Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.381
Peer-review started: August 21, 2021
First decision: September 29, 2021
Revised: October 29, 2021
Accepted: November 30, 2021
Article in press: November 30, 2021
Published online: January 7, 2022
Processing time: 130 Days and 17.8 Hours
Primary melanomas affecting the central nervous system are very rare, and melanomas originating in the spinal canal or origin of the spinal nerve root are even rarer. As a consequence, not much is known about this.
Here we report a case of primary malignant melanoma originating in the cervical spinal cord nerve root. A 64-year-old woman presented with symptoms of numbness in the right side of the neck, pain, and hypoesthesia in the right upper limb which persisted for 1 year. Neurological examination showed that the superficial sensation in the right upper limb had decreased with muscle strength of grade 4. Magnetic resonance imaging examination revealed a mass (approximately 2.5 cm × 1.4 cm × 1 cm) in the right side of the spinal canal in the C-2 plane. Based on findings obtained during operation, perioperative examination, pathological diagnosis, and the diagnostic criteria of primary central melanoma proposed by Hayward, the mass was confirmed to be a melanoma of intraspinal nerve root origin.
This is the first case of primary malignant melanoma originating from cervical spinal cord nerve roots and spread along the inside and outside of the spinal canal. The clinical relevance of this case is discussed to provide new insights into the differential diagnosis of intraspinal tumours. Further studies are needed to better understand the mechanisms driving the growth pattern and development of this type of tumour.
Core Tip: Primary malignant melanoma arising from the cervical nerve root, and spreading along the inside and outside regions of the spinal canal is clinically rare. The clinical symptoms and imaging features of this case are atypical and can easily be misdiagnosed. In this case report, additional clinical characteristics and differential diagnoses are presented.
- Citation: Shi YF, Chen YQ, Chen HF, Hu X. An atypical primary malignant melanoma arising from the cervical nerve root: A case report and review of literture. World J Clin Cases 2022; 10(1): 381-387
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/381.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.381
Primary central nervous system melanomas are very rare, and account for about 1% of all melanomas[1]. In addition, primary malignant melanoma in the spinal canal is even rarer with only several cases reported so far[2]. Majority of such cases show nerve root involvement. Herein, we present an unusual case of primary malignant melanoma originating from the nerve root in the spinal canal without a history of irradiation exposure. To date, there have been only 5 similar cases[3,4]. However, as far as we know, the patient described in this report presents the first case of primary malignant melanoma in which the growth occurs along the inside and outside of the spinal canal.
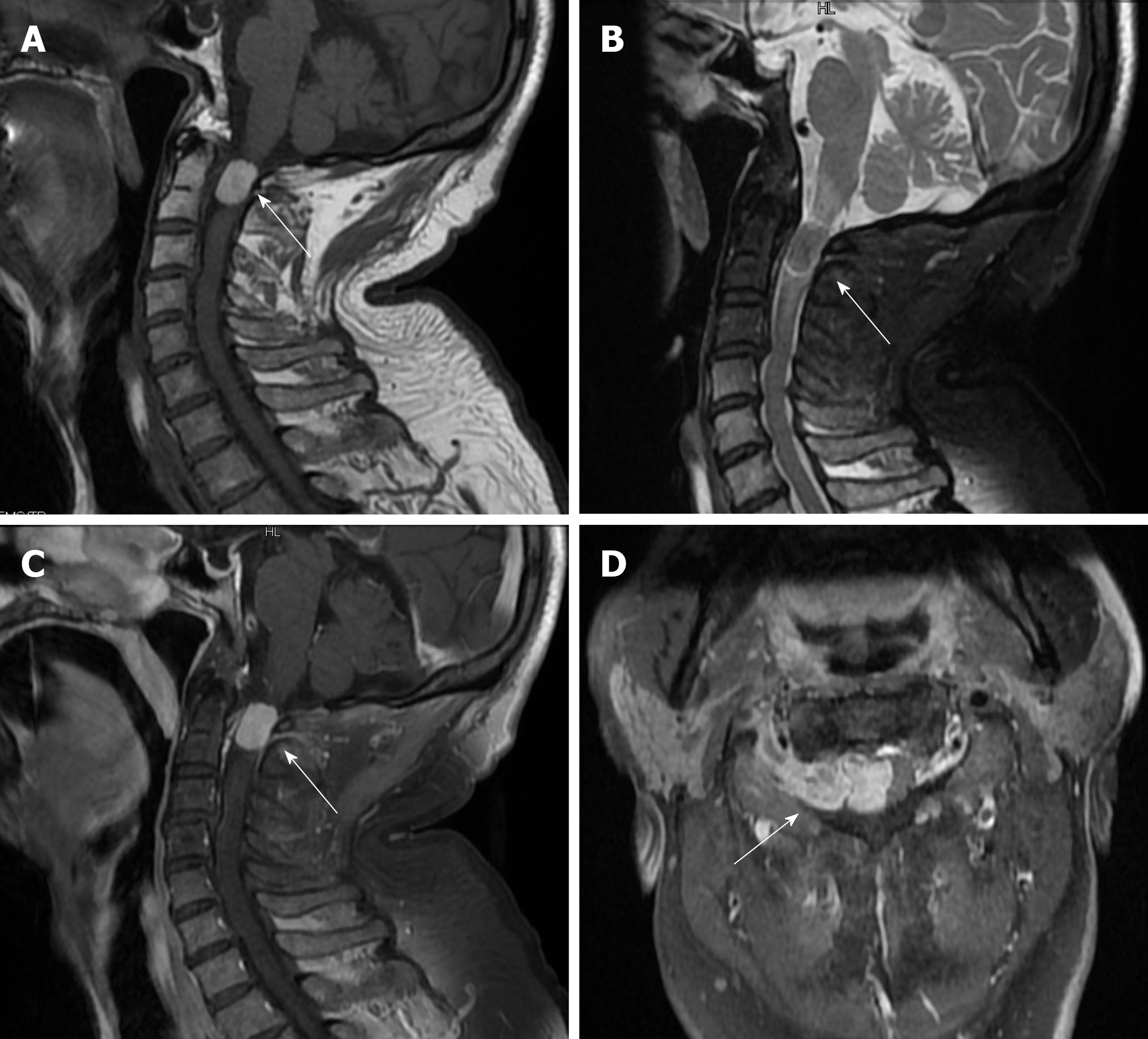
Magnetic resonance imaging (MRI) examination showed a mass (approximately 2.5 cm × 1.4 cm × 1 cm) in the right side of the spinal canal in the C-2 plane. The mass exhibited high signal intensity on T1-weighted images and isointense on T2-weighted images. The signal intensity did not vary significantly between the T1-weighted images after contrast enhancement. The boundary was clear and spinal cord appeared significantly compressed and displaced to the left side (Figure 1). Results shown in Figure 1D indicate that the tumour extended beyond the intervertebral foramen to the outside of the spinal canal.
Her preoperative laboratory examination, electrocardiogram, and lung computerized tomography (CT) findings were normal.
Neurological examination showed that the superficial sensation in the right upper limb had decreased accompanied by a muscle strength of grade 4. A general examination did not find any subcutaneous nodules or skin lesions.
No positive personal or family history.
The patient had no previous medical history or a family history of malignant melanoma. She denied having any previous irradiation exposure.
The patient presented with progressive numbness in the right side of the neck, pain, and hypoesthesia in the right upper limb that occurred in the previous 1 year.
A 64-year-old woman was admitted to our hospital with numbness in the right side of the neck, pain, and hypoesthesia in the right upper limb which persisted for 1 year.
None.
Based on the findings obtained during operation, perioperative examination, pathological diagnosis, and the diagnostic criteria of primary central melanoma proposed by Hayward, the neoplasm was considered to be a melanoma of intraspinal nerve root origin with an atypical growth pattern.
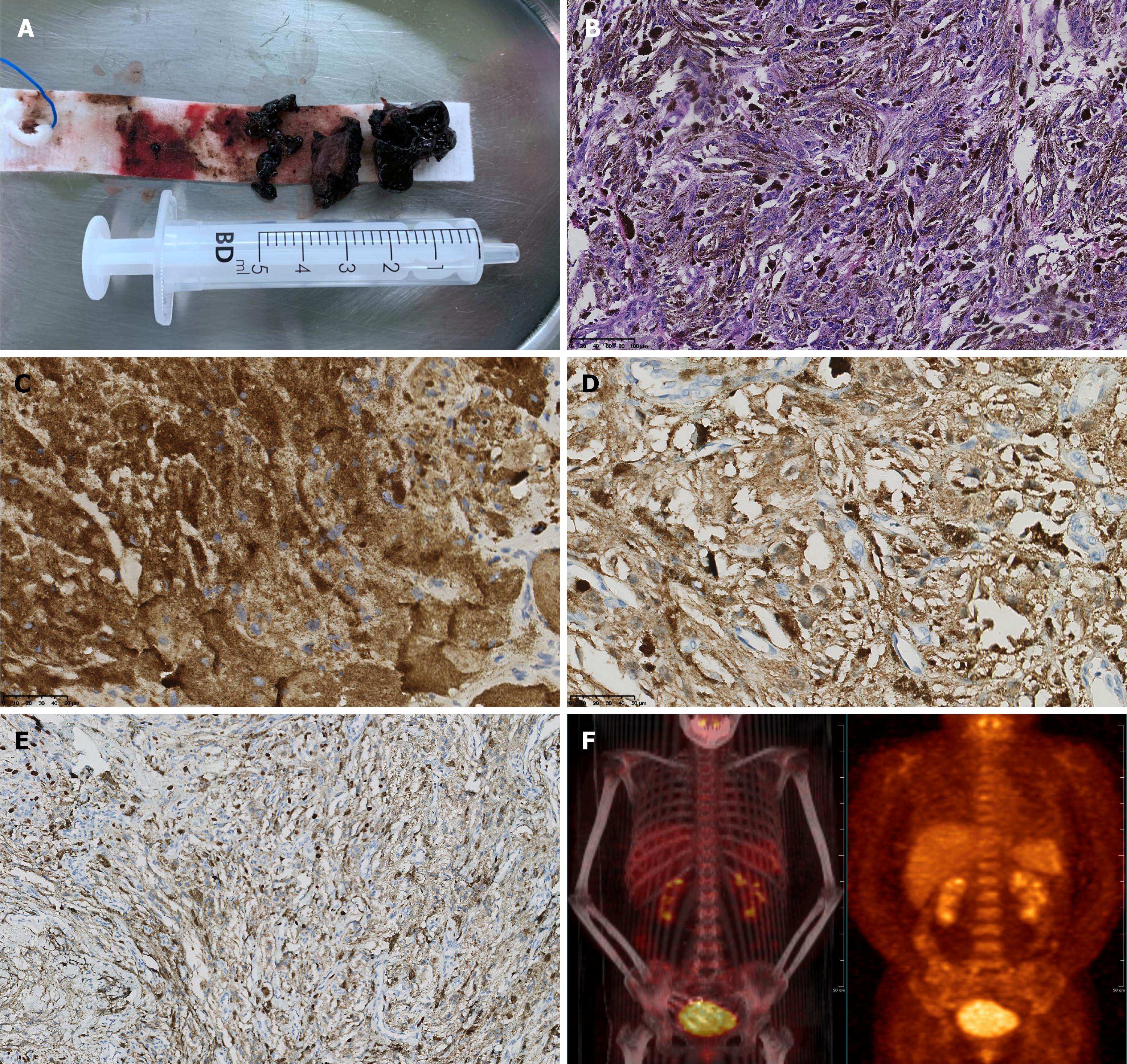
We adopted the posterior median approach which allowed us to successfully remove the tumour. During the operation, the subdural region appeared black. After opening the dura mater, a black object was seen wrapped in a membranous structure close to the nerve root. The object grew out of the spinal canal through the intervertebral foramen. The lesion was close to the pia mater surface of the spinal cord. However, it was clearly demarcated with spinal cord tissue and pia mater. It had a tough and solid texture, with little blood supply, and did not invade the dura mater (Figure 2A).
After operation, no postoperative neurological deficits were observed and postoperative pathological diagnosis confirmed malignant melanoma (Figure 2B-2E). A follow-up positron emission tomography/CT scan (Figure 2F) 1 mo after surgery showed total excision and no signs of metastasis and residual tumour. The postoperative course was uneventful, and the patient was discharged on the 14th day. At the last telephone follow-up in October 2021, the patient reported having no issues. We believe that her condition is stable based on routine follow-up MRIs.
Primary spinal cord melanoma is a very rare entity. Primary melanoma of the CNS originates from aberrant changes in pigment cells of the neural crest or from melanocytic elements of the pia mater during early embryonic development[5,6]. The clinical presentation of this condition varies from person to person, depending on the location of the tumour[7]. Primary spinal melanomas have been reported in different regions including intramedullary, intradural, and extradural lesions[8]. Most of such cases occur within the cervical and thoracic cord[9]. We retrospectively analysed 70 cases of primary spinal malignant melanoma between 1930 and 2021 on the PubMed Medline database. It was observed that tumours that grow from the inside to the outside of spinal canal are very rare (Table 1).
| Tumor feature | Number of patients |
| Growth pattern | |
| Communicating the intervertebral Foramen | 1 |
| Extradural | 5 |
| Intradural-extramedullary | 33 |
| Intradural-intra-and extra-medullary | 4 |
| Intramedullary | 22 |
| Other | 5 |
| Location | |
| Cervical | 24 |
| Thoracic | 33 |
| Lumbar | 10 |
| Sacral | 3 |
In terms of clinical manifestation, the most common initial symptom of spinal schwannoma is pain, followed by loss of nerve function[9]. In our case, symptoms of nerve root stimulation were pronounced before operation, which matched the typical clinical manifestations of spinal schwannoma. For the spinal Schwannoma, MRI imaging shows a dumbbell shape and widening of intervertebral foramen[10]. In our case, this growth pattern was first seen in the spinal melanoma. Using MRI, the primary imaging modality used for evaluation of spinal neoplasm[11], the signal of this lesion emerged from under the epidural of spinal cord, as in the case of schwannoma and meningioma[10]. Besides, most of these lesions show signal hyperintensity on T1-weighted images[8,11], rarely iso-intensity on T2-weighted images[12,13], as well as mild to moderate homogenous enhancement[14,15]. It should be that the MRI signal of the lesion showed signal hyperintensity on T1 weighted image and equal signal on T2. The signal intensity after enhancement was not significantly different from that on T1-weighted images. It has been postulated that a higher blood supply in a lesion yields a higher signal intensity after enhancement[16]. The signal hyperintensity on T1-weighted image was due to the concentration of melanin, haemorrhages, and fat deposits[17,18]. The signal characteristics of MRI may easily lead to misdiagnosis. It is important for surgeons to make an accurate diagnosis and be aware of the limitations of the diagnostic value of MRI. For instance, enhanced MRI revealed a pronounced dural tail sign, which is a classic characteristic of meningioma. However, T1-weighted images with hyperintensity and T2-weighted images with hypointensity are typical features for melanoma, and atypical for meningioma. In addition, intra-tumoral bleeding may cause uneven hyper-intensive signal in T1weighted images. However, it has been reported that enhancement scan of melanoma originating from intramedullary melanoma will be significantly enhanced. Moreover, if there is bleeding in the tumour, the signal will show mixed density[19].
Moreover, blood supply within a tumour seen during the operation was not abundant. As a consequence, we hypothesized that there was no obvious enhancement in the enhanced scan of melanoma originating from the nerve root. These factors make the preoperative diagnosis of atypical cases difficult, and our case reveals the diverse growth patterns associated the imaging findings of primary central nervous system melanoma. This is extremely important for the design of surgical strategies[20]. Thus, when making a preoperative diagnosis based on neuroimaging and clinical experience, there is need to make a more comprehensive prediction of the benign and malignant lesions before preventive measures are applied during operation and the tumour is excised. This only prevents metastasis and influences prognosis of patients.
In most melanomas occurring in the spine, they have primary lesions or metastases in other parts of the spine[21]. Therefore, the present case adds to the understanding on such melanomas. Notably, the positive rate of Ki-67 index in the postoperative pathological examination of present case was more than 20%. In theory, cancer cells of this case will proliferate rapidly and are likely to metastasize[22,23]. However, patients didn’t receive radiotherapy and chemotherapy. No recurrence or metastasis was found during follow-up, indicating that the primary malignant melanoma originating from the nerve root may have different biological characteristics[24], or such tumours have a better prognosis than do cutaneous melanomas[25]. As a consequence, the primary malignant melanoma in the spinal canal may be less invasive than in other parts. which require more evidence-based medicine from the clinical experience. The choice of treatment[26,27] for such cases is extremely important. Gross total resection has been shown to results in longer progression-free survival and survival compared with no or partial resection[28,29]. Because the gross total resection of the tumour result in good outcomes and a longer longevity[30,31]. Nevertheless, the efficacy of post
In the present report, we present the first case of a primary malignant melanoma originating from the cervical spinal cord nerve roots and grew from the inside to the outside of the spinal canal. Unlike most primary melanomas of the spinal canal, this case has an unusual tumour origin, growth pattern, and imaging findings. Therefore, it provides new insights into the understanding and differential diagnosis of intraspinal tumours. Further studies are needed to reveal the mechanisms driving the development and growth pattern of such a tumour.
The authors thank the staff (Department of Neurosurgery, West China Hospital) engaged in the surgery and clinical care of the patient.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Neurosciences
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Almzeogi MA, Velikova TV S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Puyana C, Denyer S, Burch T, Bhimani AD, McGuire LS, Patel AS, Mehta AI. Primary Malignant Melanoma of the Brain: A Population-Based Study. World Neurosurg. 2019;130:e1091-e1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Zhang M, Liu R, Xiang Y, Mao J, Li G, Ma R, Sun Z. Primary Spinal Cord Melanoma: A Case Report and a Systemic Review of Overall Survival. World Neurosurgery. 2018;114:408-420. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Lee CH, Moon KY, Chung CK, Kim HJ, Chang KH, Park SH, Jahng TA. Primary intradural extramedullary melanoma of the cervical spinal cord: case report. Spine (Phila Pa 1976). 2010;35:E303-E307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Zou C, Cheng W, Zhu C, Guo Q, Wu A. Primary Extradural Melanoma Arising in Cervical Spinal Nerve Root. World Neurosurg. 2018;111:211-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | PAPPENHEIM E, BHATTACHARJI SK. Primary melanoma of the central nervous system. Clinical-pathological report of a case, with survey and discussion of the literature. Arch Neurol. 1962;7:101-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Yamasaki T, Kikuchi H, Yamashita J, Asato R, Fujita M. Primary spinal intramedullary malignant melanoma: case report. Neurosurgery. 1989;25:117-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Vij M, Jaiswal S, Jaiswal AK, Behari S. Primary spinal melanoma of the cervical leptomeninges: report of a case with brief review of literature. Neurol India. 2010;58:781-783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Farrokh D, Fransen P, Faverly D. MR findings of a primary intramedullary malignant melanoma: case report and literature review. AJNR Am J Neuroradiol. 2001;22:1864-1866. [PubMed] |
| 9. | Tuz Zahra F, Ajmal Z, Qian J, Wrzesinski S. Primary Intramedullary Spinal Melanoma: A Rare Disease of the Spinal Cord. Cureus. 2021;13:e16194. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Olex-Zarychta D. Clinical Significance of Pain in Differential Diagnosis between Spinal Meningioma and Schwannoma. Case Rep Oncol Med. 2020;2020:7947242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Jaiswal S, Vij M, Tungria A, Jaiswal AK, Srivastava AK, Behari S. Primary melanocytic tumors of the central nervous system: a neuroradiological and clinicopathological study of five cases and brief review of literature. Neurol India. 2011;59:413-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Kounin GK, Romansky KV, Traykov LD, Shotekov PM, Stoilova DZ. Primary spinal melanoma with bilateral papilledema. Clin Neurol Neurosurg. 2005;107:525-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Lee NK, Lee BH, Hwang YJ, Sohn MJ, Chang S, Kim YH, Cha SJ, Cho HJ. Findings from CT, MRI, and PET/CT of a primary malignant melanoma arising in a spinal nerve root. European spine journal. 2010;19:174-178. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Kinnen F, Fleck S, Baldauf J, Hans V, Daeschlein G, Rathmann E, Schroeder HWS, Marx S. Primary leptomeningeal melanocytic tumors of the spine: report of two cases and review of the literature. World neurosurgery. 2019;124:228-236. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Kanatas AN, Bullock MD, Pal D, Chakrabarty A, Chumas P. Intradural extramedullary primary malignant melanoma radiographically mimicking a neurofibroma. Br J Neurosurg. 2007;21:39-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Unal B, Castillo M. MRI features of a primary thoracic epidural melanoma: a case report. Clin Imaging. 2007;31:273-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Smith A, Rushing E, Smirniotopoulos J. Pigmented lesions of the central nervous system: radiologic-pathologic correlation. Radiographics. 2009;29:1503-1524. [RCA] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 18. | Isiklar I, Leeds NE, Fuller GN, Kumar AJ. Intracranial metastatic melanoma: correlation between MR imaging characteristics and melanin content. AJR Am J Roentgenol. 1995;165:1503-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 120] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Chatterjee R, Nascimento FA, Heck KA, Ropper AE, Sabichi AL. Primary Spinal Cord Melanoma - An Uncommon Entity. Can J Neurol Sci. 2019;46:348-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Larson TC 3rd, Houser OW, Onofrio BM, Piepgras DG. Primary spinal melanoma. J Neurosurg. 1987;66:47-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Haberfellner E, Elbaroody M, Alkhamees AF, Alaosta A, Eaton S, Quint E, Shahab S, O'Connor A, Im J, Khan A, El-Gohary Y, Lotfy M, Sawan M, Shamisa A, Soliman MAR. Primary Spinal Melanoma: Case Report and Systematic Review. Clin Neurol Neurosurg. 2021;205:106649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Asi-Bautista MC, Heidemann SM, Meert KL, Canady AI, Sarnaik AP. Tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-6 concentrations in cerebrospinal fluid predict ventriculoperitoneal shunt infection. Crit Care Med. 1997;25:1713-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Schöder H, Larson S, Yeung H. PET/CT in oncology: integration into clinical management of lymphoma, melanoma, and gastrointestinal malignancies. J Nucl Med. 2004;45:72S-81S. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 24. | Sanz-Trelles A, Arranz-Salas IM, Valenzuela-Serrano MI. Melanoma arising in and limited to a spinal nerve root of the cauda equina. Histopathology. 2003;43:603-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Brat DJ, Giannini C, Scheithauer BW, Burger PC. Primary melanocytic neoplasms of the central nervous systems. Am J Surg Pathol. 1999;23:745-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 213] [Cited by in RCA: 206] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 26. | Balakrishnan R, Porag R, Asif DS, Satter AM, Taufiq M, Gaddam SS. Primary Intracranial Melanoma with Early Leptomeningeal Spread: A Case Report and Treatment Options Available. Case Rep Oncol Med. 2015;2015:293802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Fujimori K, Sakai K, Higashiyama F, Oya F, Maejima T, Miyake T. Primary central nervous system malignant melanoma with leptomeningeal melanomatosis: a case report and review of the literature. Neurosurg Rev. 2018;41:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Salpietro FM, Alafaci C, Gervasio O, La Rosa G, Baio A, Francolini DC, Batolo D, Tomasello F. Primary cervical melanoma with brain metastases. Case report and review of the literature. J Neurosurg. 1998;89:659-666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Yu J, Zhao DD, Chen S, Zhang JM, Xu J. Primary melanoma of the cervical spine with cerebral metastases: case report and review of the literature. J Int Med Res. 2012;40:1207-1215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Marx S, Fleck SK, Manwaring J, Vogelgesang S, Langner S, Schroeder HW. Primary leptomeningeal melanoma of the cervical spine mimicking a meningioma-a case report. J Neurol Surg Rep. 2014;75:e93-e97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Wu L, Yao N, Fang J, Yang J, Xu Y. Clinical features and long-term outcomes of primary spinal malignant melanoma: a single center experience. J Neurooncol. 2017;135:513-519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Patchell R, Tibbs P, Regine W, Payne R, Saris S, Kryscio RJ, Mohiuddin M, Young B. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet (London, England). 2005;366:643-648. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1662] [Cited by in RCA: 1510] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 33. | Fuld AD, Speck ME, Harris BT, Simmons NE, Corless CL, Tsongalis GJ, Pastel DA, Hartford AC, Ernstoff MS. Primary melanoma of the spinal cord: a case report, molecular footprint, and review of the literature. J Clin Oncol. 2011;29:e499-502. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |