Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.331
Peer-review started: July 8, 2021
First decision: October 16, 2021
Revised: October 25, 2021
Accepted: November 26, 2021
Article in press: November 26, 2021
Published online: January 7, 2022
Processing time: 175 Days and 6.5 Hours
Lunate dislocation is an uncommon traumatic wrist injury that require prompt surgical management. Misdiagnosis or delayed treatment often leads to a poor outcome. Open reduction and surgical repair of disrupted ligaments are done in most cases to prevent long-term joint dysfunction. However, this method has certain limitations that include partial functional improvement, which poses a high risk for degenerative arthritis and wrist instability.
A 37-year-old man presented to the Emergency Department of our hospital following a motorcycle accident. Physical examination revealed swelling and tenderness of the right hand and wrist. The patient was initially misdiagnosed with a wrist contusion by an emergency physician, but was eventually diagnosed with lunate dislocation associated with a triquetral avulsed fracture, indicated for open reduction and ligament repair. We performed closed reduction and two Kirschner wire fixations following Tavernier’s method. The injured hand was protected with a standard short-arm orthosis for one month. The patient returned to normal daily work without discomfort at five months postoperatively. Encouragingly, there was no lunate necrosis or arthritis in the latest radiologic examinations.
This case provides evidence that the closed reduction technique for addressing such cases can reduce soft tissue destruction.
Core Tip: Lunate fracture dislocation is considered urgent open reduction and surgical repair of disrupted ligaments. However, this method still has certain limitations and can raise a high risk for degenerative arthritis and wrist instability. In this case, it provides evidence that closed reduction technique can reduce soft tissue destruction and minimize the risk of post-traumatic sequelae. Surgeons should attempt to try closed reduction before open reduction in such selected cases.
- Citation: Li LY, Lin CJ, Ko CY. Lunate dislocation with avulsed triquetral fracture: A case report. World J Clin Cases 2022; 10(1): 331-337
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/331.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.331
Lunate dislocations with associated avulsed triquetral bone fracture caused by high energy trauma ae rarely reported. According to literature reviews, 7% of all carpus injuries involve the lunate, of which only 3% are classified as volar lunate dislocations[1,2]. Owing to their rarity, they are often misdiagnosed and may be missed in 25% of cases[3]. The initial presentation is often atypical. To date, there is no consensus regarding the optimal treatment of lunate dislocation. Currently, most authors consider urgent open reduction for the dislocation, repair or reconstruction of the surrounding carpal ligaments and capsules, and fixation with Kirschner wires or screws. We found these surgical options to be frequently associated with complications and unsatisfactory results. Herein, we report a rare case of acute lunate dislocation with triquetral fracture treated by closed reduction with Kirschner wires. The radiological results were encouraging and the patient demonstrated satisfactory function of the wrist joint.
This manuscript follows the CARE guidelines, and written informed consent was obtained from the patient for publication of this manuscript and the accompanying images.
A 37-year-old man presented to the Emergency Department of our hospital with closed injury to the right side of the face and right wrist, and hyper-extension of the wrist. Initially, the patient complained of headache, dizziness, and moderate pain in the right wrist.
The patient symptoms started after a fall from his motor vehicle an hour prior to presentation at the hospital.
The patient had no relevant past medical history.
Non-contributory.
The chin was obviously swollen and deformed, and the right wrist appeared slightly swollen; however, distal pulsation, thumb/finger motion, finger sensation remained normal.
All the blood tests were within normal values.
An emergency physician made the initial diagnosis of fracture of the right mandibular body and contusion of the right wrist at the first survey after radiologic evaluations.
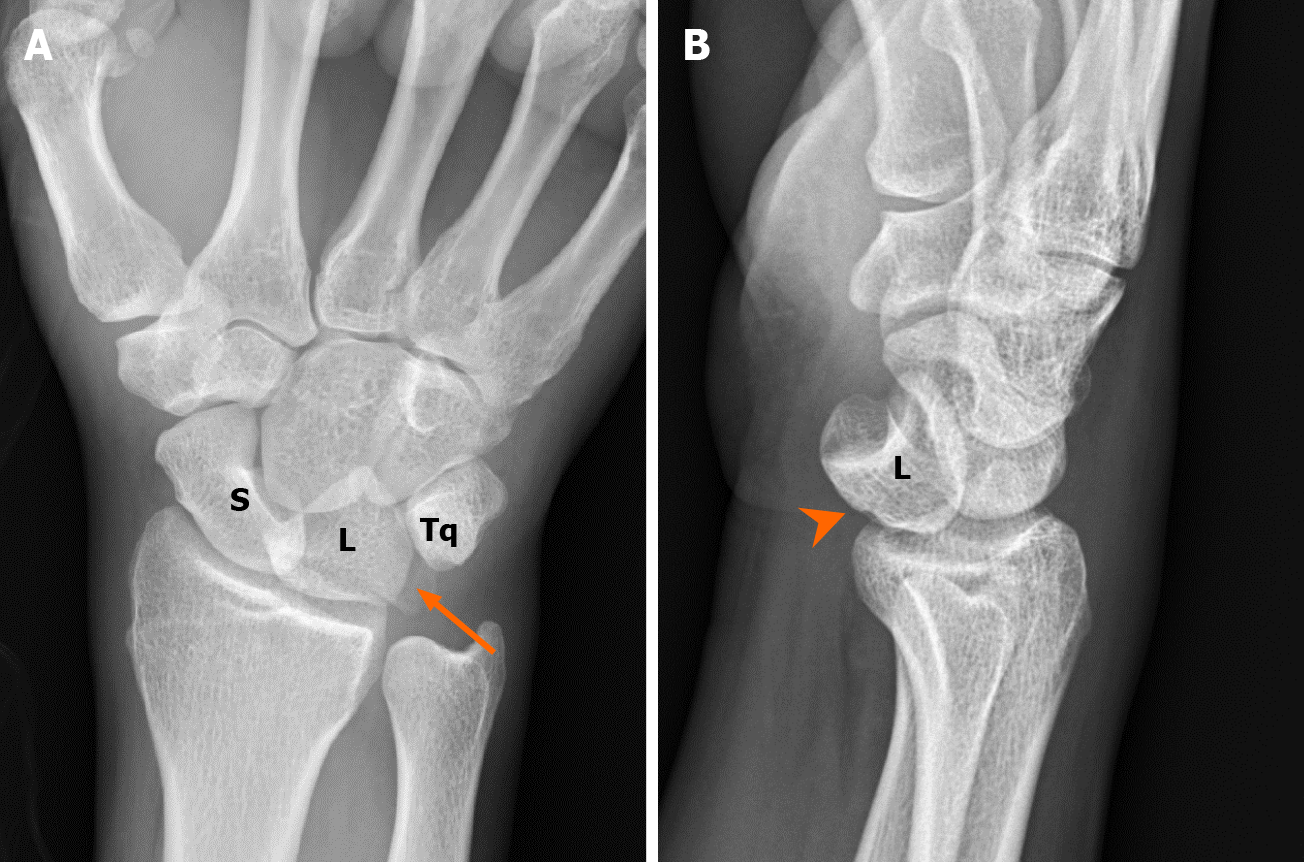
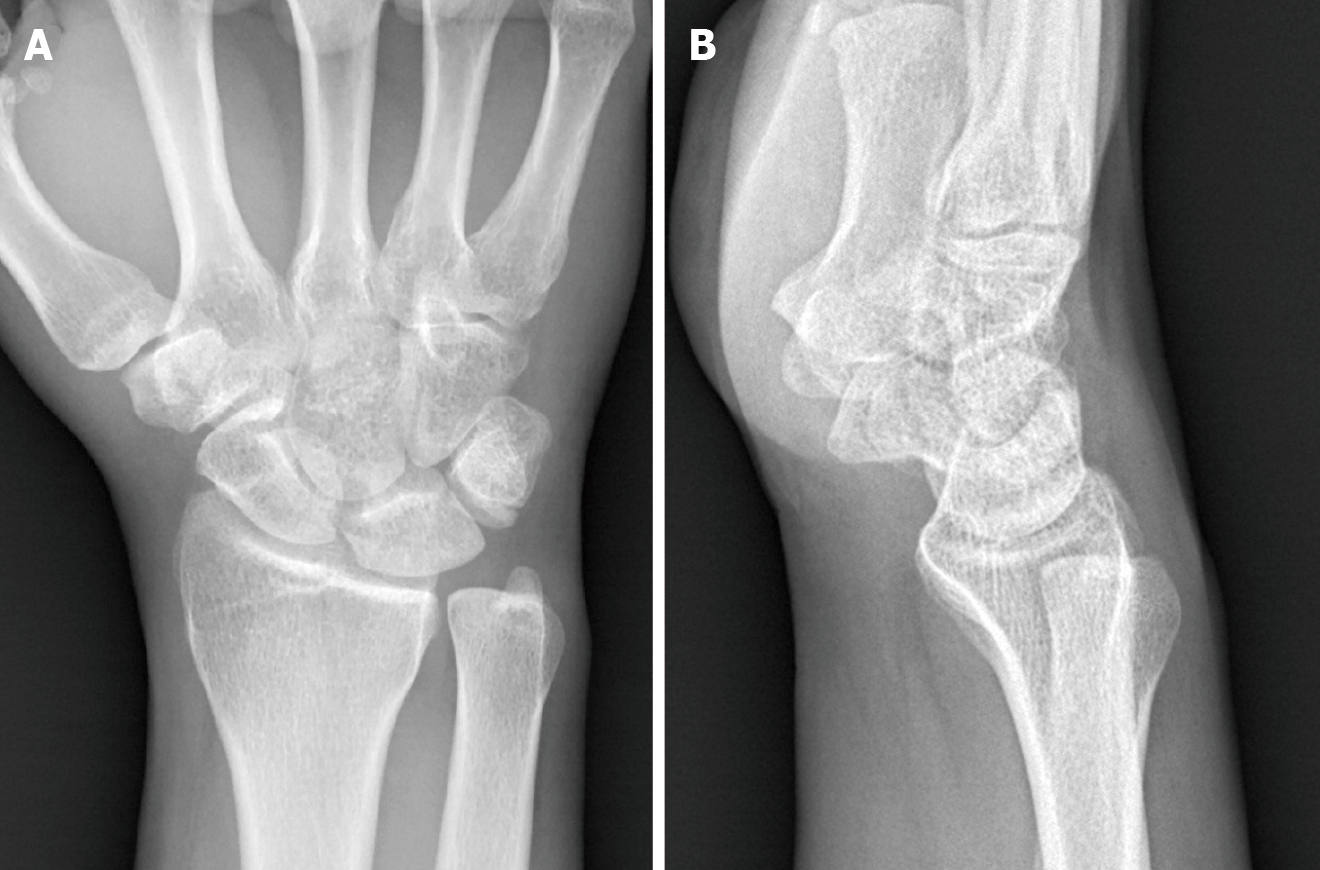
While waiting for facial bone surgery, the swelling and pain in the right wrist increased, with reduction in the range of motion. An orthopedic surgeon was consulted and re-evaluation of the plain radiograph of the right wrist revealed a triangular appearance of the lunate (piece of pie) with triquetral fracture in the anteroposterior view, and angulation and volar displacement of the lunate (spilled tea cup) in the lateral view (Figure 1)[4].
The patient was finally diagnosed with acute lunate volar dislocation with avulsed triquetral fracture. This fracture pattern could be classified as Mayfield classification stage IV[5].
An attempt at closed reduction in the emergency room failed due to excessive swelling of the wrist and inability of the patient to cooperate with the reduction maneuver due to pain. The patient was then scheduled for open reduction and surrounding carpal ligaments repair.
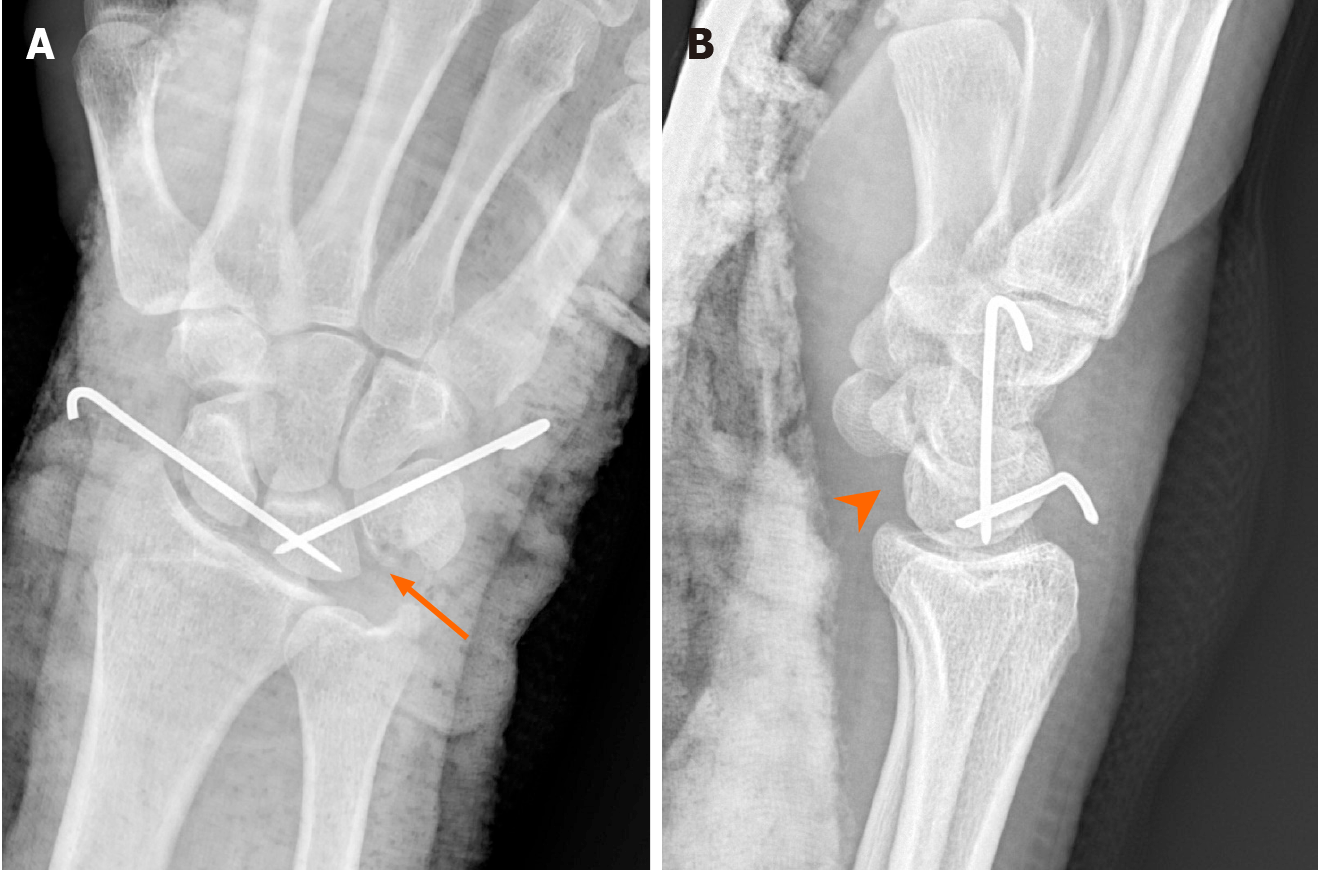
The patient was taken to the operation room approximately 30 h after sustaining trauma. We first tried closed reduction again under general anesthesia using Tavernier’s method, first described in 1906[6]. Fortunately, the dislocated lunate could be reduced with gentle manual traction and slight wrist extension. This was followed by fixation using two Kirschner wires for maintaining reduction (one from the scaphoid to the lunate, and the other from the triquetrum to the lunate). The surgical course was uneventful, and only two pin holes were created (Figure 2). The wrist was immobilized for 4 wk with short arm orthosis and hand therapy for another 8 wk.
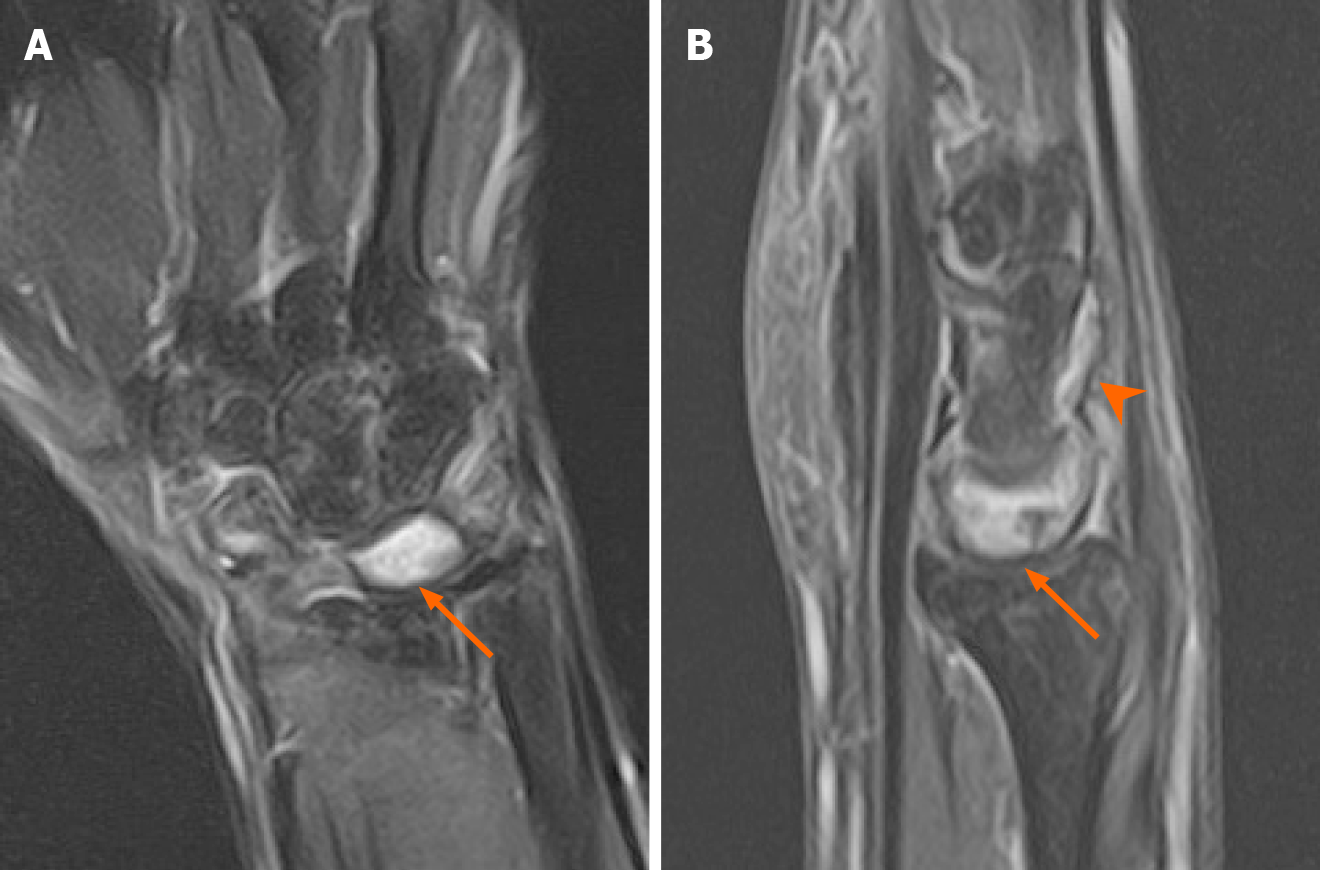
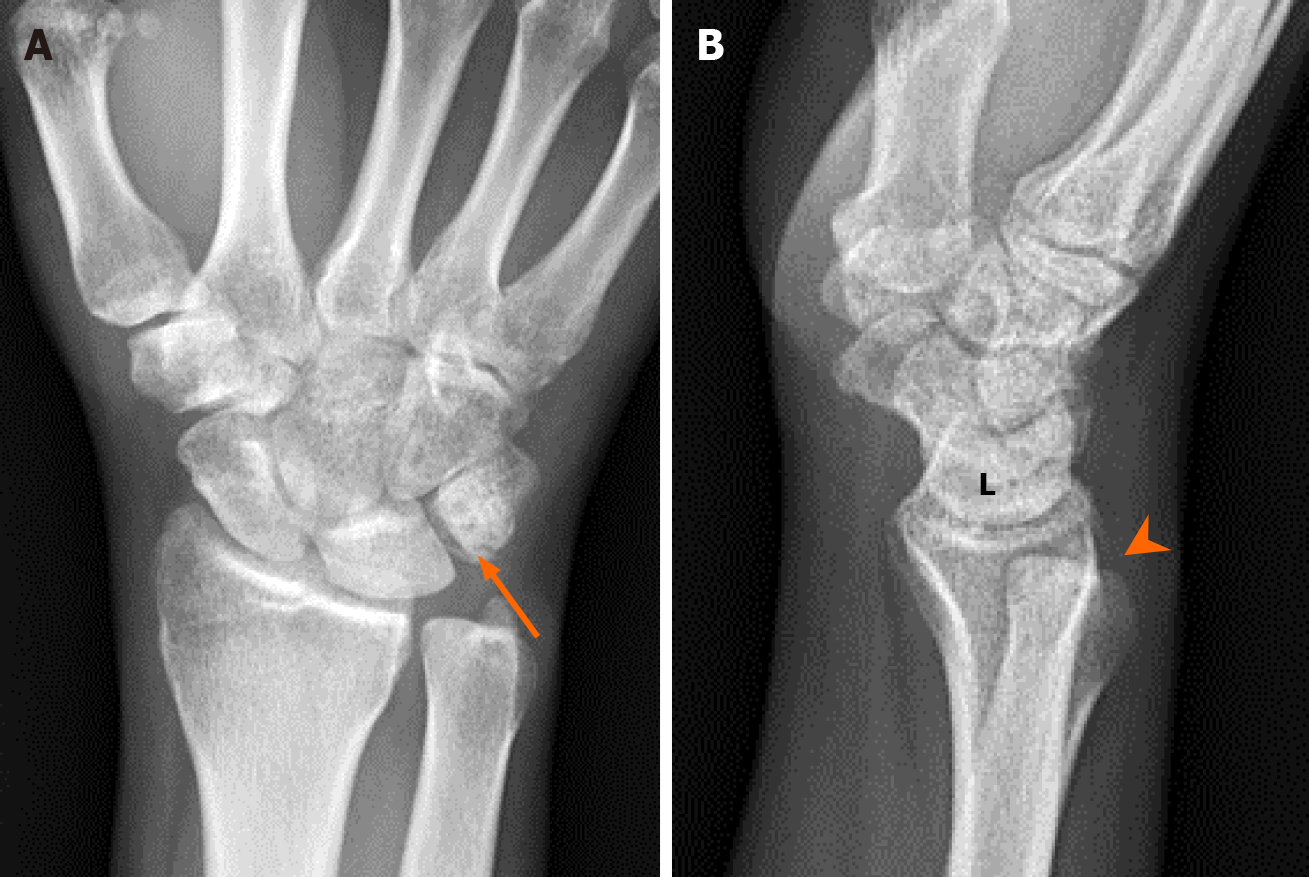
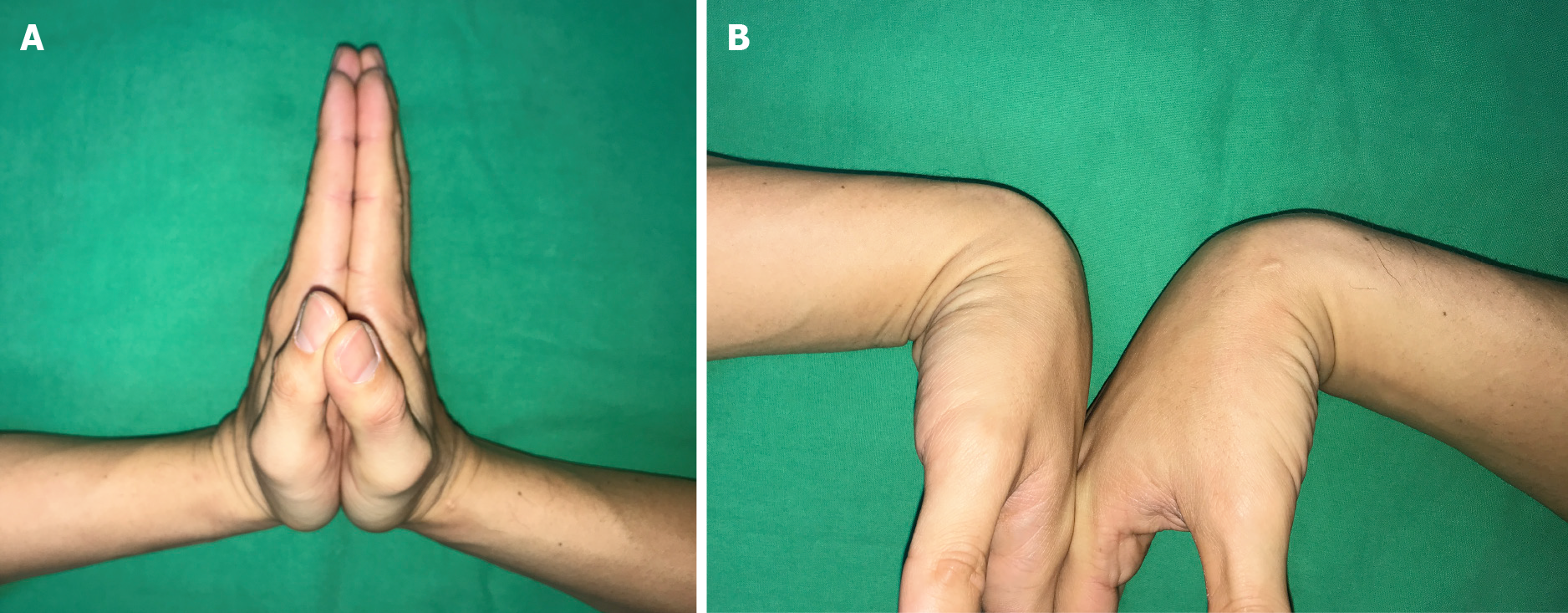
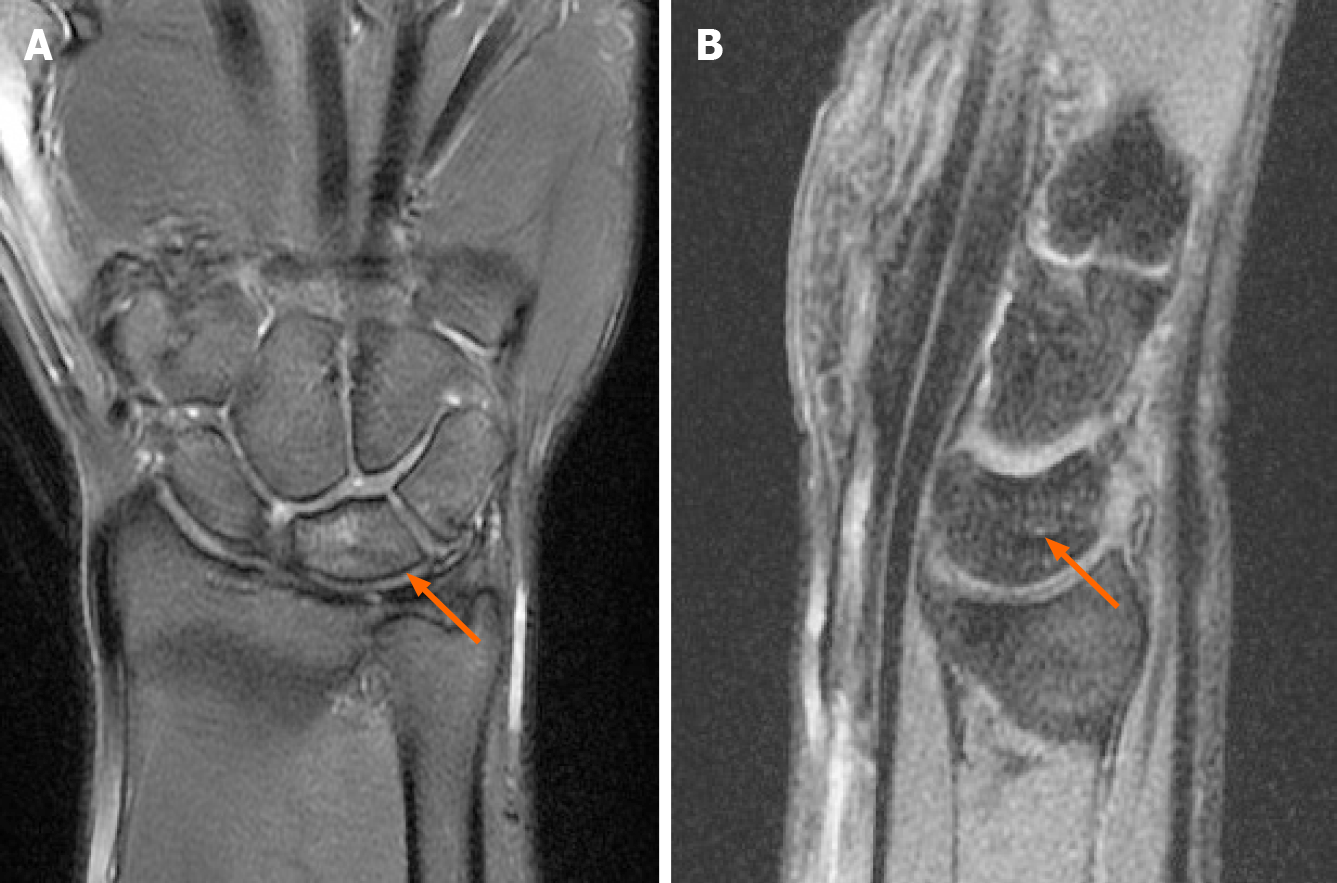
Magnetic resonance imaging (MRI) performed 2 mo postoperatively revealed residual bone marrow edema in the lunate, triquetrum, and scaphoid (Figure 3). Complete bony healing of the triquetrum was confirmed by radiographic examination 20 wk after the trauma (Figure 4). The patient resumed daily activities 24 wk after the trauma. The range of motion of the right wrist was satisfactory with an extension /flexion range of 90°-0°-75°, and pronation/supination range of 90°-0°-90° (Figure 5). The patient experienced no pain at rest, and only reported mild pain related to activity. The movement of the fingers, peripheral sensibility and circulation were fair. There was no avascular necrosis of the lunate, scapholunate instability, or carpal joint arthritis during the one-year follow-up (Figure 6). Furthermore, the patient was underwent a follow-up MRI about 18 mo postoperatively. The lunate edema was almost completely resorbed and the lunate bone had no features of progressing into osteonecrosis (Figure 7).
Lunate injury or peri-lunate injury may be easily missed at the initial presentation. According to the literature, approximately 25% of cases are associated with missed or delayed diagnosis. Lunate injury may result in progressive carpal instability, median neuropathy, avascular necrosis of the lunate, and end- to post-traumatic arthritis of the wrist joint[7]. The mechanism of injury is forced hyperextension, ulnar deviation, and intercarpal supination of the wrist[8].
Mayfield described the pattern of progressive peri-lunate instability in 1984[5]. In stage I, the distal carpal row is forced into hyperextension, and the scaphotra
Treatment of lunate or peri-lunate injury is currently challenging, given its rarity and high complication rate. The goals of surgical management are confirmation of reductions, ligamentous repair/reconstructions, fixation of associated fractures, and supplemental fixation of the bony architecture to facilitate ligamentous healing. The surgery can be performed through volar, dorsal, or combined approaches with carpal tunnel release. Herzberg suggested the single dorsal approach for cases in which the rotation of the dislocated lunate is less than 90°, and the double approach when the rotation of the bone is more than 90°[9]. However, several studies have demonstrated comparable outcomes. Thus, the choice of approach is largely influenced by surgeon preference[10-13].
This is the first such case in our practice to be treated with closed reduction and percutaneous Kirschner wires fixation. The reduction technique is meticulous and crucial. Although we agree that the closed reduction method can only be used in early-diagnosed cases of acute lunate dislocation, this surgical technique can provide an alternative treatment option that may be useful in selected cases.
This case provides evidence that the closed reduction technique for addressing acute lunate dislocation and managing triquetral fracture can reduce soft tissue destruction with the use of ligamentotaxis reduction. Postoperative 18 mo follow-up showed satisfactory outcome without progressive sequelae of carpal joint arthritis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Taiwan Society for Surgery of the Hand, No. 00818; Taiwan Orthopaedic Association, No. 001905.
Specialty type: Orthopedics
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liu H S-Editor: Ma YJ L-Editor: A P-Editor: Ma YJ
| 1. | Kastanis G, Velivasakis G, Pantouvaki A, Spyrantis M. An Unusual Localization of Lunate in a Transcaphoid Volar Lunate Dislocation: Current Concepts. Case Rep Orthop. 2019;2019:7207856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Najarian R, Nourbakhsh A, Capo J, Tan V. Perilunate injuries. Hand (N Y). 2011;6:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Aslani H, Bazavar MR, Sadighi A, Tabrizi A, Elmi A. Trans-Scaphoid Perilunate Fracture Dislocation; A Technical Note. Bull Emerg Trauma. 2016;4:110-112. [PubMed] |
| 4. | Scalcione LR, Gimber LH, Ho AM, Johnston SS, Sheppard JE, Taljanovic MS. Spectrum of carpal dislocations and fracture-dislocations: imaging and management. AJR Am J Roentgenol. 2014;203:541-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Mayfield JK. Patterns of injury to carpal ligaments. A spectrum. Clin Orthop Relat Res. 1984;36-42. [PubMed] |
| 6. | Reisler T, Therattil PJ, Lee ES. Perilunate dislocation. Eplasty. 2015;15:ic9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Herzberg G, Comtet JJ, Linscheid RL, Amadio PC, Cooney WP, Stalder J. Perilunate dislocations and fracture-dislocations: a multicenter study. J Hand Surg Am. 1993;18:768-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 285] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 8. | Mayfield JK. Wrist ligamentous anatomy and pathogenesis of carpal instability. Orthop Clin North Am. 1984;15:209-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Herzberg G, Forissier D. Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results. J Hand Surg Br. 2002;27:498-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Başar H, Başar B, Erol B, Tetik C. Isolated volar surgical approach for the treatment of perilunate and lunate dislocations. Indian J Orthop. 2014;48:301-305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Knoll VD, Allan C, Trumble TE. Trans-scaphoid perilunate fracture dislocations: results of screw fixation of the scaphoid and lunotriquetral repair with a dorsal approach. J Hand Surg Am. 2005;30:1145-1152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Kural C, Tanriverdi B, Erçin E, Baca E, Yilmaz M. The surgical outcomes of trans-scaphoid perilunate fracture-dislocations. Turk J Med Sci. 2020;50:25-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Trumble T, Verheyden J. Treatment of isolated perilunate and lunate dislocations with combined dorsal and volar approach and intraosseous cerclage wire. J Hand Surg Am. 2004;29:412-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 45] [Article Influence: 2.1] [Reference Citation Analysis (0)] |