Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3291
Peer-review started: November 15, 2021
First decision: December 27, 2021
Revised: January 8, 2022
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: April 6, 2022
Processing time: 133 Days and 21.2 Hours
A cervical aortic arch (CAA) refers to a high-riding aortic arch (AA) that often extends above the level of the clavicle. This condition is very rare, with an incidence of less than 1/10000.
A 29-year-old woman was admitted to the otolaryngology department of our hospital for repeated bilateral purulent nasal discharge for the prior 3 mo. The patient was diagnosed with chronic sinusitis and chronic rhinitis at admission. A preoperative noncontrast chest computed tomography scan showed a high-riding, tortuous AA extending to the mid-upper level of the first thoracic vertebra with local cystic dilatation. A further computed tomography angiography examination showed that the brachiocephalic trunk, left common carotid artery, left vertebral artery (LVA) (slender), and left subclavian artery sequentially branched off of the aorta from the proximal end to the distal end of the AA. The proximal end of the right subclavian artery (RSCA) was tortuous and dilated. The AA showed tumor-like local expansion, with a maximum diameter of approximately 4 cm. After consultation with the department of cardiac macrovascular surgery, the patient was diagnosed with left CAA with aneurysm formation and an anomalous RSCA and LVA and was transferred to that department. The patient underwent AA aneurysm resection and artificial blood vessel replacement under general anesthesia and cardiopulmonary bypass. No abnormality was found during the 2-mo follow-up after discharge.
A CAA is a rare congenital anomaly of vascular development. The present unique case of CAA with aneurysm formation and an anomalous RSCA and LVA enriches existing CAA data.
Core Tip: A cervical aortic arch (CAA) is a rare congenital anomaly of vascular development and refers to a high-riding aortic arch that often extends above the level of the clavicle. This paper reports a case of a unique CAA with aneurysm formation and an anomalous right subclavian artery and left vertebral artery. The present unique case enriches existing CAA data.
- Citation: Wu YK, Mao Q, Zhou MT, Liu N, Yu X, Peng JC, Tao YY, Gong XQ, Yang L, Zhang XM. Cervical aortic arch with aneurysm formation and an anomalous right subclavian artery and left vertebral artery: A case report. World J Clin Cases 2022; 10(10): 3291-3296
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3291.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3291
A cervical aortic arch (CAA) is a rare congenital anomaly of vascular development and refers to a high-riding aortic arch (AA) that often extends above the level of the clavicle[1-4]. This paper reports a case of a unique CAA with aneurysm formation and an anomalous right subclavian artery (RSCA) and left vertebral artery (LVA).
A 29-year-old woman presented repeated bilateral purulent nasal discharge for 3 mo.
The symptoms started 3 mo prior to presentation, with dizziness and headache.
The patient underwent a cesarean birth at a local hospital 4 years prior.
The patient had no family history that was related to the present illness.
Physical examination showed a slightly congested mucosa of the bilateral nasal cavity, a slightly enlarged inferior turbinate, a hypertrophic middle turbinate, and a small amount of purulent nasal discharge in both middle nasal passages and posterior nostrils.
Laboratory tests showed that the serum uric acid (428.9 μmol/L), fibrin (4.9 g/L), erythrocyte sedimentation rate (30 mm/h) and ultrasensitive thyroid stimulating hormone (5.1 μIU/mL) values were slightly elevated, the myoglobin (< 21 ng/mL) level was slightly decreased, and the complete blood count, electrolyte profiles and liver function were normal.
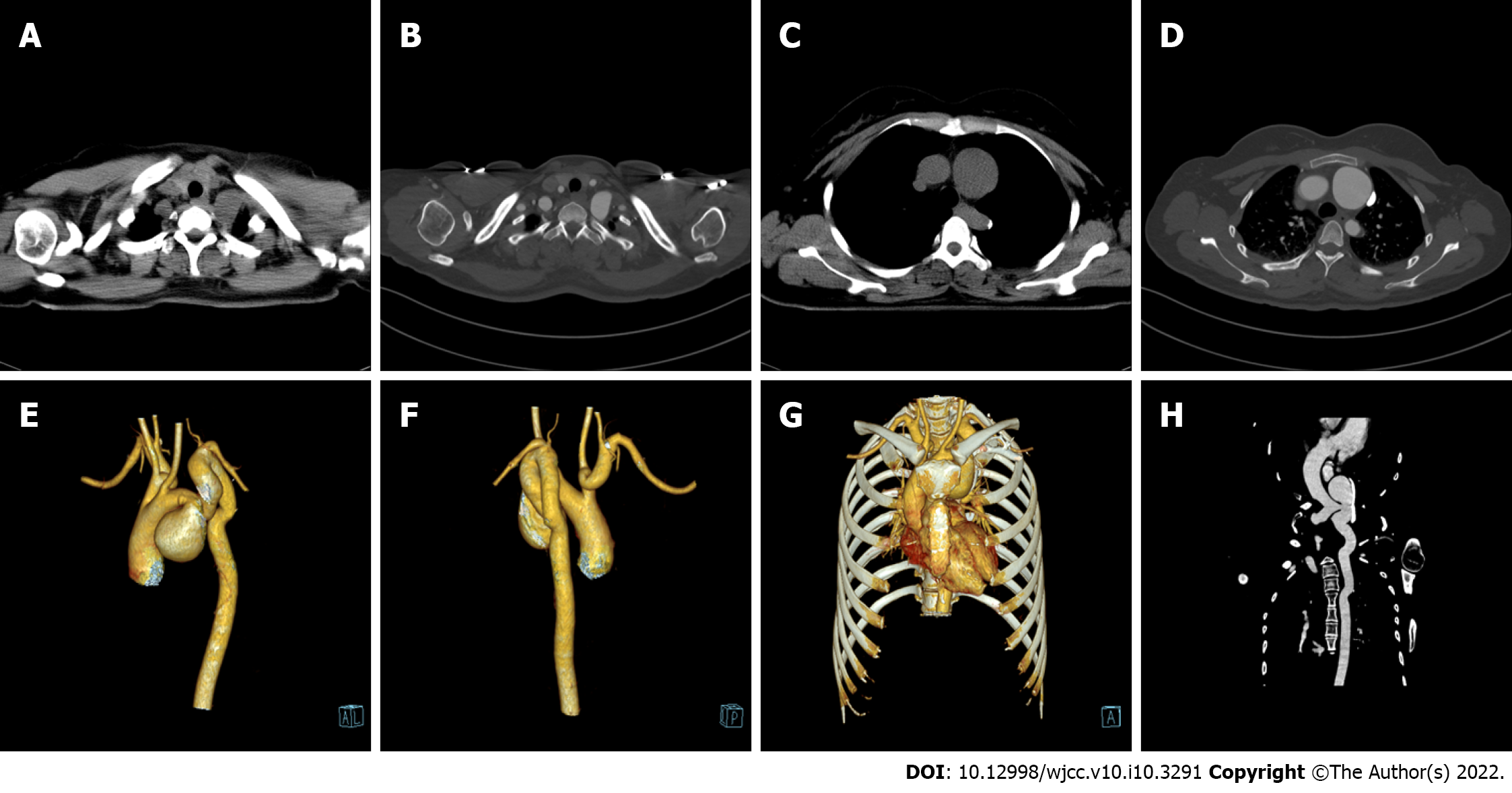
A computed tomography scan at another hospital showed bilateral maxillary sinusitis and ethmoiditis and bilateral inferior turbinate hypertrophy. The patient was diagnosed with chronic sinusitis and chronic rhinitis at admission. A preoperative noncontrast chest computed tomography scan showed a high-riding, tortuous AA extending to the mid-upper level of the first thoracic vertebra with local cystic dilatation, and a few calcified plaques were identified in the descending aorta (DA). A further computed tomography angiography examination showed that the ascending aorta was located to the right of the spine. The brachiocephalic trunk (BCT), left common carotid artery (LCCA), LVA (slender), and left subclavian artery (LSCA) sequentially branched off of the aorta from the proximal end to the distal end of the AA. The BCT bifurcated into the right common carotid artery and the RSCA. The proximal end of the RSCA was tortuous and dilated (approximately 1.5 cm in diameter). The AA showed tumor-like local expansion, with a maximum diameter of approximately 4.0 cm. The long and tortuous AA distal to the aneurysm was located to the left of the spine, extended upward, surpassed the level of the clavicle, and reached the mid-upper level of the first thoracic vertebra. Then, it extended downward tortuously along the left side of the spine to become the DA (Figure 1).
The final diagnosis of the present case was left CAA with aneurysm formation and an anomalous RSCA and LVA.
After consultation with the department of cardiac macrovascular surgery, the patient was diagnosed with left CAA plus aneurysm formation and an anomalous RSCA and LVA and was transferred to that department. The patient underwent AA aneurysm resection and artificial blood vessel replacement under general anesthesia and cardiopulmonary bypass (CPB) on July 10, 2021. The left CAA and the aneurysm (with a maximum diameter of approximately 4.0 cm) that had formed between the LCCA and the LSCA were observed during the operation. During the intraoperative period, a total of 2 units of type O suspended red blood cells, 10 units of cryoprecipitated antihemophilic factors, and 500 mL of fresh frozen plasma were transfused, and vasopressor drugs, including 8 µg deoxyepinephrine, 128 µg adrenaline, and 38478 µg dopamine, were infused with an infusion pump control to manage blood pressure. The total CPB time was 106 min, the ascending aorta was blocked for 44 min, and circulation was stopped for 15 min. After successful surgery, the patient received intensive care, anti-infection treatment, respiratory and circulatory function maintenance, and microcirculation improvement therapy for 44 h and 50 min.
The total hospital stay was 30 d. The patient’s recovery was smooth, and no abnormality was found at the 2-mo follow-up after discharge.
CAA was first reported by Reid[5] in 1914. CAA is very rare, with an incidence of less than 1/10000[1,3,6], although it is relatively more common in young women[6]. In the 35 cases of CAA reported by Zhong et al[6], the average patient age was 34.2 years, and females accounted for 65.7% of the sample.
The etiology of CAA is unclear but is possibly related to abnormal embryonic development of the AA (persistence of the 2nd or 3rd arch or incomplete descension of the normally developed fourth arch, resulting in incomplete entry of the AA into the thoracic cavity)[7-10]. Chromosome 22q11 deletion is evident in some CAA cases[3,4,11].
Most CAA cases are asymptomatic and are usually detected incidentally[4,6,12]. A few cases manifest as a pulsatile neck mass[4,6] or dyspnea and dysphagia due to compression of the trachea and esophagus[6,12,13]. Some CAA cases are combined with congenital cardiovascular anomalies, such as patent ductus arteriosus, tetralogy of Fallot, ventricular septal defect, pulmonary atresia[1,14], and various anatomical variations of the AA branches[2,3,13]. Approximately 20% of CAA cases are complicated with aneurysm formation[1,9,11], which is more common in women[8,9]. The aneurysm may be due to abnormal hemodynamics and arterial wall pressure changes caused by embryonic development, connective tissue anomalies, and a long and tortuous aorta[11,14]. Haughton et al[15] classified CAA into five types. Type A: The CAA and DA are contralateral, one side of the common carotid artery is missing, and the independent internal and external carotid arteries directly branch from the AA. Type B: The CAA and DA are contralateral, and two common carotid arteries branch from the AA. Type C: The CAA and DA are contralateral, and a bicarotid trunk appears. Type D: The CAA and DA are ipsilateral, and the sequence of brachiocephalic branching is normal. Type E: This type refers to a right CAA with an ipsilateral DA. Haughton et al[15] type D is the most common type of CAA that is combined with aneurysms[3,16], most aneurysms are located in the AA between the LCCA and the LSCA[6,8,16], but a few are located in the DA or simultaneously involve the AA and DA[16]. Shayan et al[11] reported eight cases of CAA with aneurysms (type D aneurysm in seven cases and type A aneurysm in one case), including six cases in which the aneurysm was located between the LCCA and the LSCA and two cases in which the aneurysm was located between the LSCA and the DA.
The patient described in this study had a left CAA with an ipsilateral DA. Her long and tortuous AA straddled the left side of the spine, extended upward above the clavicle, and then extended downward tortuously along the left side of the spine. The concurrent AA aneurysm was located between the LCCA and the ostium of the LSCA, and the origins of the two blood vessels were far apart. At the same time, the CAA was combined with the proximal dilatation and tortuosity of the RSCA and the anomalous origin of the LVA, reflecting the uniqueness of her manifestations.
A CAA is a rare congenital anomaly of vascular development. Some CAA cases are combined with congenital cardiovascular anomalies, and approximately 20% of CAA cases are complicated with aneurysm formation. The present unique case of CAA with aneurysm formation and an anomalous RSCA and LVA enriches existing CAA data.
We thank Mr. Yang F and Ms. Ma LJ for their contributions to computed tomography image reconstruction.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: The Chinese Society of Interventional Oncology.
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ozdemir HI, Schoenhagen P S-Editor: Guo XR L-Editor: A P-Editor: Guo XR
| 1. | Steele L, Silver B, Beegun I, Saleh H. Cervical aortic arch: an unusual cause of a pulsatile neck mass. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Priya S, Nagpal P. Virtual modeling and interactive virtual reality display of unusual high-riding cervical aortic arch. Ann Pediatr Cardiol. 2021;14:122-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Halpin JS, Kunin JR, Rosado-de-Christenson ML. Right-sided oropharyngeal cervical aortic arch. J Thorac Imaging. 2010;25:W124-W127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Baravelli M, Borghi A, Rogiani S, Preda L, Quattrociocchi M, Fantoni C, Crupi G, Tiraboschi R. Clinical, anatomopathological and genetic pattern of 10 patients with cervical aortic arch. Int J Cardiol. 2007;114:236-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Reid DG. Three Examples of a Right Aortic Arch. J Anat Physiol. 1914;48:174-181. [PubMed] |
| 6. | Zhong YL, Ma WG, Zhu JM, Qiao ZY, Zheng J, Liu YM, Sun LZ. Surgical repair of cervical aortic arch: An alternative classification scheme based on experience in 35 patients. J Thorac Cardiovasc Surg. 2020;159:2202-2213.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Satyavolu RS, Fischer R, Ramadoss R. Upper Airway Obstruction in an Adult: An Unusual Presentation-Dissection of the Cervical Aortic Arch. Indian J Crit Care Med. 2021;25:732-734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Khoury NJ, Hourani R, Birjawi GA, Hourani MH. Left-sided cervical aortic arch associated with pseudocoarctation, aneurysm formation, and anomalous left brachiocephalic vein: appearance on MDCT and MR angiography. J Thorac Imaging. 2008;23:206-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Tsukamoto O, Seto S, Moriya M, Yano K. Left cervical aortic arch associated with aortic aneurysm, aortic coarctation, and branch artery aneurysm--a case report and review. Angiology. 2003;54:257-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Dasari TW, Paliotta M. Images in clinical medicine. Cervical aortic arch. N Engl J Med. 2014;371:e38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Shayan G, Shao J, Wang Y, Si L, Shen J, Chen Y, Liu B, Zheng Y. Management of cervical aortic arch complicated by multiple aneurysms. Interact Cardiovasc Thorac Surg. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Higuchi K, Koseni K, Takamoto S. Left-sided cervical aortic arch aneurysm: case report. J Thorac Cardiovasc Surg. 2003;126:2098-2100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Guha S, Grover V, Aiyer P, Dhull J. A unique case of right cervical aortic arch with anomalous left common carotid artery and absent right common carotid artery. Ann Med Surg (Lond). 2016;9:58-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kaul P. 11 cm Haughton D left cervical aortic arch aneurysm. J Cardiothorac Surg. 2013;8:108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Haughton VM, Fellows KE, Rosenbaum AE. The cervical aortic arches. Radiology. 1975;114:675-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 66] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Hirao K, Miyazaki A, Noguchi M, Shibata R, Hayashi K. The cervical aortic arch with aneurysm formation. J Comput Assist Tomogr. 1999;23:959-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |