
Approved by the Ethics Committee of the Affiliated Hospital of Guangdong Medical University committee (PJ2020-022), we were collected from all patients undergoing total hip replacement from March 1, 2017 to August 31, 2019 at the Affiliated Hospital of Guangdong Medical University. Inclusion criteria were age > 65 years, elective surgical treatment with total hip replacement. Non-inclusion criteria were age < 65 years, electronic medical records incomplete, patients or family members disagree with the study.
Data on general patient information, comorbidities, laboratory test results, intraoperative variables, and postoperative complications during hospitalization were collected from electronic medical records and electronic Anesthesia Information Management System. Known patient-related factors of complications are age, gender, fractures or not and comorbidity such as renal failure, hypertension, diabetes, coronary heart disease, stroke, laboratory test results of white blood cells, red blood cells, hemoglobin, platelets, albumin (ALB) and blood urea nitrogen. Intraoperative variables included estimated blood loss, lowest heart rate, the type of anesthesia, preoperative American Society of Anesthesiologists Score and operation time.
The primary outcome measure was the incidence of a postoperative complication or death during hospitalization. Complications were identified from diagnoses in discharge summaries, operative reports, and International Classification of Diseases-9 codes by a single investigator. Included: cardiac arrest, deep venous thrombosis, myocardial infarction, pneumonia, pulmonary embolism, systemic inflammatory response syndrome, infection, dislocation, delirium, according to definitions from the National Quality Improvement Project[8].
All statistical analyses were performed using the STATA14.0 statistical software package and R software (R3.2.3) with rms package added. Differences between patients with and without complications were compared with t-test or Wilcoxon rank-sum test using the mean ± SD and the median (range) for quantitative variables and chi-squared test using n (%) for qualitative variables. Univariate logistic regression for patients clinical data were analyzed to identify the independent risk factors for postoperative complications after surgery. A multivariate logistic regression model was built using the factors associated with P values < 0.05 by univariate analysis. Selection values of P < 0.05 variables by multivariate analysis to create a nomogram model by R software (R3.2.3) rms package, evaluated the nomogram by assessing discrimination and calibration.
In our study 414 elderly total hip replacement patients of 59 cases with postoperative complications after surgery, the incidence was 14.3%. The demographics and descriptive statistics for our patient cohort are given in Table 1. Multivariable logistic regression of each clinical variable of patients related factors for postoperative complications include patients age (OR = 1.05, 95%CI: 1.00-1.09), renal failure (OR = 0.90, 95%CI: 0.83-0.97), diabetes (OR = 2.37, 95%CI: 1.04-5.40) and ALB (OR = 0.91, 95%CI: 0.83-0.99) (Table 2).
| Patient characteristics | No complications (n = 355) | Complications (n = 59) | t/χ2/Z value | P value |
| Age (yr)1 | 74.06 ± 7.25 | 81.29 ± 8.19 | 6.96 | 0.000 |
| Male gender (%)2 | 149 (41.9) | 24(40.7) | 0.03 | 0.852 |
| Weight (kg)1 | 58.93 ± 10.23 | 57.2 ± 9.93 | 1.2 | 0.226 |
| Comorbidities | ||||
| Hypertension (%)2 | 114 (32.1) | 30 (50.8) | 7.83 | 0.006 |
| Diabetes (%)2 | 50 (14.1) | 16 (27.1) | 6.41 | 0.017 |
| Coronary heart disease (%)2 | 30 (5) | 10 (16.9) | 4.19 | 0.041 |
| Stroke (%)2 | 16 (4.5) | 12 (20.3) | 20.11 | 0.000 |
| Renal failure (%)2 | 13 (3.7) | 7 (11.9) | 7.404 | 0.017 |
| Fractures (%)2 | 123 (34.6) | 45 (76.3) | 36.35 | 0.000 |
| Laboratory data | ||||
| WBC (109/L)1 | 7.6 ± 2.46 | 8.69 ± 2.93 | 2.7 | 0.003 |
| RBC (1012/L)1 | 4.21 ± 0.59 | 3.89 ± 0.69 | 3.81 | 0.000 |
| Hb (g/L)1 | 123.37 ± 20.99 | 111.89 ± 22.64 | 3.85 | 0.000 |
| PLT (109/L)1 | 235.66 ± 71.56 | 247.91 ± 115.27 | 0.79 | 0.272 |
| ALB (g/L)1 | 39.37 ± 4.51 | 35.75 ± 4.41 | 5.72 | 0.000 |
| BUN (mmol/L)1 | 6.05 ± 4.02 | 7.71 ± 5.08 | 2.39 | 0.019 |
| Intraoperative characteristics | ||||
| EBL (mL)3 | 203.79 (50-1500) | 229.8 (50-1000) | 1.5 | 0.134 |
| Lowest heart rate (bpm)1 | 59.39 ± 10.49 | 65.37 ± 13.88 | 3.16 | 0.001 |
| Operation time (min)1 | 100.85 ± 40.26 | 89.41 ± 37.24 | 2.04 | 0.505 |
| General anesthesia (%)2 | 159 (44.8) | 24 (40.7) | 0.35 | 0.556 |
| ASA class ΙΙΙ or ΙV (%)2 | 159 (44.8) | 518 (86.4) | 39.35 | 0.000 |
| Variables | OR | SE | Z | 95%CI | P value |
| Age | 1.05 | 0.02 | 2.04 | 1.00-1.09 | 0.041 |
| Renal failure | 3.96 | 2.44 | 2.23 | 1.18-13.27 | 0.026 |
| Hypertension | 1.31 | 0.47 | 0.74 | 0.65-2.64 | 0.457 |
| Coronary heart disease | 0.84 | 0.41 | 0.36 | 0.32-2.18 | 0.722 |
| Diabetes | 2.37 | 1.00 | 2.05 | 1.04-5.40 | 0.040 |
| Stroke | 2.41 | 1.15 | 1.84 | 0.94-6.16 | 0.066 |
| Fractures | 2.21 | 0.95 | 1.86 | 0.96-5.12 | 0.063 |
| ASA class ΙΙΙ or ΙV | 1.85 | 0.68 | 1.69 | 0.91-3.79 | 0.090 |
| Lowest heart rate | 1.02 | 0.01 | 1.10 | 0.99-1.05 | 0.272 |
| RBC | 1.05 | 0.34 | 0.16 | 0.56-1.99 | 0.869 |
| WBC | 1.03 | 0.64 | 0.44 | 0.91-1.16 | 0.657 |
| Hb | 1.00 | 0.01 | 0.10 | 0.98-1.02 | 0.922 |
| ALB | 0.90 | 0.04 | 2.73 | 0.83-0.97 | 0.006 |
| BUN | 1.00 | 0.04 | 0.13 | 0.94-1.08 | 0.893 |
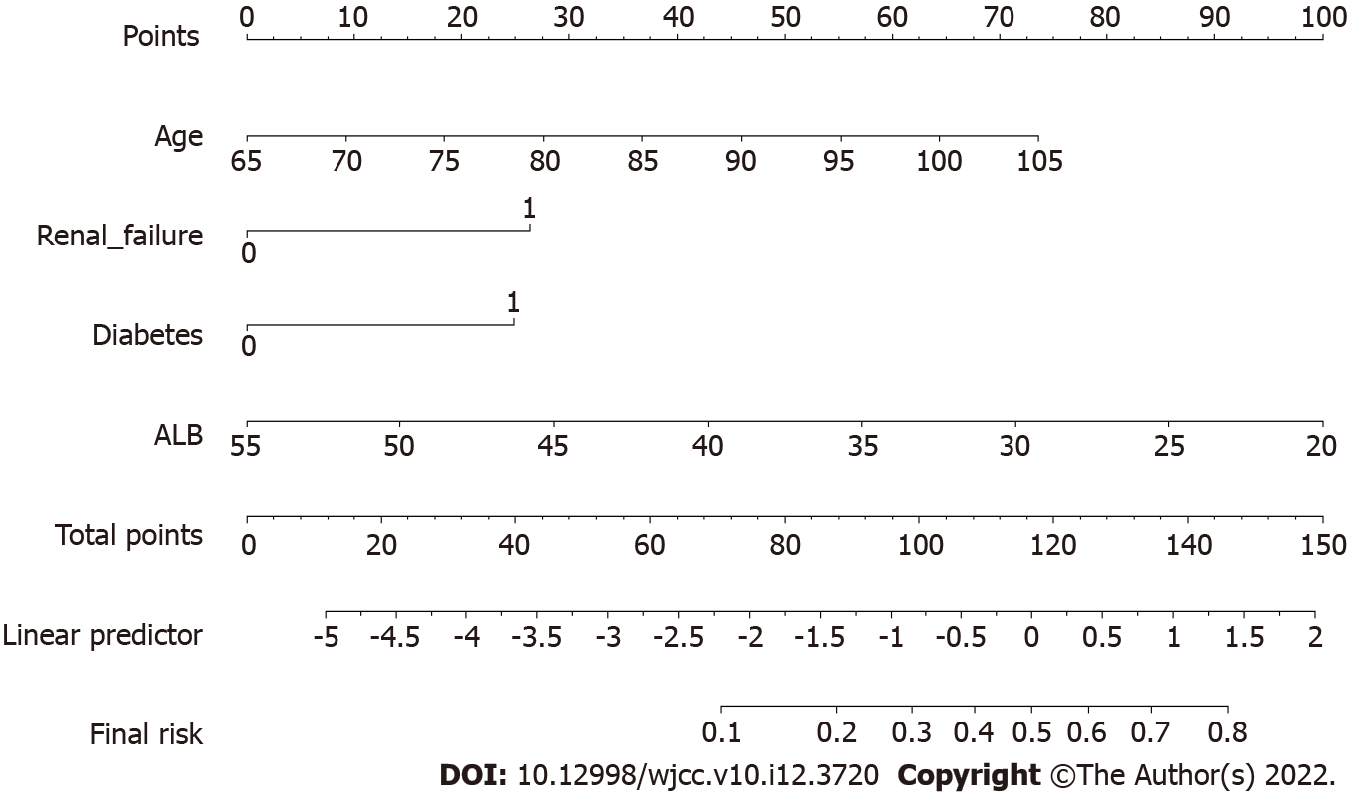
According to the above multivariable logistic regression analysis results, choose P < 0.05 variable apply R software to build a nomogram model of postoperative complications in elderly total hip replacement patients (Figure 1).
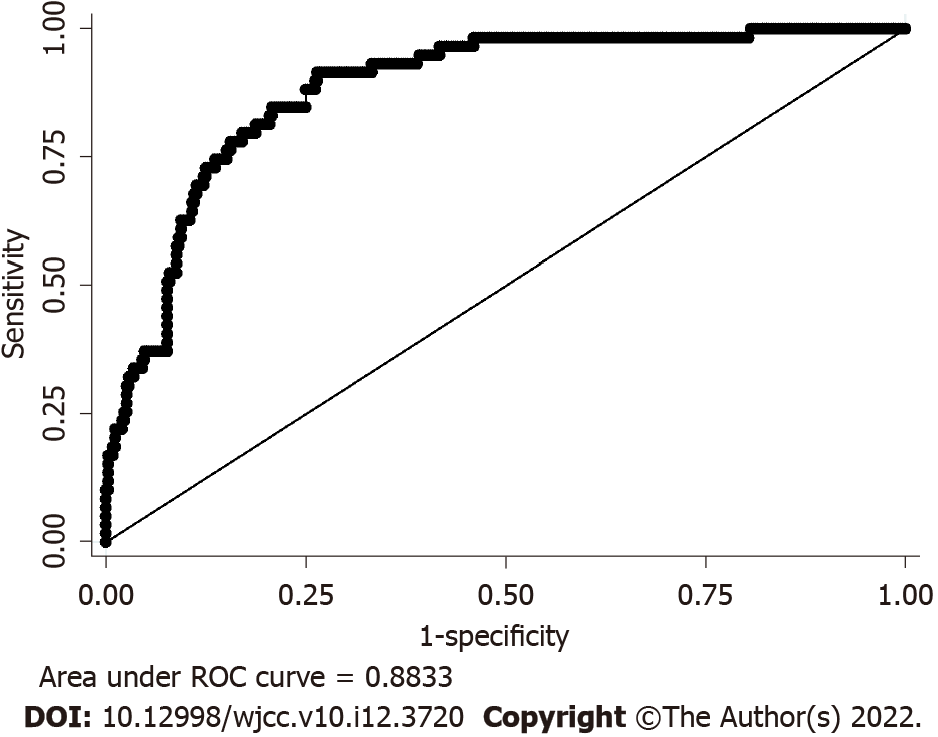
Using nomogram model to predict postoperative complications in elderly total hip replacement patients risk receive operating characteristic (ROC) curve, area under curve (AUC) is 0.8254 (95%CI: 0.78-0.87), indicating that the nomogram model has a good bootstrap-corrected concordance (Figure 2).
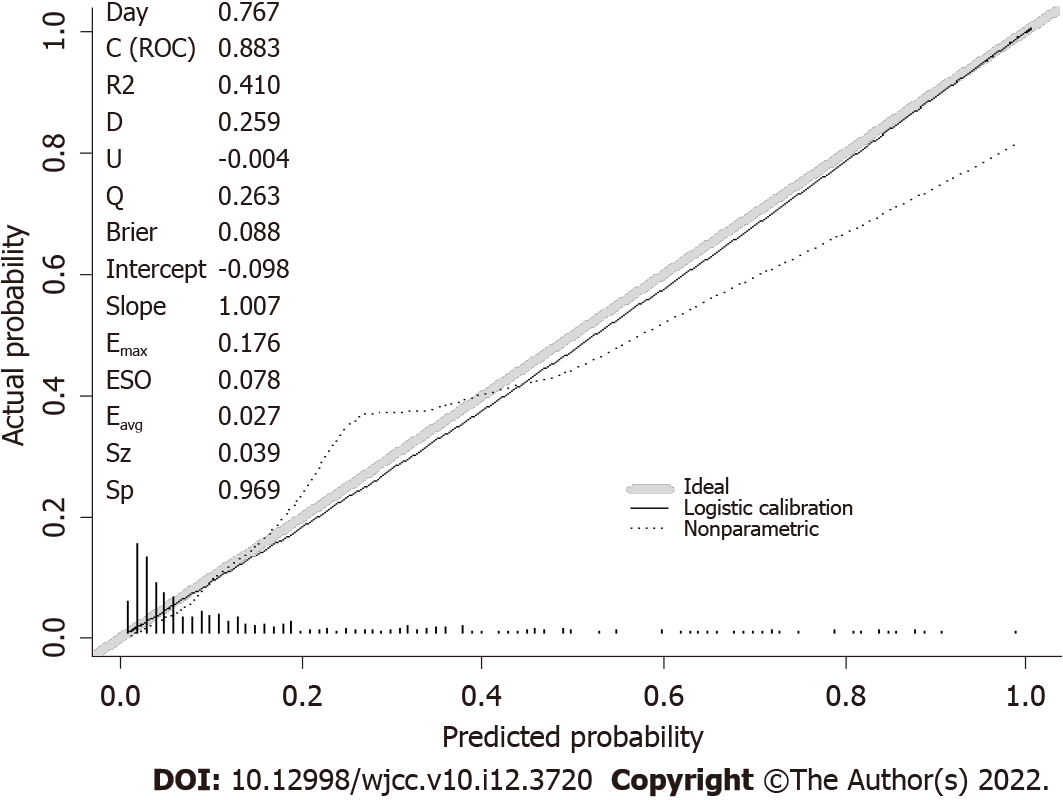
Perform Hosmer-Lemeshow goodness-of-fit test and evaluate nomogram Model accuracy, Hosmer-Lemeshow fit goodness test χ2 = 10.16, P = 0.4264 (Figure 3), calibration in rms package by R software Emax = 0.176, Eavg = 0.027 (Figure 4), all shows that the model appears to be well-calibrated, with predicted outcome rates closely reflecting the observed rates.
China is the most populated country in the world, and now has the second-largest economy in the world[9]. As nearly 166 million Chinese are aged more than 65 years[10]. The demand for healthcare, including hip arthroplasty is increasing[11,12]. There are several predict complications model have be reported[13-15], but on one is modeling by Chinese. In this study, 59 of the 414 elderly total hip replacement patients who underwent surgical treatment were developed postoperative complication, the incidence is 14.3%, morbidity is much higher than 3.9%[16]. Probably because our definition of complications not only included dislocation, pulmonary embolism, and infection as reported previously, but included systemic inflammatory response syndrome, delirium which are common in elderly. Among 566 older patients (mean age, 76.7 years) undergoing a variety of elective operations (including orthopedic, general, and vascular), 23.9% patients developed postoperative delirium[17]. The incidence of postoperative delirium was reported as 7.0%-30.2% in hip arthroplasty[18,19]. In this study the average age is 75.09 ± 7.8. As a result, the morbidity 14.3% is considered to be reasonable.
Age is a recognized risk factor for postoperative complications. The results of this study indicate that elderly patients with renal failure and diabetes are more likely to have postoperative complications after total hip replacement. It is Consistent with the research results of Merrill et al[20]. One possible reason is that elderly patients have more comorbidities will make them less able to withstand the stresses of anesthesia and surgery[21,22]. Diabetes have been reported to be significant predictors for complications such as surgical site infections[23]. The available data suggest that diabetes may promote the development of osteoarthritis[24]. Our results for the outcome measure indicate that elderly patients with renal failure and diabetes increase the weight of the nomogram model score by 25 points and 24 points, respectively.
Interestingly, our data suggest that low preoperative albumin levels can predict the incidence of postoperative complications following surgery for total hip replacement. The result is consistent with Kishawi et al[25]. Since ALB is a biomarker of visceral protein and immune-competence status, it is commonly used for nutritional assessment[26]. Preoperative albumin bears strong potential as a practical metric to assess a patient’s overall health[27]. Recent studies even show that low ALB rather reflects a state of persistent inflammation[28]. The perhaps reason for ALB as an independent predictor of major complications is that ALB recapitulates the physiological stress intensity triggered by surgery, which is determined by several factors, such as the invasiveness of surgery and its duration, as well as the intrinsic characteristics of the patient[29]. Our results pointed out that the weight of 12.7 points in the nomogram model score will be increased for every 5 g/L decrease in ALB. We recommend surgeons and anesthetists should ideally attempt to optimize patient nutritional status before total hip replacement in elderly in order to avoid a greater likelihood of postoperative complications or mortality.
However our study has several limitations. First, our data were limited only 414 patients, it only represents an elective patient population. Second, complications were only collected while in hospital, some of these complications could have occurred after discharge. Third, the predict model quality checks only with internal validation, so external validation will have to be included in future studies in order to promote use. Fourth, this was a retrospective study that relied on 9th edition coding, which can lead to errors and/or incomplete coding.
Risk calculators should serve as a tool to help clinical decision-making, promote individualized medicine, and aid in the shared decision-making process[30]. Many of the studies report poor discrimination and calibration of the investigated risk calculators. In our study, founded that age, diabetes, renal failure, and Albumin value are independent risk factors for postoperative complications in elderly patients with total hip replacement, ROC curve shows the AUC is 0.8254, indicating that the nomogram model has a good discrimination. The Hosmer-Lemeshow fit goodness test χ2 = 10.16, P = 0.4264 and calibration curve is a straight line with a slope close to 1, indicating that the nomogram model has good accuracy in predicting the risk of postoperative complications in elderly patients with total hip replacements surgery and has clinical application value.
This study created a nomogram model based on age, diabetes, renal failure, and albumin value independent risk factors for postoperative complications, has good indexing and accuracy can provide scientific guidance for individualized clinical prevention and treatment of postoperative complications in elderly patients with total hip replacements surgery in our hospital. This four variables are easy to get in clinical practice, has clinical application value especially for basic-level hospital.
As living standards and medical technology improve, the average lifespan and demand for medical care are gradually increasing, and the number of total hip replacements in elderly individuals is also increasing. Patients who undergo total hip replacement often experience trauma, pain, bleeding, and immobilization, leading to a cascade of inflammatory and metabolic processes that lead to severe postoperative complications. Numerous clinical tools have been developed to predict a variety of THA patient outcomes, but these risk calculators are poor predictors of postoperative complications in Chinese patients. The aim of this study was to analyse and assess postoperative complications and develop a nomogram model based on the related risk factors in elderly patients who underwent total hip replacement to guide surgeons and anaesthesiologists in developing strategies to minimize complications in elderly patients.
Develop a nomogram model to provide scientific guidance for the individualized prevention and treatment of postoperative complications in elderly patients who underwent total hip replacement.
To develop a nomogram model based on preoperative and intraoperative variables to predict postoperative complications in elderly patients who underwent total hip replacement.
We collected the clinical data of all patients who underwent total hip replacement from March 1, 2017 to August 31, 2019 at the Affiliated Hospital of Guangdong Medical University, including patient information, comorbidities, laboratory test results, intraoperative variables, and postoperative complications during hospitalization. The STATA 14.0 statistical software package and R software (R3.2.3) were used to develop a nomogram to predict the risk of postoperative complications in elderly patients who underwent total hip replacement surgery. The nomogram model can predict the risk of adverse clinical events individually by quantifying and visually displaying the results of the logistic regression.
Age, diabetes, renal failure, and albumin value were independent risk factors for postoperative complications in elderly patients who underwent total hip replacement surgery.
The nomogram model can integrate the related risk factors and predict the risk of adverse clinical events for individual patients and provide scientific guidance for the individualized clinical prevention and treatment of postoperative complications in elderly patients who underwent total hip replacement surgery.
We will increase the sample size used to construct the model, perform prolonged follow-up, and conduct a multicenter study in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ewers A, Austria; Ewers A, Austria; Hori T, Japan; Hori T, Japan S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Ferguson RJ, Palmer AJ, Taylor A, Porter ML, Malchau H, Glyn-Jones S. Hip replacement. Lancet. 2018;392:1662-1671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 382] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 2. | Pivec R, Johnson AJ, Mears SC, Mont MA. Hip arthroplasty. Lancet. 2012;380:1768-1777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 430] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 3. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3260] [Article Influence: 181.1] [Reference Citation Analysis (0)] |
| 4. | Nanjayan SK, Swamy GN, Yellu S, Yallappa S, Abuzakuk T, Straw R. In-hospital complications following primary total hip and knee arthroplasty in octogenarian and nonagenarian patients. J Orthop Traumatol. 2014;15:29-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Konopka JF, Hansen VJ, Rubash HE, Freiberg AA. Risk assessment tools used to predict outcomes of total hip and total knee arthroplasty. Orthop Clin North Am. 2015;46:351-362, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Schwartz PB, Stahl CC, Ethun C, Marka N, Poultsides GA, Roggin KK, Fields RC, Howard JH, Clarke CN, Votanopoulos KI, Cardona K, Abbott DE. Retroperitoneal sarcoma perioperative risk stratification: A United States Sarcoma Collaborative evaluation of the ACS-NSQIP risk calculator. J Surg Oncol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Lakomkin N, Lajam C, Holt GE, Hutzler L, Iorio R, Bosco JA III. The Utility of Preoperative Labs in Predicting Postoperative Complications Following Primary Total Hip and Knee Arthroplasty. Bull Hosp Jt Dis (2013). 2020;78:266-274. [PubMed] |
| 8. | Khuri SF, Daley J, Henderson W, Barbour G, Lowry P, Irvin G, Gibbs J, Grover F, Hammermeister K, Stremple JF. The National Veterans Administration Surgical Risk Study: risk adjustment for the comparative assessment of the quality of surgical care. J Am Coll Surg. 1995;180:519-531. [PubMed] |
| 9. | Open Knowledge Repository (OKR). World Bank Group. World Development Indicators 2017. [cited 2019 Jul 8]. Available from: https://openknowledge.worldbank.org/han-dle/10986/26447. |
| 10. | National Bureau of Statistics of China. China Statistics Press. China Statistical Yearbook 2017. [cited 2019 Jul 8]. Available from: http://www.stats.gov.cn/tjsj/ndsj/2019/indexeh.htm. |
| 11. | Wang K. Brief discussion on present status and future of joint replacement in China. Chin J Joint Surg. 2015;9:12-14. |
| 12. | Pei FX. The current status and future perspective of hip and knee arthroplasty in China. Chin J Bone Joint. 2012;1:4-8. |
| 13. | Wuerz TH, Kent DM, Malchau H, Rubash HE. A nomogram to predict major complications after hip and knee arthroplasty. J Arthroplasty. 2014;29:1457-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 14. | Wuerz TH, Regenbogen SE, Ehrenfeld JM, Malchau H, Rubash HE, Gawande AA, Kent DM. The Surgical Apgar Score in hip and knee arthroplasty. Clin Orthop Relat Res. 2011;469:1119-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Inneh IA, Lewis CG, Schutzer SF. Focused risk analysis: regression model based on 5,314 total hip and knee arthroplasty patients from a single institution. J Arthroplasty. 2014;29:2031-2035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Phillips CB, Barrett JA, Losina E, Mahomed NN, Lingard EA, Guadagnoli E, Baron JA, Harris WH, Poss R, Katz JN. Incidence rates of dislocation, pulmonary embolism, and deep infection during the first six months after elective total hip replacement. J Bone Joint Surg Am. 2003;85:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 346] [Cited by in RCA: 324] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 17. | Zenilman ME. Delirium: An Important Postoperative Complication. JAMA. 2017;317:77-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Chung KS, Lee JK, Park JS, Choi CH. Risk factors of delirium in patients undergoing total knee arthroplasty. Arch Gerontol Geriatr. 2015;60:443-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Scott JE, Mathias JL, Kneebone AC. Incidence of delirium following total joint replacement in older adults: a meta-analysis. Gen Hosp Psychiatry. 2015;37:223-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Merrill RK, Ibrahim JM, Machi AS, Raphael JS. Analysis and Review of Automated Risk Calculators Used to Predict Postoperative Complications After Orthopedic Surgery. Curr Rev Musculoskelet Med. 2020;13:298-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Monk TG, Saini V, Weldon BC, Sigl JC. Anesthetic management and one-year mortality after noncardiac surgery. Anesth Analg. 2005;100:4-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 634] [Cited by in RCA: 599] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 22. | Higuera CA, Elsharkawy K, Klika AK, Brocone M, Barsoum WK. 2010 Mid-America Orthopaedic Association Physician in Training Award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. 2011;469:1391-1400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 23. | Saucedo JM, Marecek GS, Wanke TR, Lee J, Stulberg SD, Puri L. Understanding readmission after primary total hip and knee arthroplasty: who's at risk? J Arthroplasty. 2014;29:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 137] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 24. | Illingworth KD, El Bitar YF, Banerjee D, Scaife SL, Saleh KJ. Inpatient mortality after primary total hip arthroplasty: analysis from the National Inpatient Sample database. J Arthroplasty. 2015;30:369-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Kishawi D, Schwarzman G, Mejia A, Hussain AK, Gonzalez MH. Low Preoperative Albumin Levels Predict Adverse Outcomes After Total Joint Arthroplasty. J Bone Joint Surg Am. 2020;102:889-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 26. | Seltzer MH, Bastidas JA, Cooper DM, Engler P, Slocum B, Fletcher HS. Instant nutritional assessment. JPEN J Parenter Enteral Nutr. 1979;3:157-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 112] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Gupta A, Upadhyaya S, Cha T, Schwab J, Bono C, Hershman S. Serum albumin levels predict which patients are at increased risk for complications following surgical management of acute osteoporotic vertebral compression fractures. Spine J. 2019;19:1796-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | de Mutsert R, Grootendorst DC, Indemans F, Boeschoten EW, Krediet RT, Dekker FW; Netherlands Cooperative Study on the Adequacy of Dialysis-II Study Group. Association between serum albumin and mortality in dialysis patients is partly explained by inflammation, and not by malnutrition. J Ren Nutr. 2009;19:127-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 178] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 29. | Labgaa I, Mantziari S, Genety M, Elliott JA, Kamiya S, Kalff MC, Winiker M, Pasquier J, Allemann P, Messier M, van Berge Henegouwen MI, Nilsson M, Reynolds JV, Piessen G, Hübner M, Demartines N, Schäfer M. Early postoperative decrease of albumin is an independent predictor of major complications after oncological esophagectomy: A multicenter study. J Surg Oncol. 2021;123:462-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 30. | Mansmann U, Rieger A, Strahwald B, Crispin A. Risk calculators-methods, development, implementation, and validation. Int J Colorectal Dis. 2016;31:1111-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |