Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3241
Peer-review started: October 10, 2021
First decision: December 12, 2021
Revised: December 30, 2021
Accepted: February 23, 2022
Article in press: February 23, 2022
Published online: April 6, 2022
Processing time: 170 Days and 8.6 Hours
Appendico-vesicocolonic fistulas and appendiceal-colonic fistulas are two kinds of intestinal and bladder diseases that are rarely seen in the clinic. To our knowledge, no more than 4 cases of appendico-vesicocolonic fistulas have been publicly reported throughout the world, and no more than 100 cases of appendiceal-colonic fistulas have been reported. Although the overall incidence is low, an early diagnosis is difficult due to their atypical initial symptoms, but these diseases still require our attention.
Here, we report a case of a 77-year-old male patient diagnosed with an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula. The main manifestations were diarrhea and urine that contained fecal material. The diagnosis was confirmed by multiple laboratory and imaging examinations. A routine urinalysis showed red blood cells and white blood cells. Abdominal and pelvic computed tomography scans showed close adhesions between the bowels and the bladder, and fistulas could be seen. Colonoscopy and cystoscopy and some other imaging examinations clearly showed fistulas. The preoperative diagnoses were a colovesical fistula and an appendiceal-colonic fistula. The fistulas were repaired by laparoscopic surgical treatment. The diseased bowel and part of the bladder wall were removed, followed by a protective ileostomy. The postoperative diagnosis was an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula, and the pathology suggested inflammatory changes. The patient recovered well after surgery, and all his symptoms resolved.
The final diagnosis in this case was a double fistula consisting of an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula.
Core Tip: Appendico-vesicocolonic fistulas and appendicovesical fistulas are rare diseases involving the intestine and urinary bladder. These conditions have a very low morbidity even in patients with appendicitis after conservative treatment or with malignant tumors. Early symptoms and signs are usually atypical, making early diagnosis and treatment more difficult. Here, we present a case of an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula and provide some recommendations for diagnosis and treatment along with a review of the literature.
- Citation: Yan H, Wu YC, Wang X, Liu YC, Zuo S, Wang PY. Appendico-vesicocolonic fistula: A case report and review of literature. World J Clin Cases 2022; 10(10): 3241-3250
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3241.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3241
Appendicovesical fistulas are commonly seen as complications after conservative treatment of acute and chronic appendicitis and benign or malignant appendiceal neoplasms[1]. Appendicovesical fistulas account for approximately 5% of all enterovesical fistulas[2]. Appendiceal-colonic fistulas are commonly seen in diseases such as a vermiform appendix combined with acute or chronic appendicitis or benign or malignant appendiceal neoplasms. It also occurs in the sigmoid colon combined with colonic diverticulitis or colonic malignancy[3]. Colovesical fistulas are more commonly seen in sigmoid diverticulitis or colonic malignancy disease and are rarely seen with bladder malignancies originating on the left side of the bladder that invade the sigmoid colon. Sigmoid diverticulitis is the most common cause[4]. It has been reported that the incidence of colovesical fistula is 2%-23% in diverticular disease[5].
Appendico-vesicocolonic fistulas are composed of the above three fistulas. It is a rare disease, with only 3 cases reported thus far[6-8]. A case of simultaneous double fistulas, “appendico-vesicocolonic fistula combined with appendiceal-colonic fistula”, has not been reported thus far throughout the world. Here, we report a rare case of an appendico-vesicocolonic fistula with an appendiceal-colonic fistula.
A 77-year-old male patient was admitted to the hospital because of “diarrhea and urine having fecal material for 7 years”.
Seven years before presentation, the patient experienced diarrhea and frequent and urgent urination, accompanied by urine having fecal material with no obvious cause. He was admitted to the local hospital. Colonoscopy showed a fistula 15 cm away from the anus, and a colovesical fistula was considered. Surgical treatment was suggested, but the patient refused surgery because the symptoms did not significantly affect his quality of life at that time. Recently, the patient came to our hospital due to worsening of the symptoms of frequent and urgent urination. The patient did not receive any other trauma or treatment during the period between refusing the surgery and its acceptance.
The patient had hypertension and diabetes for many years but had no history of trauma or surgery.
There was no specific family history.
The patient had some mild tenderness in the lower abdomen. Percussion of the abdomen revealed dull percussion sounds.
Routine blood test: White blood cell (WBC) 7.9 × 109/L, hemoglobin (HBG) 127 g/L; Stool routine test
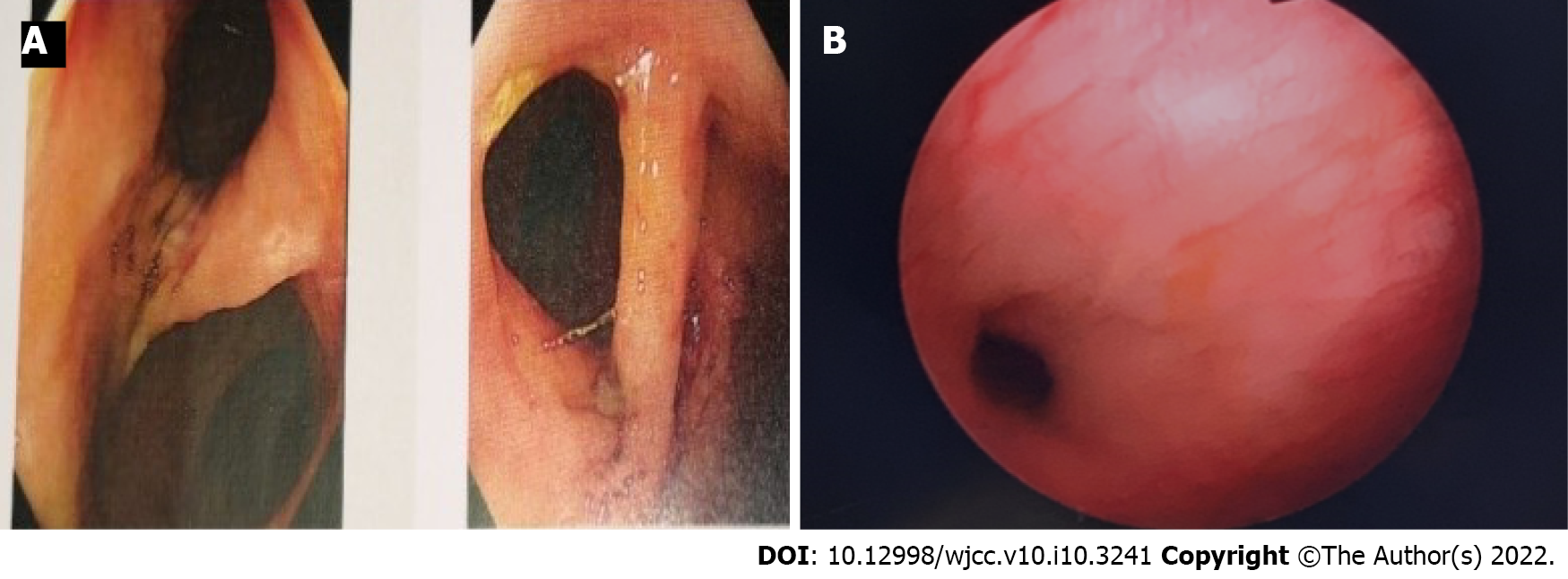
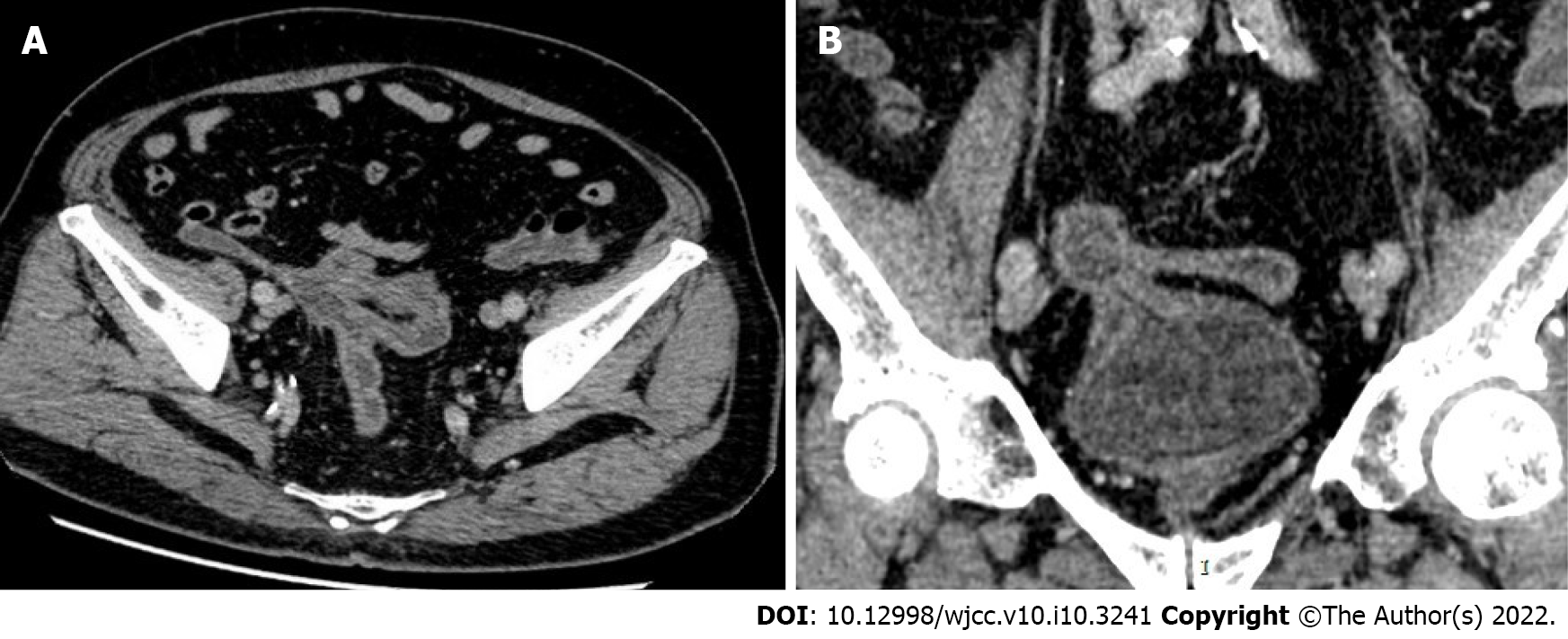
Colonoscopy: A fistula approximately 1.5 cm in size could be seen involving the sigmoid colon 20 cm from the anus. The endoscope could pass through the fistula, and the bladder mucosa could be seen. Another fistula with a size of approximately 1.2 cm could be seen 15 cm away from the anus. This suggested multiple colovesical fistulas (Figure 1A). Cystoscopy showed a high turbidity of the urine in the bladder, with a large amount of feces visible, and the wall of the bladder was edematous. A fistula could be seen in the lateral wall of the bladder. Both ureteral orifices were fissured, but the flow of urine was clearly visible (Figure 1B). Abdominal pelvic computed tomography (CT) showed that the appendix was not clearly visible. The distal sigmoid colon-cecum, right posterior to the top wall of the bladder-sigmoid colon, and middle sigmoid colon-cecal wall contained adhesions, and fistulas could be seen among these structures. A gas density shadow could be seen in the bladder. The involved intestinal wall and bladder wall were thickened, and a contrast-enhanced CT scan showed enhancements (Figure 2). In view of the previous consideration of a possible colovesical fistula and the complexity of the patient's condition, we considered a CT examination directly rather than a plain film or ultrasound. Plain films, ultrasound, fistulography and magnetic resonance imaging (MRI) were not performed later because the CT scan provided comprehensive information.
Preoperative diagnosis was a colovesical fistula and an appendiceal-colonic fistula. Postoperative diagnosis was an appendico-vesicocolonic fistula with an appendiceal-colonic fistula.
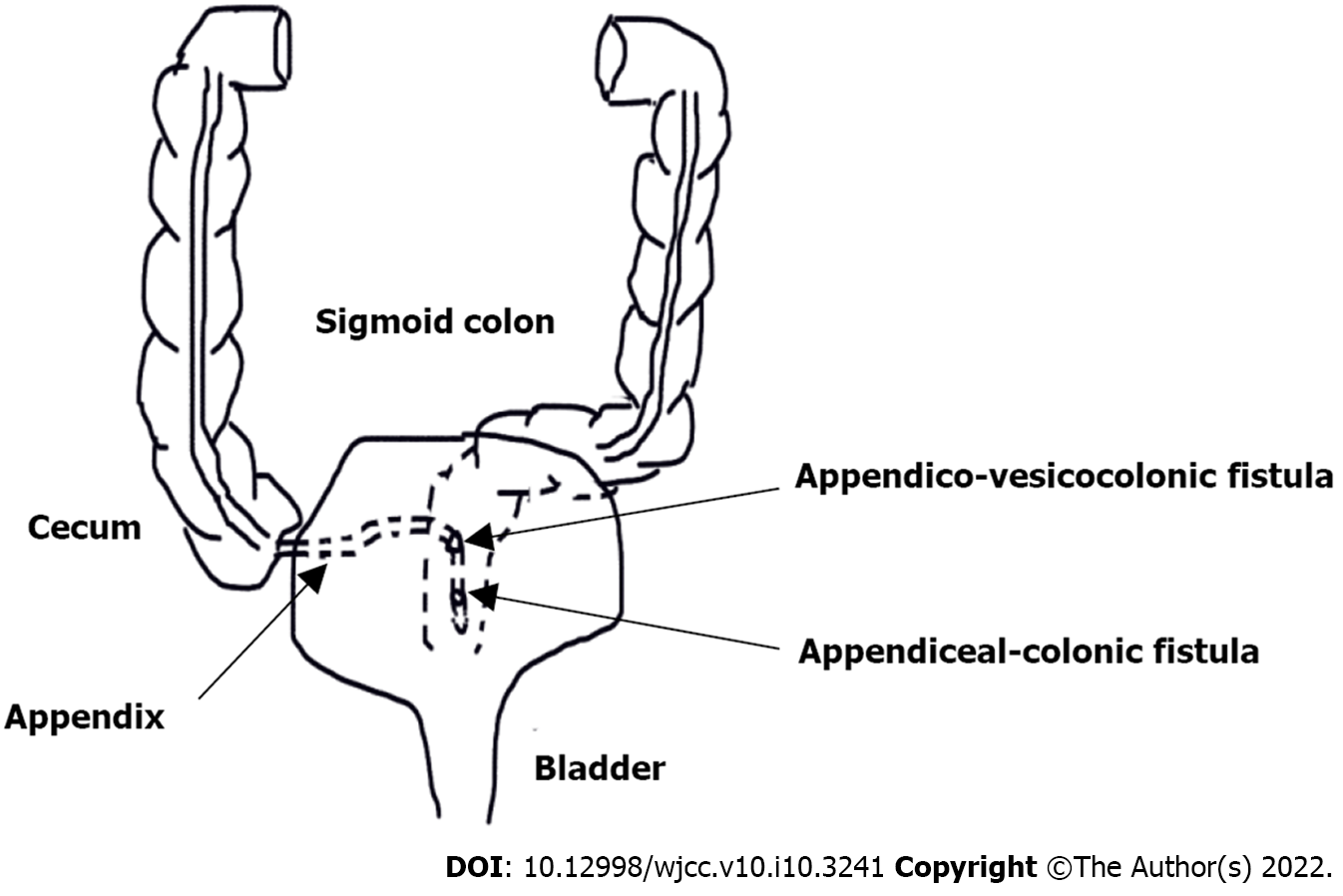
After completing the preoperative preparation and signing the informed consent, the surgeries, which consisted of “cystoscopy, bilateral Double J (D-J) ureteral tube placement, laparoscopic exploration, appendicectomy, resection and anastomosis of sigmoid colon, double-lumen protective ileostomy, bladder fistula neoplasty, and drainage tube placement” were performed. First, for the operation, bilateral D-J tubes were placed with cystoscopy. A zebra guidewire was set through the sinus tract. A catheter was inserted through the guide wire, and the catheter water bag was filled with water for subsequent guidance to find the sinus canal. Using laparoscopy, the water sac was found and located in the cecum. After the appendix was severed at its root from the cecum, the sinus tract was cut open, and the urinary duct was withdrawn. The urinary duct was withdrawn into the colon lumen and then into the bladder lumen. Then, it was confirmed that there was a three-way fistula of the appendix, colon and bladder. After that, sigmoidectomy and anastomosis were performed, and the other fistula revealed by colonoscopy was not found during the operation. The rectum was dissected in the upper segment, and a double-lumen protective ileostomy and bladder neoplasty were performed. The operation was successful with a minimal amount of bleeding.
The specimen was opened and revealed a fistula of approximately 1.5 cm in diameter in the middle of the appendix and leading to the colon and bladder.
Another fistula was seen approximately 5 cm away from the tip of the appendix, which was confirmed as a case of a double fistula consisting of an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula (Figure 3).
In the course of postoperative recovery, a urinary tract infection occurred, and the urinary culture grew Candida albicans. The infection was cured after antibiotics and antifungal agents were given. The bilateral D-J tubes were removed from the bladder under cystoscopy guidance one month after the operation, and the procedure was successful. Postoperative pathology of the resected rectum, appendix, and part of bladder showed the following: a segment of large intestine was evaluated with a length of 8 cm, and acute or chronic inflammation was present in the large intestinal wall. There was local mucosal erosion and infiltration of some eosinophils in the lamina propria. Two fistulas were observed in the wall of the large intestine. One fistula was adhered to part of the appendiceal wall, and the appendiceal wall was dilated, with mucosal erosion and degeneration. The other fistula was adhered to a small amount of hyperplastic fibers and smooth muscle tissue, and no transitional epithelium was observed. One lymph node around the large intestine showed reactive hyperplasia.
The patient has recovered well after surgery. In addition, the symptoms above have completely resolved.
Enterovesical fistulas were first described by Cripps[9] in 1888. Appendiceal-colic fistulas were first reported by Cherigie et al[10] in 1953.
The common causes of appendico-vesicocolonic fistulas mainly include inflammation, tumors, trauma, and iatrogenic and congenital diseases. Appendiceal-colonic fistulas often begin when acute or chronic appendicitis is combined with the formation of a local abscess, especially after conservative treatment. When the appendix is long and in the pelvic position, local inflammation and abscesses are more likely to be close to and invade the lengthy sigmoid colonic wall, leading to the formation of an appendiceal-colonic fistula. In addition, malignancy of the appendix, neuroma, cystic fibrosis, villous adenoma and parasites are also common causes[2]. Colovesical fistulas are more common in patients with colonic diverticulitis and colonic malignancy, especially in the sigmoid colon, which may be due to its high mobility and anatomical characteristics. According to the data, the incidence of diverticula developing into fistulas was 4% to 23%. Enterovesical fistulas are the most common type, accounting for 33% to 65% of all diagnosed diverticular fistulas[11]. According to the report, inflammatory bowel disease, colon radiotherapy, or bladder malignancy are also rare causes of colovesical fistula[12]. Dangle et al[13] reported that, rarely, enterovesical fistulas were the result of inflammatory and necrotic responses to the intravesical injection of mitomycin. The underlying etiologies of 66 patients diagnosed with enterovesical fistulas, as reported by Qiu et al[14], were intestinal cancer (46.97%), Crohn's disease (16.67%), colonic diverticulitis (15.15%), bladder cancer (12.12%), appendicitis and other inflammatory diseases (7.58%), and intraoperative injury (1.52%).
The clinical manifestations of appendico-vesicocolonic fistulas are diverse, and the common manifestations are frequent urination, pneumaturia, urine containing fecal material complex and persistent urinary tract infection, dysuria, diarrhea, abdominal discomfort and other symptoms. Sometimes the symptoms, such as urinary tract irritation, are relieved because the fistula is completely blocked by a bezoar, but temporary abdominal pain may occur when the bezoar in the fistula falls into the bladder[15]. Different patients have different clinical manifestations, and the above clinical symptoms do not always occur simultaneously. Therefore, the early diagnosis of an appendico-vesicocolonic fistula is much more difficult. In this case, the main clinical manifestations of the patient were diarrhea, fecal contamination, and frequent and urgent urination. Melchior et al[16] reported 49 patients with colovesical fistulas due to sigmoid diverticulitis, 71.4% of patients had pneumaturia, and 51% had fecal material within urine. Yagi et al[17] had previously reported on a patient with a sigmoid carcinoma within the colonic diverticulum, which invaded the bladder and resulted in a colovesical fistula, the main symptom of which was hematuria. In addition, Keane and Tebala[18] reported a rare case of hypokalemia and hyperchloremic metabolic acidosis. Most of the patients with appendico-vesicocolonic fistulas were male, which may be because the uterus plays a protective role in the formation of enterovesical fistulas[4]. Melchior et al[16] reported 49 patients with colovesical fistulas, only 7 patients (14.3%) were female, and 5 of them had undergone a hysterectomy. However, the clinical manifestations of appendiceal-colic fistulas are relatively vague and have a poor specificity, and patients have nonspecific symptoms such as discomfort in the lower abdomen, constipation, diarrhea and so on. Due to its nonspecific manifestations, a preoperative diagnosis is often difficult. The postoperative diagnosis is usually made through histopathological examination of resected specimens after exploratory surgery for other suspected diseases[19].
The diagnoses of appendico-vesicocolonic fistulas and appendiceal-colonic fistulas are often difficult. Although there are various diagnostic methods, different methods have different specificities and sensitivities, so it is often necessary to apply multiple simultaneous diagnostic methods to aid in diagnosis and to improve the detection rates.
In terms of laboratory examinations in patients with appendico-vesicocolonic fistulas, routine urine tests and urine cultures had the best results. Routine urine tests are commonly characterized by turbid urine with feces containing a large number of white blood cells and red blood cells. Escherichia coli and Klebsiella are usually found in the urine cultures[20].
In terms of imaging examinations in patients with appendico-vesicocolonic fistulas, compared with other diagnostic tools, abdominal CT is considered to be one of the most sensitive detection tools[21]. The main manifestations are as follows: the intestine and bladder are closely adhered, fistulas can be seen in some cases, gas density shadows can be seen in the bladder, there is corresponding intestinal and bladder wall thickening, and some other manifestations can be present. It has been reported that the detection rate of colovesical fistulas using abdominal spiral CT is between 60% and 100%[22]. In the study from Melchior et al[16], the detection rate using CT was 40%. Although the detection rate of appendico-vesicocolonic fistulas by CT is highly variable, CT is useful to exclude other organic diseases in the abdominal cavity, such as malignant tumors.
Colonoscopy and cystoscopy have a limited diagnostic value for appendico-vesicocolonic fistulas. According to relevant reports, the detection rate of enterovesical fistulas by colonoscopy is highly variable, ranging from 11% to 89%[22]. The low colonoscopy detection rate was mainly because some fistulas with stenosis in the neck were easily ignored or mistaken for colonic diverticula. Although cystoscopy is a routine test, it has been reported to diagnose no more than 50% of enterovesical fistulas[22]. Cystoscopy often presents some nonspecific findings, such as diffuse edema of the bladder wall and mucosal bulging. Only mature fistulas with obvious openings can be easily diagnosed with endoscopy. In the study from Melchior et al[16], the detection rate using colonoscopy was 8.5%, and the detection rate using cystoscopy was 10.2%. Although the diagnostic value of colonoscopy for enterovesical fistulas is limited, it helps to rule out inflammatory bowel disease and colon, appendix, and bladder tumors.
Detection of poppy seeds in urine is considered a positive confirmatory test for enterovesical fistulas. In some studies, the sensitivity of the poppy seed test to detect fistulas was 94.8%[23]. The poppy seed test involves taking 50 g of poppy seeds orally and visually testing urine for the presence of poppy seeds within 48 h. This experiment is simple and effective, with a high diagnostic rate and almost no side effects. However, it has not been carried out in our country (China) or in our center.
MRI is widely used in the diagnosis of appendico-vesicocolonic fistulas because of its quality imaging of soft tissues. The main radiographic findings were tubular hyperintensities on T2-weighted images and focal disruptions of the muscular layer of the bladder wall. A study by Ravichandran et al[24] showed that enterovesical fistulas were diagnosed by MRI in 18 out of 19 patients, and the related causes were analyzed. The patient reported in this paper did not receive an MRI examination because the diagnosis was confirmed by CT and endoscopy. In addition, barium enema studies, total alimentary tract contrast studies, cystography, and retrograde urography also play auxiliary roles in the diagnosis. Among them, the Bourne test had a higher detection rate, urine specimens were collected immediately after a barium enema, and the sediment was examined by radiography after centrifugation. If the sediment contained the barium agent, the diagnosis could be confirmed. However, few institutions have carried out such test.
For appendiceal-colonic fistulas, the main manifestations on CT are as follows: the distal appendix may be closely adhered to the lengthy sigmoid colon, local inflammation or abscesses can be seen, and the fistula can be seen in some cases. Fluorodeoxyglucose (FDG) positron emission tomography is helpful to distinguish between benign and malignant diseases[25]. Barium enemas are useful for the confirmation of appendiceal-colonic fistulas[26].
Given the atypical symptoms of enterovesical and appendiceal-colonic fistulas, differential diagnoses need to be considered. Because the common symptoms are abdominal pain in the hypogastrium and right/left iliac fossa, they are often differentiated from the following conditions: inflammatory and infectious conditions involving the ileocecal region, diverticulitis occurring in different parts of the digestive tract, malignancies of the appendix and colorectum, and other rare diseases[27]. Interestingly, van Breda Vriesman AC et al[28] found that infarction of the epiploic appendage or omentum can cause similar localized pain and can easily produce clinical symptoms that resemble appendicitis and diverticulitis, leading to unnecessary surgery. Trovato et al[29] reported a case of epiploic appendagitis with left lower abdominal pain, whose symptoms were similar to diseases such as diverticulitis and could be treated with conservative treatment. These possible differential diagnoses should all be taken into account.
For appendico-vesicocolonic fistulas, if they are secondary to a benign disease and the symptoms are mild, conservative treatment such as antibiotics can be attempted. However, relevant literature shows that the closure rate of the fistula remains low and there is a significant risk of infectious complications after conservative treatment[30]. Surgical treatment is recommended for appendico-vesicocolonic fistulas caused by malignant diseases or with more severe symptoms that affect normal life. The preferred surgical treatment strategy is a one-stage resection and anastomosis of the disordered bowel segment with or without prophylactic ileum or colon neostomy[16]. However, Hsieh et al[31] showed that the one-stage operation of enterovesical fistulas should be limited to patients with good nutrition and no severe inflammation, radiation injuries, intestinal obstructions, or advanced malignant tumors present and should not be pursued in elderly patients. In the study by Smeek et al[32], 53% of the patients underwent secondary surgery due to the advanced age of the patients in the study and the high rate of complications. For the bladder, if the lesion is caused by a benign disease, it is feasible to resect and suture the bladder wall. If malignant tumors involve the trigone of the bladder, a partial resection of the bladder wall with the preservation of the bladder may not be safe. If located outside the trigone of the bladder, partial bladder wall resection with bladder preservation should be considered[17]. There is a marked difference between benign and malignant disease in the treatment of appendiceal-colonic fistulas. If the lesion is benign, resection of the appendix, the fistula and part of the colon should be considered[33]. If the lesion is malignant, a right hemicolectomy, lymph node dissection with resection of the fistula and part of colon should be considered[34]. Specific methods of surgery include open surgery, laparoscopic surgery and robot-assisted surgery. Open surgery is considered the traditional method of treatment, and laparoscopy has been widely used with the maturity of technology in recent decades. Chung et al[35], Albrecht et al[1], Lee et al[36] and others reported successful cases using laparoscopic surgery. In our case, the laparoscopic technique was also used to successfully remove the diseased intestinal segment and repair the fistula. Kibar et al[37] reported a successful case using robot-assisted enterovesical fistula surgery. Postoperative complications include anastomotic fistulas and urinary tract infections. Our patient also developed a urinary tract infection after surgery. The main influencing factors for poor anastomotic healing include radiotherapy, the American Society of Anaesthesiologists (ASA) score, hormone therapy, emergency surgery, lack of surgical experience and a higher body mass index (BMI)[38].
The case presented here is the fourth reported case of an appendico-vesicocolonic fistula to date worldwide (Table 1). Marsha et al[6] previously reported a case in 1975 involving a 55-year-old male patient with bladder irritation and diarrhea as the main manifestations. A urine culture showed an E. coli infection, and a barium enema showed that the contrast agent quickly entered the bladder and filled the colon. Intraoperative exploration revealed an appendico-vesicocolonic fistula. Colostomy was performed after the resection of the lesion, and the stoma was closed 3 mo after surgery. Postoperative pathology showed chronic inflammatory changes. Blalock[7] reported a case in 1981 involving a 45-year-old male patient with diarrhea, urinary tract infection, pneumaturia and fecal contamination as the main manifestations. A urine culture showed an Escherichia coli infection. The excretory radiography, barium enema, and cystoscopy showed nonspecific inflammatory changes. During laparotomy, the necrotic tip of the appendix was found in the abscess cavity connected with the sigmoid colon and bladder, and the lesion was removed. Postoperative pathology suggested severe inflammatory changes. Keane and Tebala[18] reported a 15-year-old male who developed abdominal pain, dysuria, frequent urination and diarrhea after conservative treatment for appendicitis and upper abdominal trauma in 1983. A urinalysis revealed leukocytes present in the urine, and a urine culture grew Escherichia coli. Cystourethrography showed an extravasation of contrast medium, but no obvious abnormality was found by colonoscopy and cystoscopy. An exploratory laparotomy revealed fistulas in the appendix, bladder, and rectum, and the lesions were removed. In the 77-year-old man reported in our case, the main manifestations were diarrhea, frequent and urgent urination, and fecal contamination of the urine. Routine urine tests showed a significant increase in white blood cells and red blood cells, the CT showed fistula formation, and cystoscopy and colonoscopy showed fistulas. A laparoscopic resection of the lesion was followed by a protective ileum neostomy. Pathological findings indicated inflammation of the appendix and colon. This is the fourth publicly reported case of an appendico-vesicocolonic fistula. It was also the first double fistula case having an appendico-vesicocolonic fistula combined with an appendiceal-colonic fistula.
| Ref. | Age and gender (man-M/woman-F) | Etiology | Clinical manifestation | Library examinations | Imaging examinations | Treatment |
| Marsha et al[6], 1975 | 55/M | Chronic appendicitis | Frequent urination, diarrhea | Urine culture: E. coli | Barium enema: fistula | Open surgery (lesion resection + colostomy) |
| Blalock[7], 1981 | 45/M | Appendicular abscess | Diarrhea, urinary tract infections, gas urine, urine fecal stain | Urine culture: E. coli | Excretory imaging, barium enema, cystoscope: Nonspecific changes | Open operation (lesion resection) |
| Kathie et al[8], 1983 | 15/M | Appendicular abscess, trauma | Abdominal pain, nausea→trauma→abdominal pain, diarrhea, frequent urination, dysuria | Urine culture: E. coliUrine routine: WBC | Colonoscopy, cystoscopy, barium enema: nonspecific findings. Excretory imaging: Extravasation | Open surgery (removal of lesion) |
| Our 2022 | 77/M | Acute or chronic inflammation of the colon and inflammation of the appendix | Diarrhea, urine and feces, frequent and urgent urination | Urine routine: WBC, RBC (+) | CT: Fistula visible cystoscope & colonoscopy: Fistula visible | Laparoscopic surgery (lesion resection + ileostomy) |
This case is the first double fistula case involving an appendico-vesicocolonic fistula with an appendiceal-colonic fistula that has been publicly reported in the world, and it is also the first case of an appendico-vesicocolonic fistula treated by laparoscopic surgery. The clinical manifestations of this case varied, including feces in the urine, pneumaturia, complicated urinary tract infection and abdominal discomfort. However, the symptoms of this condition often lack specificity. The sensitivity and specificity of different examination methods vary greatly, and the combined application of multiple examinations is often required. The main treatment was the excision of the diseased intestine and bladder. Laparoscopic surgery can be performed by a skilled surgeon with satisfactory results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A, Silano F S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Albrecht K, Schumann R, Peitgen K, Walz MK. [Laparoscopic therapy of appendicovesical fistula -- two case reports]. Zentralbl Chir. 2004;129:396-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Wang W, Wang L, Xu J, Shi S, Tian Y, Zhang Y. Combination of CT imaging and endoscopy in diagnosis of appendicovesical fistula caused by appendiceal adenocarcinoma. J Xray Sci Technol. 2014;22:493-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Agarwal S, Sharma A, Aggarwal A, Sankhwar S. Air in the urine: a mystified patient and a concerned surgeon. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Garcea G, Majid I, Sutton CD, Pattenden CJ, Thomas WM. Diagnosis and management of colovesical fistulae; six-year experience of 90 consecutive cases. Colorectal Dis. 2006;8:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Small WP, Smith AN. Fistula and conditions associated with diverticular disease of the colon. Clin Gastroenterol. 1975;4:171-199. [PubMed] |
| 6. | Marshall VR, Molland E, Blandy JP. Appendico-vesico-colic fistula. Br J Urol. 1975;47:544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Dalessandri KM, Swafford GR. Appendico-vesicocolonic fistula. J Urol. 1983;130:777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Cherigie, Proux, Bourdon. [Sigmoid pseudocancer, appendiculo-sigmoid fistula, resection of the fistula, postoperative obstruction, study of the small intestine]. Arch Mal Appar Dig Mal Nutr. 1953;42:989-991. [PubMed] |
| 11. | Eglinton T, Nguyen T, Raniga S, Dixon L, Dobbs B, Frizelle FA. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 119] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Najjar SF, Jamal MK, Savas JF, Miller TA. The spectrum of colovesical fistula and diagnostic paradigm. Am J Surg. 2004;188:617-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 77] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Dangle PP, Wang WP, Pohar KS. Vesicoenteric, vesicovaginal, vesicocutaneous fistula -an unusual complication with intravesical mitomycin. Can J Urol. 2008;15:4269-4272. [PubMed] |
| 14. | Qiu SL, Yu JW, Liu XH, Wang HY. Diagnosis and treatment of 66 cases with vesicoenteric fistula. Chin J Postgrad Med. 2019;42. [DOI] [Full Text] |
| 15. | Abubakar AM, Pindiga UH, Chinda JY, Nggada HA. Appendicovesical fistula associated with Hirschsprung's disease. Pediatr Surg Int. 2006;22:617-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Melchior S, Cudovic D, Jones J, Thomas C, Gillitzer R, Thüroff J. Diagnosis and surgical management of colovesical fistulas due to sigmoid diverticulitis. J Urol. 2009;182:978-982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Yagi Y, Shoji Y, Sasaki S, Yoshikawa A, Tsukioka Y, Fukushima W, Hirosawa H, Izumi R, Saito K. Sigmoid colon cancer arising in a diverticulum of the colon with involvement of the urinary bladder: a case report and review of the literature. BMC Gastroenterol. 2014;14:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Keane S, Tebala GD. Appendicovesical fistula presenting as hypokalaemic hyperchloraemic metabolic acidosis: a case report. Ann R Coll Surg Engl. 2019;101:e131-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Hakim S, Amin M, Cappell MS. Limited, local, extracolonic spread of mucinous appendiceal adenocarcinoma after perforation with formation of a malignant appendix-to-sigmoid fistula: Case report and literature review. World J Gastroenterol. 2016;22:8624-8630. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Trinavarat P, Mahayosnond A, Riccabona M. Appendico-vesical fistula: A clinical and imaging challenge—A case report based discussion of imaging implication. Eur J Radiol Extra. 2009;71:e101-e103. [DOI] [Full Text] |
| 21. | Scozzari G, Arezzo A, Morino M. Enterovesical fistulas: diagnosis and management. Tech Coloproctol. 2010;14:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Tsivian A, Kyzer S, Shtricker A, Benjamin S, Sidi AA. Laparoscopic treatment of colovesical fistulas: technique and review of the literature. Int J Urol. 2006;13:664-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Leicht W, Thomas C, Thüroff J, Roos F. [Colovesical fistula caused by diverticulitis of the sigmoid colon: diagnosis and treatment]. Urologe A. 2012;51:971-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Ravichandran S, Ahmed HU, Matanhelia SS, Dobson M. Is there a role for magnetic resonance imaging in diagnosing colovesical fistulas? Urology. 2008;72:832-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Nakamoto H, Yokota R, Namba H, Ishikawa T, Yamada K, Hosoda M, Taguchi K. A Benign Appendiceal-Colonic Fistula, Diagnosed and Managed Laparoscopically: A Case Report. Am J Case Rep. 2020;21:e925946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Morris-Stiff GJ, Islam KA. Appendico-colic fistula complicating appendicitis in cystic fibrosis. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Purysko AS, Remer EM, Filho HM, Bittencourt LK, Lima RV, Racy DJ. Beyond appendicitis: common and uncommon gastrointestinal causes of right lower quadrant abdominal pain at multidetector CT. Radiographics. 2011;31:927-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | van Breda Vriesman AC, Lohle PN, Coerkamp EG, Puylaert JB. Infarction of omentum and epiploic appendage: diagnosis, epidemiology and natural history. Eur Radiol. 1999;9:1886-1892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 103] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Trovato P, Simonetti I, Verde F, Lomoro P, Vinci G, Tarotto L, Corvino F, Corvino A. Acute epiploic appendagitis: ultrasound and computed tomography findings of a rare case of acute abdominal pain and the role of other imaging techniques. Pol J Radiol. 2020;85:e178-e182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Granieri S, Sessa F, Bonomi A, Paleino S, Bruno F, Chierici A, Sciannamea IM, Germini A, Campi R, Talso M, Facciorusso A, Deiana G, Serni S, Cotsoglou C. Indications and outcomes of enterovesical and colovesical fistulas: systematic review of the literature and meta-analysis of prevalence. BMC Surg. 2021;21:265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Hsieh JH, Chen WS, Jiang JK, Lin TC, Lin JK, Hsu H. Enterovesical fistula: 10 years experience. Zhonghua Yi Xue Za Zhi (Taipei). 1997;59:283-288. [PubMed] |
| 32. | Smeenk RM, Plaisier PW, van der Hoeven JA, Hesp WL. Outcome of surgery for colovesical and colovaginal fistulas of diverticular origin in 40 patients. J Gastrointest Surg. 2012;16:1559-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Joo JS, Agachan F, Wexner SD. Laparoscopic surgery for lower gastrointestinal fistulas. Surg Endosc. 1997;11:116-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 34. | Knigge U, Hansen CP. [Appendiceal carcinoid tumors and goblet cell carcinoids]. Ugeskr Laeger. 2010;172:1678-1681. [PubMed] |
| 35. | Chung CW, Kim KA, Chung JS, Park DS, Hong JY, Hong YK. Laparoscopic treatment of appendicovesical fistula. Yonsei Med J. 2010;51:463-465. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Lee JW, Ahn JH, Ha HK. Vesico-Appendiceal Fistula Misdiagnosed as Meckel's Diverticulum: A Laparoscopic Approach. World J Mens Health. 2012;30:195-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Kibar Y, Yalcin S, Kopru B, Kaya E, Topuz B, Ebiloglu T. Robot-Assisted Laparoscopic Repair of Spontaneous Appendicovesical Fistula. J Endourol Case Rep. 2016;2:111-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 38. | Alves A, Panis Y, Trancart D, Regimbeau JM, Pocard M, Valleur P. Factors associated with clinically significant anastomotic leakage after large bowel resection: multivariate analysis of 707 patients. World J Surg. 2002;26:499-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 336] [Article Influence: 14.6] [Reference Citation Analysis (0)] |