Published online Apr 6, 2022. doi: 10.12998/wjcc.v10.i10.3005
Peer-review started: June 16, 2021
First decision: September 5, 2021
Revised: September 20, 2021
Accepted: February 22, 2022
Article in press: February 22, 2022
Published online: April 6, 2022
Processing time: 285 Days and 16.1 Hours
Elevated intra-abdominal pressure (IAP) is a known cause of increased morbidity and mortality among critically ill patients. Intra-abdominal hypertension (IAH) and abdominal compartment syndrome can lead to rapid deterioration of organ function and the development of multiple organ failure. Raised IAP affects every system and main organ in the human body. Even marginally sustained IAH results in malperfusion and may disrupt the process of recovery. Yet, despite being so common, this potentially lethal condition often goes unnoticed. In 2004, the World Society of the Abdominal Compartment Syndrome, an international multidisciplinary consensus group, was formed to provide unified definitions, improve understanding and promote research in this field. Simple, reliable and nearly costless standardized methods of non-invasive measurement and monitoring of bladder pressure allow early recognition of IAH and timely optimized management. The correct, structured approach to treatment can have a striking effect and fully restore homeostasis. In recent years, significant progress has been made in this area with the contribution of surgeons, internal medicine specialists and anesthesiologists. Our review focuses on recent advances in order to present the complex underlying pathophysiology and guidelines concerning diagnosis, monitoring and treatment of this life-threatening condition.
Core Tip: Elevated intra-abdominal pressure is a common, life-threatening condition associated with increased morbidity and mortality. Unrecognized intra-abdominal hypertension (IAH) quickly leads to the development of multiple organ failure; therefore, vigilance is necessary in relation to high-risk patients. Monitoring bladder pressure in this group allows early recognition of IAH/abdominal compartment syndrome and timely intervention which can have a striking effect and fully restore homeostasis. Although the progress made in recent years is significant, there are still open questions which leave room for future research.
- Citation: Łagosz P, Sokolski M, Biegus J, Tycinska A, Zymlinski R. Elevated intra-abdominal pressure: A review of current knowledge. World J Clin Cases 2022; 10(10): 3005-3013
- URL: https://www.wjgnet.com/2307-8960/full/v10/i10/3005.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i10.3005
Increased intra-abdominal pressure (IAP) has drawn attention and become an accentuated condition in critically ill patients over the last few years[1-3]. IAP is defined as pressure concealed within the abdominal cavity, which is relative to the respiratory phase and abdominal wall resistance. It was first recognized in the 19th century with a recent increase of interest and publications in this field. In 1863, Marey noticed a link between the respiratory system and abdominal pressure for the first time. Promptly after this discovery, a damaging effect on other organs was described, inspiring scientists to explore this phenomenon in animal models in the early 20th century. In the following years, surgeons made a significant contribution to understanding gastrointestinal, cardiac and pulmonary complications and restoring their function through decompression of the abdominal cavity. Accumulation of clinical data throughout the last decades has led to a better understanding of underlying pathophysiology and its consequences. The impact of elevated IAP is not only limited to deterioration of intra-abdominal organs function but rather directly and indirectly influences different systems and main organs[4]. Untreated pre-existing comorbidities, abdominal trauma or surgical interventions and extra-abdominal diseases like chronic kidney disease, heart failure or impaired respiratory function, exacerbate the harmful effects of elevated IAP. In these high-risk subpopulations, even marginal sustained rise in IAP results in malperfusion and potential subsequent multiple organ failure.
In 2004, the World Society of the Abdominal Compartment Syndrome (WSACS), an international multidisciplinary consensus group, was formed from critical care, surgical and trauma experts to provide standardized definitions, promote research in this field and improve survival of patients affected by intra-abdominal hypertension (IAH) and abdominal compartment syndrome (ACS). WSACS specialists published new definitions and recommendations for IAP measurement and management. According to created guidelines, normal IAP in critically ill adults ranges approximately from 5 mmHg to 7 mmHg. IAH is defined as a sustained or repeated rise in IAP above 12 mmHg and is divided into four grades, namely grade I: 12-15 mmHg, grade II: 16-20 mmHg, grade III: 21-25 mmHg and grade IV: > 25 mmHg. ACS is defined as a sustained IAP > 20 mmHg associated with new organ dysfunction or failure[5].
The following review focuses on current knowledge of elevated IAP, its relationship with deterioration of organ function and structured management of this condition which can be applied in general internal and surgical practice.
A series of the latest studies indicates a high prevalence of IAH ranging from 28% to 71% depending on the studied cohort of patients admitted to critical care units. In comparison, ACS developed in 3%-12% of admissions. Moreover, IAH was a significant and independent predictor for short- and long-term mortality and was significantly associated with severe organ failures and prolonged stay in the hospital[6-8]. Depending on the study, ICU mortality was considerably higher in IAH and ACS groups compared to normal IAP, and the grade of IAH was inversely related to outcome. According to the study conducted by Smit et al[6], both intensive care and 90-d mortality were higher in IAH (4.8% and 15.2%, respectively) and ACS (16.7% and 38,9%, respectively) in comparison to patients with normal IAP (1.2% and 7.1%, respectively). In addition, mechanical ventilation with positive pressure, obesity, sepsis, positive fluid balance, acute respiratory distress syndrome and anemia were indicated repeatedly as risk factors of IAH development[9].
The complicated pathophysiology of raised IAP remains poorly understood. The deteriorated function of organs has been observed for years but this complex network of interactions is now being rediscovered (Table 1).
| Location | Effect of IAH |
| Central nervous system | ↑ Intracranial pressure |
| ↓ Cerebral perfusion pressure | |
| ↓ Venous outflow | |
| ↑ Intracerebral venous pooling | |
| Thorax | ↑ Intrathoracic pressure |
| ↑ Inferior vena cava diameter | |
| ↓ Wall compliance | |
| Cardiovascular system | ↑ Obstruction of vena cava |
| ↓ Venous return (preload) | |
| ↓ Cardiac output | |
| ↓ Ventricular compliance and contractility | |
| ↑ Compression of the aorta and systemic vasculature | |
| ↑ Systemic vascular resistance (afterload) | |
| ↑ Compression of pulmonary parenchyma | |
| ↑ Pulmonary vascular resistance | |
| ↑ Central venous pressure | |
| ↑ Pulmonary artery occlusion pressure | |
| Lungs | Atelectasis |
| ↓Compliance | |
| ↑ Infection rate | |
| Alveolar volutrauma | |
| ↑ Peak inspiratory pressure | |
| ↑ Mean airway pressure | |
| ↑ Ventilation-perfusion mismatch | |
| ↑ Pulmonary dead space | |
| ↑ PaCO2 | |
| ↓ PaO2 | |
| Abdomen | ↓ Abdominal perfusion pressure |
| ↓ Wall compliance | |
| ↓ Wall blood flow | |
| ↓ Celiac and mesenteric blood flow | |
| ↑ Mesenteric venous pressure | |
| ↑ Visceral swelling | |
| ↑ Ischaemia | |
| ↑ Feeding intolerance | |
| ↓ Intramucosal pH | |
| Bacterial translocation | |
| Liver | ↓ Portal blood flow |
| ↓ Hepatic artery blood flow | |
| ↓ Hepatic vein blood flow | |
| ↓ Lactate clearance | |
| Kidney | ↓ Renal blood flow |
| ↑ Renal venous pressure | |
| ↑ Renal vascular resistance | |
| ↓ Glomerular filtration rate | |
| ↓ Diuresis | |
| ↑ Blood urea nitrogen concentration | |
| ↑ Serum creatinine | |
| ↑ Activation of renin-angiotensin-aldosterone axis | |
| ↑ Antidiuretic hormone release |
The abdominopelvic cavity is the body chamber defined by rigid bone structures and soft tissue. A slow increase in internal pressure causes the walls to expand but their abilities to compensate are limited. When they are exceeded, a force applied to the diaphragm causes a cephalic shift which was first described in 1922. This movement results in a reduced volume of the thoracic cavity and changed distribution of pressures. This concept which is called abdominal compliance (AC) is defined as a measure of the capability of abdominal expansion, which depends on the elasticity of the abdomen and diaphragm, and can be expressed as a change in intra-abdominal volume per change in IAP. AC depends on both these components and its dynamic of changes over time is thus hard to evaluate AC directly. Nevertheless, it should be considered an important component of IAP, playing a significant role in organ interactions and end-organ perfusion. Understanding AC helps in applying the right management strategies and preventing the consequences of increased IAP. Particularly patients with IAH and reduced AC can benefit even from a small reduction in IAV[10,11].
Reduction of thorax volume caused by deviation of the diaphragm is accompanied by an elevation of the thoracic pressure which declines the preload and thus cardiac output[12-14]. Such alterations were observed already at pressures of 10 mmHg in animal models[15]. The unfavorable effect can be aggravated additionally by hypovolemia. A rise in IAP followed by higher intrathoracic pressure results in impairment of ventricular compliance and compression of systemic and pulmonary arteries leading to an increasing afterload[16]. A combination of these factors affects the venous system. Reduction in venous return can be observed due to increased pressure in the vena cava and is proportional to the increase in pressure in the abdominal cavity[12]. Data suggest that fluid resuscitation improves venous return and thus diminishes the negative effect of increased afterload[16]. Furthermore, patients are at risk of deep venous thrombosis because of a rise in hydrostatic pressure throughout veins and the formation of peripheral edemas.
Compression of pulmonary tissue results in a higher intrapulmonary shunt fraction; therefore, it may contribute to the development of respiratory failure. This effect begins with an IAP > 16 mmHg. Alterations in dynamic and static spirometry variables are observed. A decrease in vital capacity, residual capacity and an increase in pleural, inspiratory and peak pressures are prevalent[17].
Deterioration of alveolar blood flow, ventilation-perfusion mismatch and atelectasis are presented with hypercarbia and hypoxemia in arterial blood samples and are frequently accompanied by infective complications[18].
In the state of elevated IAP, renal function should be considered at all times during therapy. The pressure determining the proper blood flow through the abdominal organs is called the abdominal perfusion pressure (APP). It is calculated using the mean arterial pressure (MAP) and IAP. APP results from the difference between these two variables.
The organ most exposed to changes in IAP is the kidney. The divertive parameter from APP that refers directly to kidney function is called the renal filtration gradient (RFG). The RFG, assuming a pressure in the proximal tubule is equal to IAP, can be calculated from the formula RFG = MAP-2 × IAP. Acute kidney injury induced by declined renal blood flow, venous congestion and parenchymal compression is a common finding among all patients with IAH[19-23].
As a response, the renin-angiotensin-aldosterone axis is chronically activated and an increase in antidiuretic hormone concentration can be observed[24]. A large decrease in urine sodium concentration is demonstrated which contributes to the development of diuretic resistance and further disturbs the fluid balance[25,26]. The effect of IAH on the kidney is highly dependent on pressure value. With an IAP between 15 and 20 mmHg, reduced renal filtration pressure leads to oliguria (2-5 mL/kg per hour of diuresis) followed by the development of anuria at 30 mmHg. Also, an IAP of 20 mmHg causes an increase in renal vascular resistance by 500% and 1500% at 40 mmHg[27]. These changes shunt blood from the kidney, start glomerular necrosis, cause tubular damage and progress towards renal insufficiency[19].
The influence of IAP on the gastrointestinal tract cannot be ignored. Reduced blood flow combined with compression leads to venous hypertension in the visceral vascular system causing edema in the intestinal tissue. Along with it, the pressure in the abdominal cavity also increases, promoting further ischemic changes, malabsorption syndrome, bacterial flora translocation, metabolic acidosis and finally increasing mortality. A specific scale has been developed to predict mortality caused by intestinal dysfunction in patients with IAH[28]. Hepatic complications are common as the liver is sensitive to changes in abdominal pressure. In conditions of IAH, both hepatic blood vessel and portal vein blood flow is decreased. As a response to congestion, hepatocellular injury occurs[29]. Compromised mitochondrial function results in altered glucose metabolism and increased lactic acid concentration. This effect has been observed at an IAP of only 10 mmHg with preserved normal mean arterial blood pressure and cardiac output[13].
Venous blood return from the cerebrum affected by elevated pressure in the abdomen and thorax can cause an increase of intracranial venous blood volume, a rise in intracranial pressure and a decrease in cerebral perfusion pressure[12]. These factors lead to cerebral edema and worsening of neurological functions[30,31].
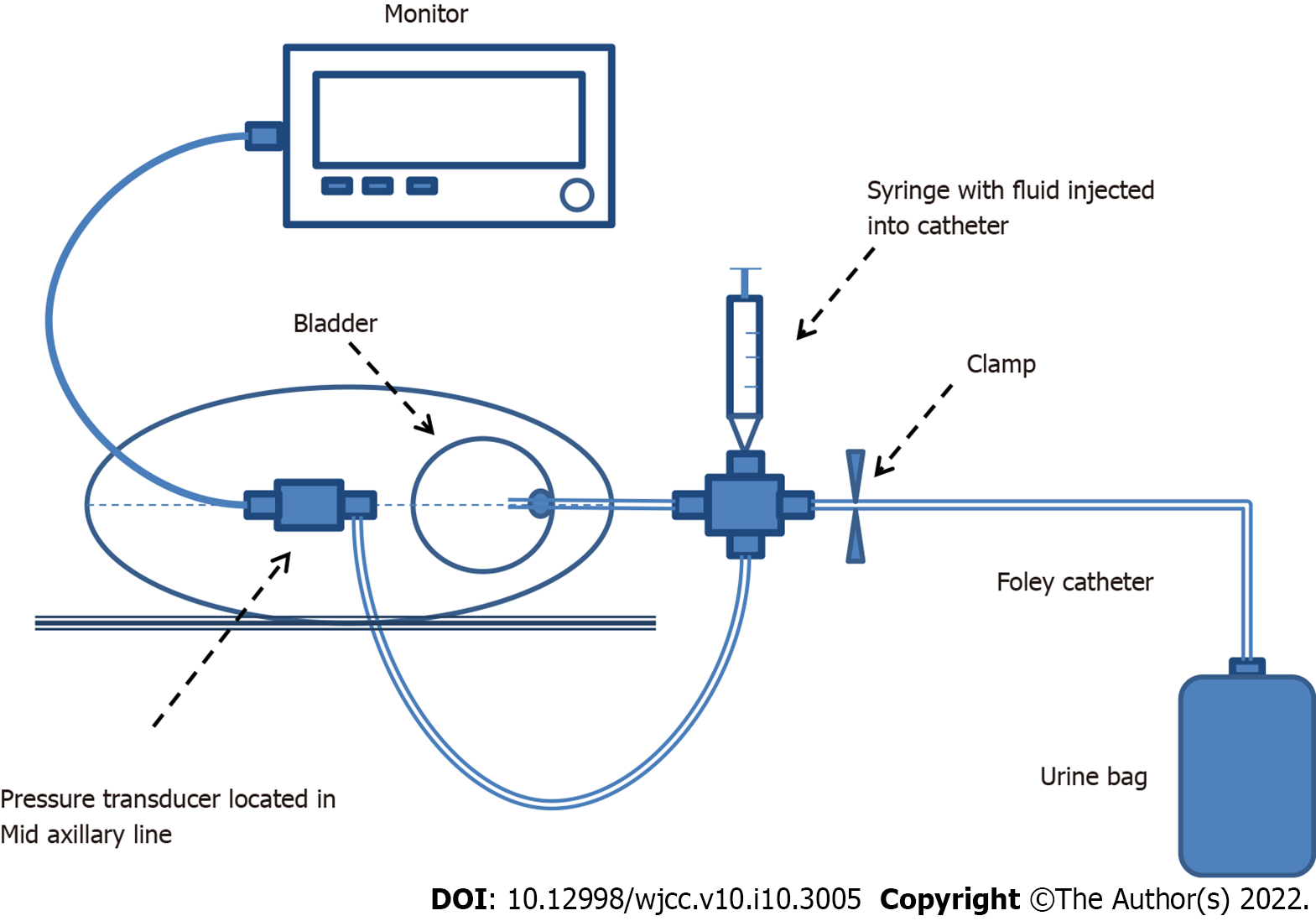
Physical examination has been proven unreliable and imprecise in IAH diagnosis[32-34]. Since monitoring IAP is of fundamental importance for profiling patients and guiding therapy, different methods of its assessment have been proposed. The first attempts to measure IAP were associated with an invasive peritoneal puncture procedure and the direct measurement of IAP using a peritoneal dialysis catheter. In the past, other methods like intramuscular continuous automatic piezoresistive pressure reading were confirmed as precise and consistent with non-direct measurements in porcine models. However, it has not been evaluated for safety and reliability in the ICU environment. Therefore, other less invasive methods have been developed as an alternative. IAP can be estimated by recording bladder pressure (using a Foley catheter), stomach pressure (using a nasogastric or gastrostomy tube), rectal pressure (using a balloon catheter) or inferior vena cava pressure. Transurethral measurement gained special recognition among these measurements because of its simplicity, reliability, consistency and low cost. The bladder is a passive reservoir which reflects IAP accurately[35]. In this technique, a Foley catheter is inserted into a vesicle and filled with 25 mL of saline, which guarantees the transfer of hydrostatic pressure between the bladder wall and the pressure measuring device. As a device, a simple standpipe or conventional electronic transducer can be used. The tip of the pressure tube is connected to the catheter to prevent air from entering the line and avoid dampened readings (Figure 1). Recently, commercially produced measurement kits have been available on the market. WSACS recommends measuring IAP every 4 h in the complete supine position without abdominal muscle activity and at end-expiration phase. The transducer should be zeroed at the mid-axillary line level and at the level of the iliac crest for 30-60 s after installation of body temperature fluid to allow bladder detrusor muscle relaxation. This reduces inaccuracy and ensures reproducibility of the measurement. While using standpipe, reading in cmH2O should be converted to mmHg. Intravesical measurement is a gold standard for indirect measurement proposed by WSACS, although it is only suitable for intermittent use[36,37].
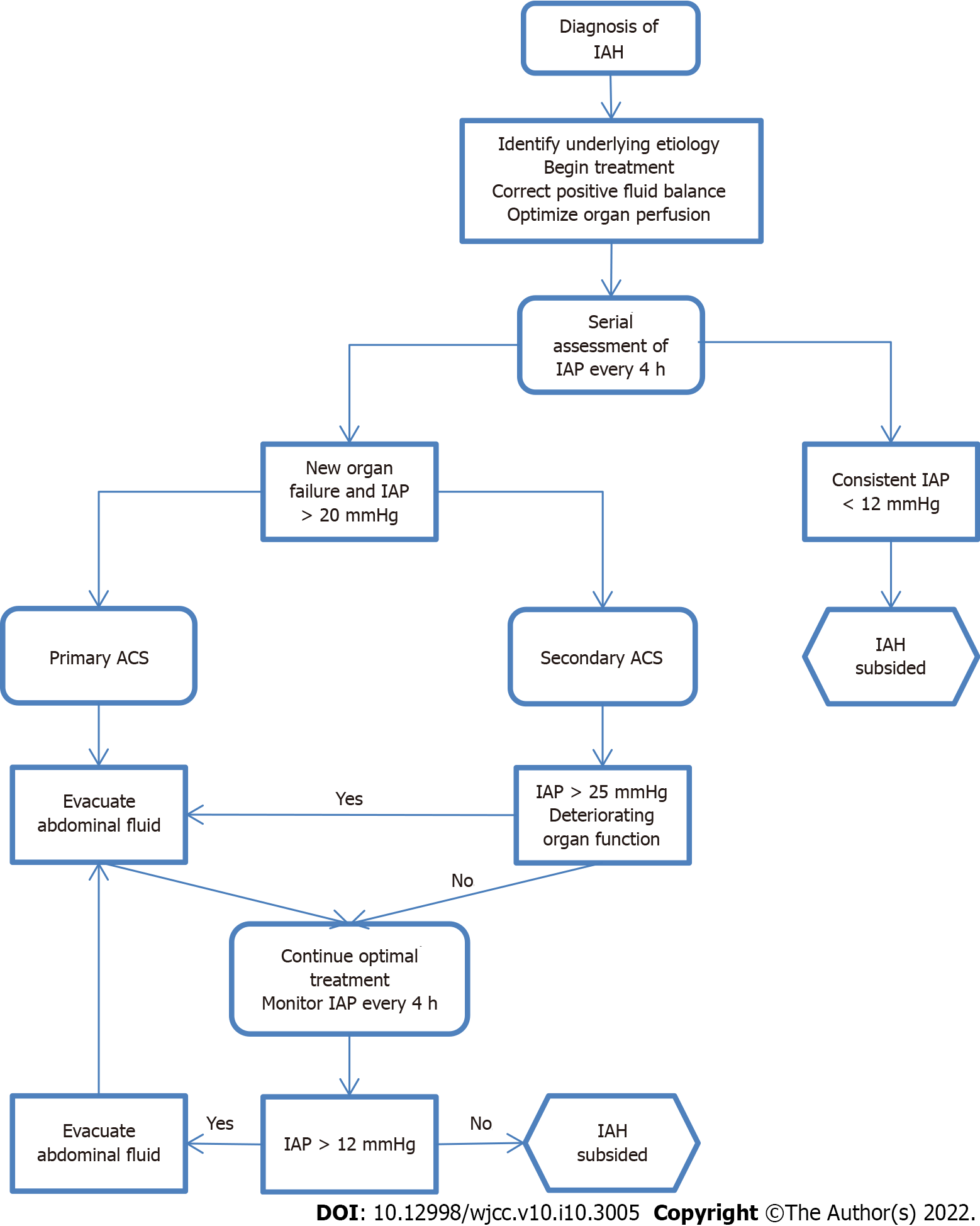
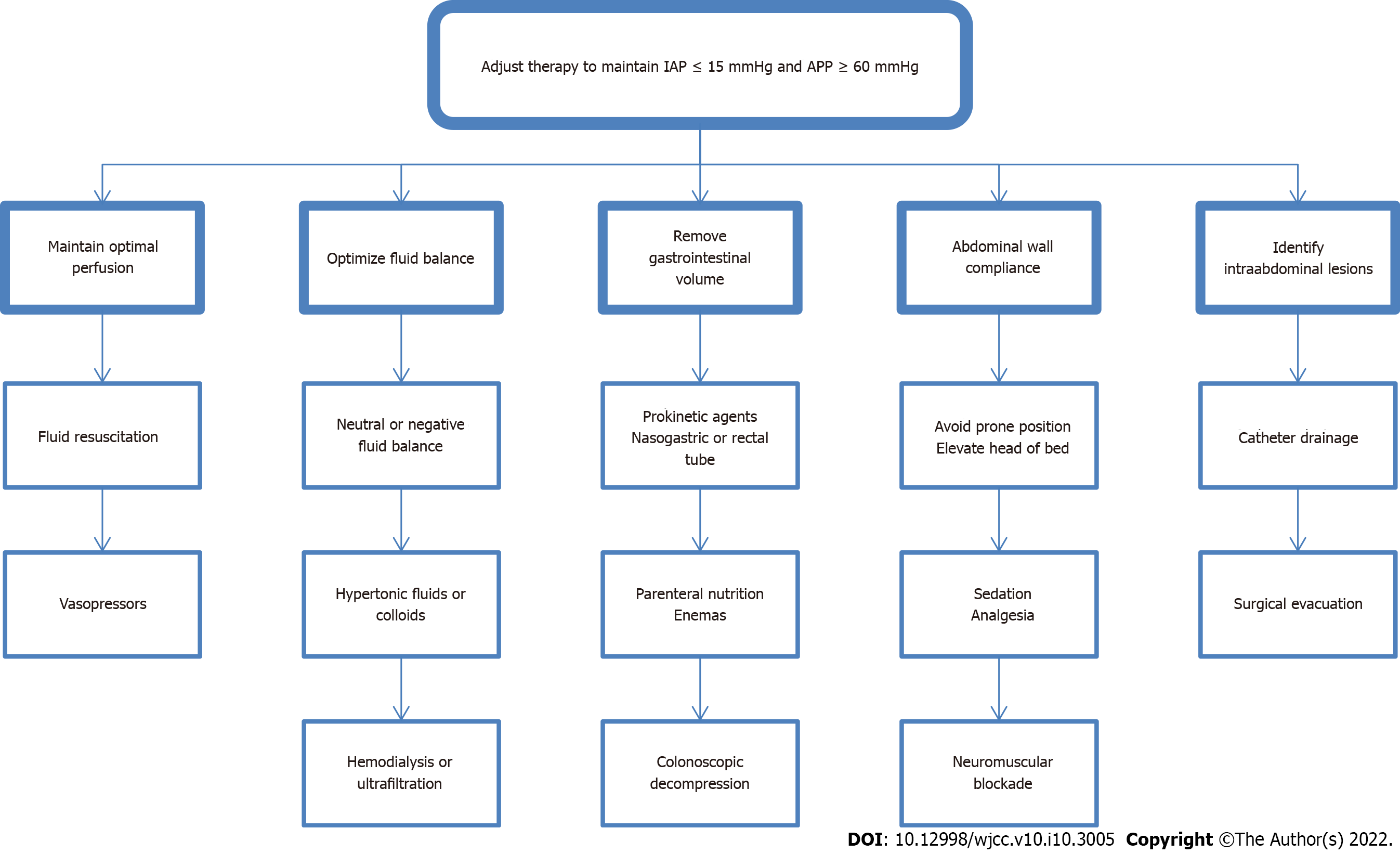
The goal of the treatment is to reduce IAP, restore regular systemic perfusion, reduce risk and avoid permanent end-organ damage. To achieve it, WSACS recommends a strategy that consists of improving abdominal wall compliance, evacuating intra-luminal contents and excessive abdominal fluid collections, correcting positive fluid balance and supporting organs. However, it is essential to remember that clinical judgment and physical examination are far from accurate estimating IAP. Therefore, the ACS management algorithm has been developed to help clinicians in the process of decision-making. This integrated approach results in improved outcomes and higher economic efficiency.
As soon as IAH is diagnosed, actions should be taken to lower the pressure inside the abdominal cavity. Underlying etiology has to be identified and treated. To improve wall compliance, sedation and neuromuscular blockade can be initiated. If possible, the head of the bed angle should be under 30 degrees. Intra-luminal contents can be removed by nasogastric or rectal decompression, and prokinetic drugs can be applied. Invasive procedures like paracentesis or percutaneous drainage are recommended for evacuating residual fluid from the abdomen. The options of correcting the fluid balance include diuretics, colloids or hypertonic fluids, hemodialysis and ultrafiltration. If all of the above have failed, surgical intervention might be indicated. Abdominal decompression technique called open abdomen (OA) therapy is proven to enhance renal function and urine output, improve cardiac index and lung compliance[38]. These changes have major repercussions on hemodynamics. Lowered CVP and higher tidal volume are observed, which physicians must be prepared for and adjust resuscitation as well as parameters of mechanical ventilation appropriately. The intensivist should optimize the process aiming for early fascial closure to avoid delayed extubation, development of fistulas and septic complications of extended OA therapy. Hypothermia, coagulopathy and acidosis are general concerns that should be addressed. Choosing optimal therapy requires a personalized approach. After implementing appropriate treatment, IAP should be monitored with serial assessments every 4 h (Figures 2 and 3).
Elevated IAP is a common, life-threatening condition associated with increased morbidity and mortality. Unrecognized IAH quickly leads to the development of multiple organ failure, therefore, vigilance is necessary in relation to high-risk patients. Monitoring bladder pressure in this group allows early recognition of IAH/ACS and consequently, timely intervention, which can have a striking effect and fully restore homeostasis. Although the progress made in recent years is significant, there are still open questions which leaves room for future research.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Poland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Oprea V S-Editor: Gao CC L-Editor: Filipodia P-Editor: Gao CC
| 1. | Ball CG, Kirkpatrick AW, McBeth P. The secondary abdominal compartment syndrome: not just another post-traumatic complication. Can J Surg. 2008;51:399-405. [PubMed] |
| 2. | Malbrain ML, Chiumello D, Pelosi P, Wilmer A, Brienza N, Malcangi V, Bihari D, Innes R, Cohen J, Singer P, Japiassu A, Kurtop E, De Keulenaer BL, Daelemans R, Del Turco M, Cosimini P, Ranieri M, Jacquet L, Laterre PF, Gattinoni L. Prevalence of intra-abdominal hypertension in critically ill patients: a multicentre epidemiological study. Intensive Care Med. 2004;30:822-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 350] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 3. | Kimball EJ, Kim W, Cheatham ML, Malbrain ML. Clinical awareness of intra-abdominal hypertension and abdominal compartment syndrome in 2007. Acta Clin Belg. 2007;62 Suppl 1:66-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Cheatham ML. Abdominal compartment syndrome: pathophysiology and definitions. Scand J Trauma Resusc Emerg Med. 2009;17:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 125] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 5. | Malbrain ML, Cheatham ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppäniemi A, Olvera C, Ivatury R, D'Amours S, Wendon J, Hillman K, Johansson K, Kolkman K, Wilmer A. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med. 2006;32:1722-1732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 952] [Cited by in RCA: 863] [Article Influence: 45.4] [Reference Citation Analysis (2)] |
| 6. | Smit M, Koopman B, Dieperink W, Hulscher JBF, Hofker HS, van Meurs M, Zijlstra JG. Intra-abdominal hypertension and abdominal compartment syndrome in patients admitted to the ICU. Ann Intensive Care. 2020;10:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Reintam Blaser A, Regli A, De Keulenaer B, Kimball EJ, Starkopf L, Davis WA, Greiffenstein P, Starkopf J; Incidence, Risk Factors, and Outcomes of Intra-Abdominal (IROI) Study Investigators. Incidence, Risk Factors, and Outcomes of Intra-Abdominal Hypertension in Critically Ill Patients-A Prospective Multicenter Study (IROI Study). Crit Care Med. 2019;47:535-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 110] [Article Influence: 18.3] [Reference Citation Analysis (1)] |
| 8. | Murtaza G, Pal KM, Jajja MR, Nawaz Z, Koondhar R, Nasim S. Intra abdominal hypertension; incidence, prevalence and outcomes in a mixed intensive care unit: Prospective cohort study. Int J Surg. 2015;19:67-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Holodinsky JK, Roberts DJ, Ball CG, Blaser AR, Starkopf J, Zygun DA, Stelfox HT, Malbrain ML, Jaeschke RC, Kirkpatrick AW. Risk factors for intra-abdominal hypertension and abdominal compartment syndrome among adult intensive care unit patients: a systematic review and meta-analysis. Crit Care. 2013;17:R249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 136] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 10. | Blaser AR, Björck M, De Keulenaer B, Regli A. Abdominal compliance: A bench-to-bedside review. J Trauma Acute Care Surg. 2015;78:1044-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Malbrain ML, Roberts DJ, De Laet I, De Waele JJ, Sugrue M, Schachtrupp A, Duchesne J, Van Ramshorst G, De Keulenaer B, Kirkpatrick AW, Ahmadi-Noorbakhsh S, Mulier J, Ivatury R, Pracca F, Wise R, Pelosi P. The role of abdominal compliance, the neglected parameter in critically ill patients - a consensus review of 16. Part 1: definitions and pathophysiology. Anaesthesiol Intensive Ther. 2014;46:392-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Caldwell CB, Ricotta JJ. Changes in visceral blood flow with elevated intraabdominal pressure. J Surg Res. 1987;43:14-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 208] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 13. | Diebel LN, Wilson RF, Dulchavsky SA, Saxe J. Effect of increased intra-abdominal pressure on hepatic arterial, portal venous, and hepatic microcirculatory blood flow. J Trauma. 1992;33:279-82; discussion 282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 246] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 14. | Luca A, Cirera I, García-Pagán JC, Feu F, Pizcueta P, Bosch J, Rodés J. Hemodynamic effects of acute changes in intra-abdominal pressure in patients with cirrhosis. Gastroenterology. 1993;104:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 75] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Richardson JD, Trinkle JK. Hemodynamic and respiratory alterations with increased intra-abdominal pressure. J Surg Res. 1976;20:401-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 205] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Ridings PC, Bloomfield GL, Blocher CR, Sugerman HJ. Cardiopulmonary effects of raised intra-abdominal pressure before and after intravascular volume expansion. J Trauma. 1995;39:1071-1075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 175] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Obeid F, Saba A, Fath J, Guslits B, Chung R, Sorensen V, Buck J, Horst M. Increases in intra-abdominal pressure affect pulmonary compliance. Arch Surg. 1995;130:544-7; discussion 547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 91] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Aprahamian C, Wittmann DH, Bergstein JM, Quebbeman EJ. Temporary abdominal closure (TAC) for planned relaparotomy (etappenlavage) in trauma. J Trauma. 1990;30:719-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 76] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Mullens W, Abrahams Z, Skouri HN, Francis GS, Taylor DO, Starling RC, Paganini E, Tang WH. Elevated intra-abdominal pressure in acute decompensated heart failure: a potential contributor to worsening renal function? J Am Coll Cardiol. 2008;51:300-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 297] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 20. | Mullens W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, Young JB, Tang WHW. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009;53:589-596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1323] [Cited by in RCA: 1180] [Article Influence: 73.8] [Reference Citation Analysis (0)] |
| 21. | Talizin TB, Tsuda MS, Tanita MT, Kauss IAM, Festti J, Carrilho CMDM, Grion CMC, Cardoso LTQ. Acute kidney injury and intra-abdominal hypertension in burn patients in intensive care. Rev Bras Ter Intensiva. 2018;30:15-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Smit M, van Meurs M, Zijlstra JG. Intra-Abdominal Pressure, Acute Kidney Injury, and Obesity in Critical Illness. Crit Care Med. 2016;44:e766-e767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Stone HH, Fulenwider JT. Renal decapsulation in the prevention of post-ischemic oliguria. Ann Surg. 1977;186:343-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 24. | Le Roith D, Bark H, Nyska M, Glick SM. The effect of abdominal pressure on plasma antidiuretic hormone levels in the dog. J Surg Res. 1982;32:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 48] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Nguyen VQ, Gadiraju TV, Patel H, Park M, Le Jemtel TH, Jaiswal A. Intra-abdominal Hypertension: An Important Consideration for Diuretic Resistance in Acute Decompensated Heart Failure. Clin Cardiol. 2016;39:37-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Mullens W, Damman K, Harjola VP, Mebazaa A, Brunner-La Rocca HP, Martens P, Testani JM, Tang WHW, Orso F, Rossignol P, Metra M, Filippatos G, Seferovic PM, Ruschitzka F, Coats AJ. The use of diuretics in heart failure with congestion - a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21:137-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 696] [Article Influence: 116.0] [Reference Citation Analysis (0)] |
| 27. | Harman PK, Kron IL, McLachlan HD, Freedlender AE, Nolan SP. Elevated intra-abdominal pressure and renal function. Ann Surg. 1982;196:594-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 347] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 28. | Reintam A, Parm P, Kitus R, Starkopf J, Kern H. Gastrointestinal failure score in critically ill patients: a prospective observational study. Crit Care. 2008;12:R90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 151] [Cited by in RCA: 149] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 29. | Lima R, Silva PL, Capelozzi VL, Oliveira MG, Santana MCE, Cruz FF, Pelosi P, Schanaider A, Malbrain MLNG, Rocco PRM. Early impact of abdominal compartment syndrome on liver, kidney and lung damage in a rodent model. Anaesthesiol Intensive Ther. 2017;49:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Luce JM, Huseby JS, Kirk W, Butler J. Mechanism by which positive end-expiratory pressure increases cerebrospinal fluid pressure in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1982;52:231-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 31. | Bloomfield GL, Dalton JM, Sugerman HJ, Ridings PC, DeMaria EJ, Bullock R. Treatment of increasing intracranial pressure secondary to the acute abdominal compartment syndrome in a patient with combined abdominal and head trauma. J Trauma. 1995;39:1168-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 88] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 32. | Malbrain ML. Different techniques to measure intra-abdominal pressure (IAP): time for a critical re-appraisal. Intensive Care Med. 2004;30:357-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 308] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 33. | De Waele JJ, De Laet I, Malbrain ML. Rational intraabdominal pressure monitoring: how to do it? Acta Clin Belg. 2007;62 Suppl 1:16-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 34. | Hunt L, Frost SA, Hillman K, Newton PJ, Davidson PM. Management of intra-abdominal hypertension and abdominal compartment syndrome: a review. J Trauma Manag Outcomes. 2014;8:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | Lopes AM, Morgado M, Niza MMRE, Franca N, Mestrinho L, Félix N, Dourado A. Biophysical Validation of Intra- Abdominal Pressure and Transurethral Method. J Vet Sci Med Diagn. 2016;5. [DOI] [Full Text] |
| 36. | Zymliński R, Biegus J, Sokolski M, Jankowska EA, Banasiak W, Ponikowski P. Validation of transurethral intraabdominal pressure measurement in acute heart failure. Pol Arch Intern Med. 2018;128:403-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Milanesi R, Caregnato RC. Intra-abdominal pressure: an integrative review. Einstein (Sao Paulo). 2016;14:423-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 38. | Ertel W, Oberholzer A, Platz A, Stocker R, Trentz O. Incidence and clinical pattern of the abdominal compartment syndrome after "damage-control" laparotomy in 311 patients with severe abdominal and/or pelvic trauma. Crit Care Med. 2000;28:1747-1753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 180] [Article Influence: 7.2] [Reference Citation Analysis (0)] |