Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.316
Peer-review started: August 11, 2021
First decision: October 20, 2021
Revised: October 23, 2021
Accepted: November 30, 2021
Article in press: November 30, 2021
Published online: January 7, 2022
Processing time: 140 Days and 18.4 Hours
Mature teratoma composed of all three basic germ cell layers of the head and neck is a rare disease. Teratomas involving the temporal bone are particularly scarce.
A 48-year-old male patient with a history of chronic otitis of the left ear from infancy, for which he had been operated on twice, was referred to our hospital for chronic otitis, cholesteatoma and a middle ear mass. Computed tomography (CT) scan and magnetic resonance imaging (MRI) revealed a eustachian tube teratoma, in which the anterior lower part and posterior upper part were connected by a thin membranaceous tissue. The mass was removed completely under general anesthesia by mastoidectomy. As of last follow-up (2 years post-surgery), the disease had not relapsed.
Pre-operative CT and MRI are necessary for eustachian tube teratoma. Complete surgical resection provided excellent prognosis.
Core Tip: Mature teratoma of the head and neck is a rare disease. We present a case of eustachian tube teratoma, in which the anterior lower part and posterior upper part were connected by a thin membranaceous tissue, in a 48-year-old male patient who had a history of chronic otitis of the left ear from infancy and had already been operated on twice. When a long history of chronic otitis is encountered, combined with polyps in the tympanum and/or external auditory canal, a combination of computed tomography and magnetic resonance imaging is necessary pre-operation.
- Citation: Li JY, Sun LX, Hu N, Song GS, Dou WQ, Gong RZ, Li CT. Eustachian tube teratoma: A case report. World J Clin Cases 2022; 10(1): 316-322
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/316.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.316
Teratomas of the head and neck account for 5%-15% of all teratomas and principally involve the nasopharynx and neck[1]. Reports of teratomas involving the temporal bone are scarce[2,3]. Herein, we present a case of mature teratoma of the eustachian tube (ET) in an adult male with a history of chronic otitis of the left ear from infancy.
A 48-year-old man was referred to our hospital for chronic otitis, cholesteatoma and a middle ear mass.
The patient had experienced chronic otitis of the left ear from infancy and underwent surgery for cholesteatoma in the tympanum at another hospital. However, his clinical symptoms had persisted. His conscious hearing was poor, and he suffered from earache, ear boredom, headache and dizziness.
The patient had no significant past medical history.
The patient’s family history was unremarkable.
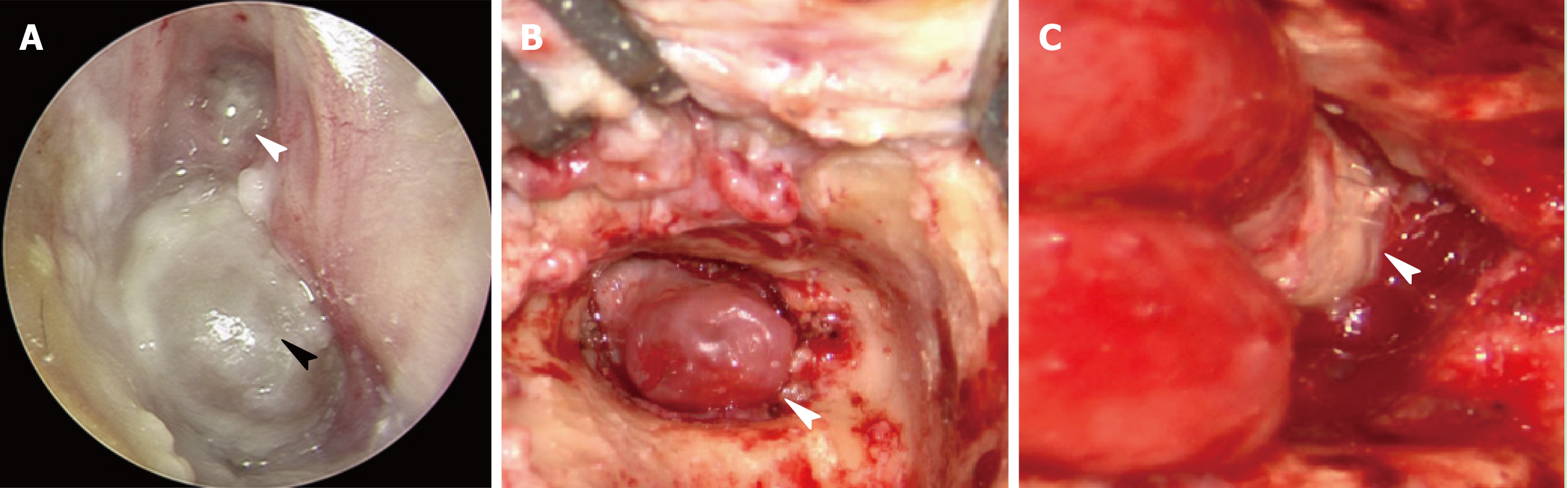
Otoscopic examination demonstrated a large amount of pus in the left external auditory canal, a fleshy polyp present at a deeper site, and mucosal edema in the previously operated area (Figure 1). Audiometric assessment confirmed a severe conductive hearing loss; hearing threshold was 80 dB and auditory brainstem response was 70 dB on the affected side. Nasopharyngoscopy showed that the orifice of the left ET opened well.
The laboratory examination was otherwise unremarkable. The laboratory assessment included routine blood tests. Tests for C-reactive proteins and viral hepatitis markers were negative. Glucose and serum insulin levels were normal.
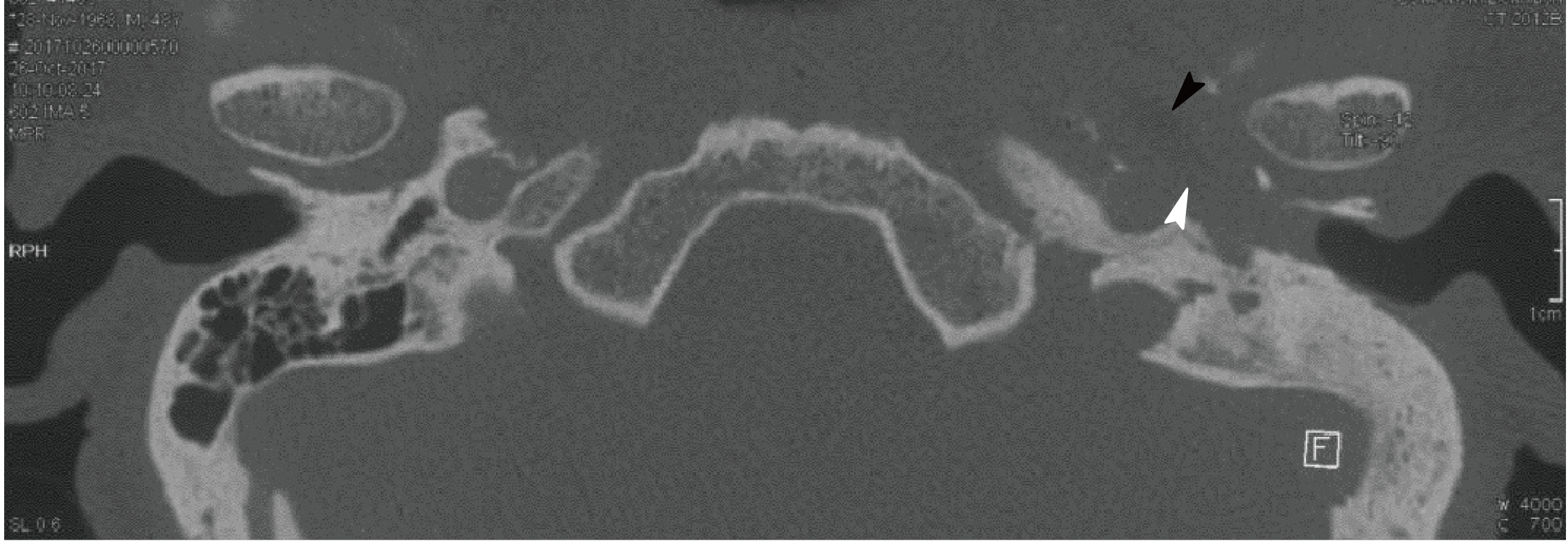
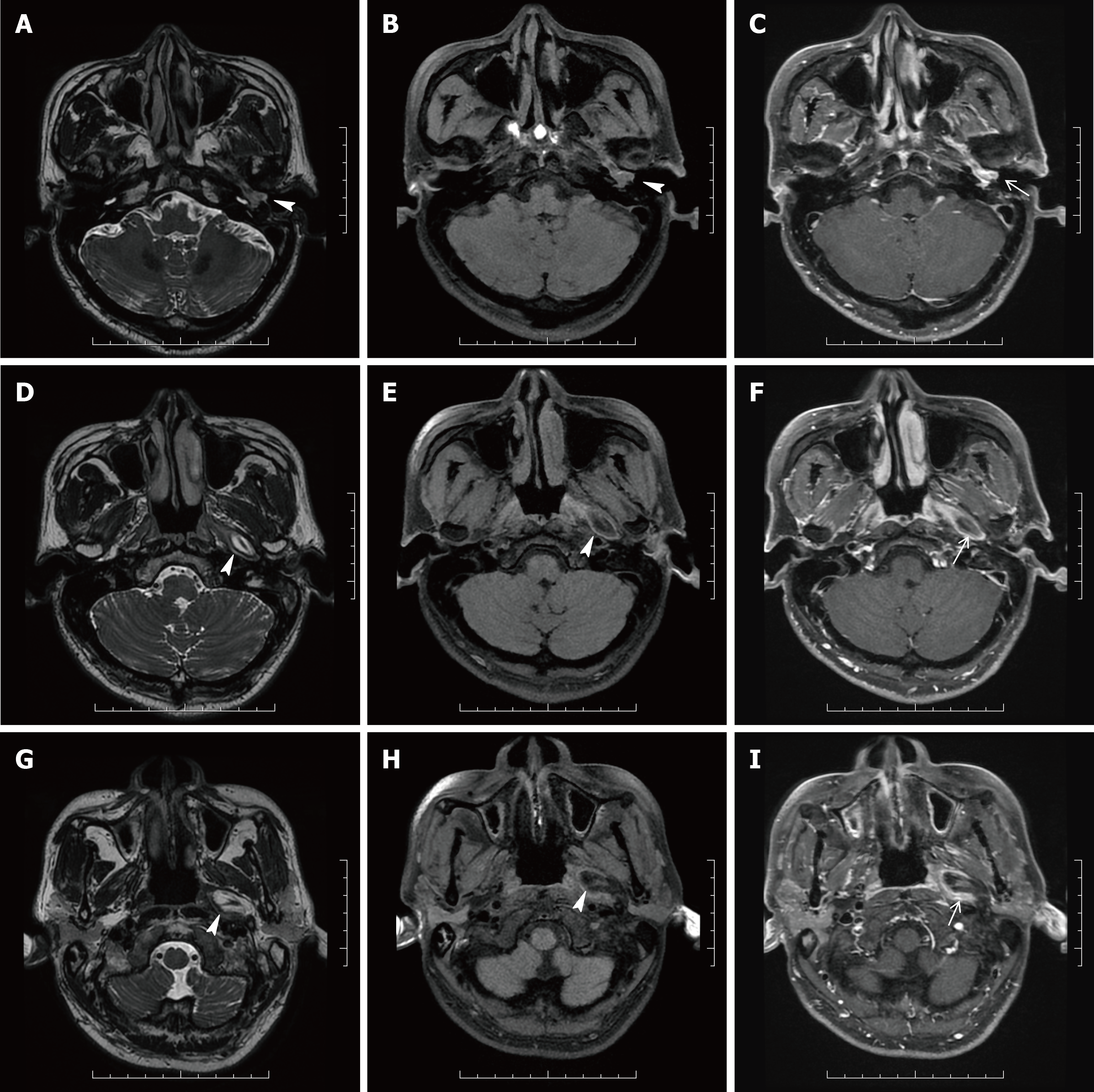
The unenhanced computed tomography (CT) of the temporal bone showed some changes, including a well-circumscribed, mixed density tumor with a fat density area in the ET; the lesion extended down to the left part of the tympanum and external auditory canal (Figure 2), without ossicular chain, which had resulted from the mastoidectomy. The T1- and T2-weighted magnetic resonance imaging (MRI) in the transverse plane showed a 3.2 cm × 1.3 cm × 2.0 cm, well-defined, homogeneous lesion with high signal intensity along the left ET. The mass showed signal intensity similar to that of the fat on all sequences and with little cartilage signal (Figure 3). The lesion extended down to the left part of the tympanum and external auditory canal, where the signal was slightly higher than the part in the ET. On fat-saturated T1- and T2-weighted sequences, the part of the mass in the ET demonstrated a decreased signal intensity, indicating that the mass was consistent with macroscopic fat. The mass was surrounded by a smooth, thick, hypointense capsule, which was enhanced slightly after contrast administration.
The ET diameter was expanded, to about 0.8 cm. The part of the mass in the tympanum and external auditory canal was classified as a fleshy polyp. However, “hairs” were visible on the surface of the mass and cartilage surrounded by the mass could be seen in the ET area (Figure 1). The mass, in which the anterior lower part and posterior upper part were connected by a thin membranaceous tissue, was in the ET. It was tightly bonded to the former ET wall and could not be removed in toto, so serial partial excision was performed. The resulting cavity (composed of the tympanum and external auditory canal) was then resolved by filling with abdominal fat.
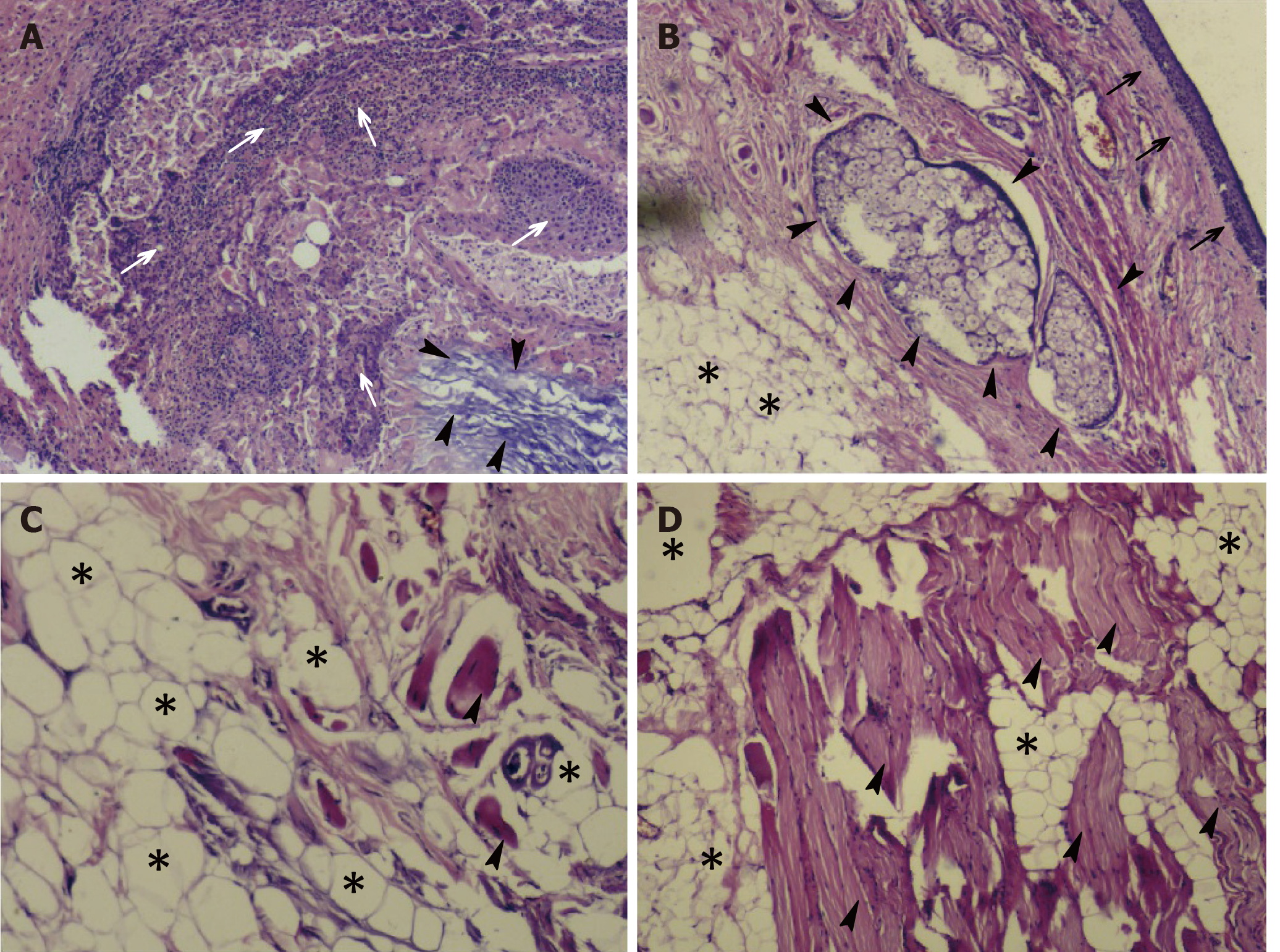
On gross examination, the resected mass appeared as a cluster of irregular, soft, grey-colored tissue. Microscopically, a photomicrograph of the mass revealed characteristics of keratinized squamous epithelium, adipose, sweat gland and mature skeletal muscle tissues. Photomicrographs of the areas including the tympanum and external auditory canal revealed squamous epithelial mucosal polyps (Figure 4).
Mature teratomas.
The mass was removed completely by mastoidectomy, with the patient under general anesthesia.
After follow-ups at 7 mo and 2 years, the patient showed no signs of disease relapse.
Mature teratoma is a true neoplasm composed of all three basic germ cell layers (ectoderm, mesoderm, and endoderm), which differs from dermoids and epidermois[4]. Most cases involve a midline or paraxial location, and the most common site is in the sacrococcygeal region (40%-60% of cases)[5]. Only 2%-10% of cases have involved the head and neck regions[5], especially the cervical and nasopharyngeal regions. We used the PubMed database to search for relevant publications on (keywords) “mature teratoma” and “eustachian tube”. We found only eight relevant publications among the English-language literature, excluding reports on dermoid cysts, which represent a special category of teratomas. According to the histologic classification of teratomas in the head and neck region that is most commonly used today, the term ‘dermoid’ (as it was proposed by Arnold in 1888) is most appropriate[6]. This implies an origin from epidermal and mesodermal elements, which differentiates them histologically from teratomas composed of elements from all three germinal layers and from cholesteatomas, which are only of ectodermal origin[7]. Of these 9 total cases reported to date (including this case), 4 were male and 5 female; the near 1:1 ratio indicates that there is no sex preponderance for ET teratoma. The age of the 9 patients ranged from 1 d to 48 years, with a median of 10-mo-old. The cases had various clinical manifestations, as follow: foul-smelling left otorrhea[8], peripheral palsy of the seventh cranial nerve[5], a tongue-like structure which protruded when the patient cried and retracted into the mouth when swallowing[9], a history of refractory otitis media and a nasopharyngeal mass[3], a discharging left ear since infancy[10], respiratory distress in a premature infant[11] with recurrent otitis media and chronic otorrhea of the left ear[12], and a history of chronic otitis of the right ear from infancy[13]. However, all these manifestations were due to obstruction of the channel or oppression of the surrounding structures.
The case presented here is the first reported for an ET teratoma with the anterior lower part and posterior upper part connected by a thin membranaceous tissue, accompanied by a fleshy polyp in the tympanum and external auditory canal. The patient, who had a history of chronic otitis of the left ear from infancy, was older than the other 8 patients reported for previous cases. It is, therefore, possible that the history of chronic otitis of the left ear and previous operations he underwent led to the formation of a fleshy polyp in the tympanum and external auditory canal. Of note, in patients with a history of chronic otitis that exhibit polyps in the tympanum and/or external auditory canal, it is important to avoid the assumption that these are merely a result of inflammation. Equally important is to avoid making an immediate call for surgery. Both CT and MRI examinations must be performed to appraise the condition of the ET and identify possible neoplasms. For our patient, the only examination made before his previous surgery was a CT scan. This led to the failure of identifying the ET tumor. Had a preoperative MRI examination been conducted, the ET tumor would likely have been detected and the following operation would have addressed both the inflammation and the tumor.
Ultrasound is an ideal initial imaging modality to investigate neck masses, as it reveals the solid or cystic nature in most cases and localizes the lesion in relation to surrounding structures[14], but it has some limitations when applied to the temporal bone region. A combination of CT and MRI scans provides valuable clinical information to exclude alternative cranial base pathologies and assess the extent of the lesion. The CT scan allows for better evaluation of the bone architecture, whereas the MRI scan can better demonstrate the relationship between the mass and the carotid artery beneath the temporal bone[7]. The typical clinical presentation of ET teratomas includes recurrent episodes of otitis media and chronic otorrhea[15,16], caused by the obstruction of the ET by the teratomas. Ultimately, ET teratoma requires surgical removal and has excellent prognosis upon complete resection[12].
In summary, this case highlights the necessity of examination via a combination of CT and MRI pre-operation for ET teratoma. The surgical removal itself provides an excellent prognosis upon complete resection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Corvino A S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
| 1. | Aubin A, Pondaven S, Bakhos D, Lardy H, Robier A, Lescanne E. Oropharyngeal teratomas in newborns: management and outcome. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131:271-275. [PubMed] [DOI] [Full Text] |
| 2. | Nalavenkata S, Meller C, Forer M, Patel NP. Dermoid cysts of the Eustachian tube: a transnasal excision. Int J Pediatr Otorhinolaryngol. 2013;77:588-593. [PubMed] [DOI] [Full Text] |
| 3. | Nicklaus PJ, Forte V, Thorner PS. Hairy polyp of the eustachian tube. J Otolaryngol. 1991;20:254-257. [PubMed] |
| 4. | Smirniotopoulos JG, Chiechi MV. Teratomas, dermoids, and epidermoids of the head and neck. Radiographics. 1995;15:1437-1455. [PubMed] [DOI] [Full Text] |
| 5. | Navarro Cunchillos M, Bonachera MD, Navarro Cunchillos M, Cassinello E, Ramos Lizana J, Oña Esteban J. Middle ear teratoma in a newborn. J Laryngol Otol. 1996;110:875-877. [PubMed] [DOI] [Full Text] |
| 6. | Tharrington CL, Bossen EH. Nasopharyngeal teratomas. Arch Pathol Lab Med. 1992;116:165-167. [PubMed] |
| 7. | Kollias SS, Ball WS Jr, Prenger EC, Myers CM 3rd. Dermoids of the eustachian tube: CT and MR findings with histologic correlation. AJNR Am J Neuroradiol. 1995;16:663-668. [PubMed] |
| 8. | Forrest AW, Carr SJ, Beckenham EJ. A middle ear teratoma causing acute airway obstruction. Int J Pediatr Otorhinolaryngol. 1993;25:183-189. [PubMed] [DOI] [Full Text] |
| 9. | Wasinwong Y, Chaipasithikul S, Kanchanapitak P. Eustachian tube mature teratoma. Otolaryngol Head Neck Surg. 2003;128:589-591. [PubMed] [DOI] [Full Text] |
| 10. | Bowyer DJ, Wilson J, Sillars HA. Mature teratoma of the eustachian tube. Otol Neurotol. 2012;33:e43-e44. [PubMed] [DOI] [Full Text] |
| 11. | Bayır Ö, Güneri EA, Dilek M, Özer E, Çakmakçı H, Erdağ TK. Nasopharyngeal mature teratoma in the newborn. Turk Pediatri Ars. 2014;49:257-260. [PubMed] [DOI] [Full Text] |
| 12. | Rondenet C, Boudjemaa S, Sileo C, Garabedian EN, Ducou le Pointe H, Blondiaux E. CT and MR imaging findings of teratoma of the Eustachian tube. Diagn Interv Imaging. 2017;98:269-271. [PubMed] [DOI] [Full Text] |
| 13. | Cruz-Toro P, Moya R, Domènech I. Eustachian tube teratoma. Acta Otorrinolaringol Esp. 2015;66:e22-e23. [PubMed] [DOI] [Full Text] |
| 14. | Corvino A, Pignata S, Campanino MR, Corvino F, Giurazza F, Tafuri D, Pinto F, Catalano O. Thyroglossal duct cysts and site-specific differential diagnoses: imaging findings with emphasis on ultrasound assessment. J Ultrasound. 2020;23:139-149. [PubMed] [DOI] [Full Text] |
| 15. | Batsakis JG. Tumors of the Head and Neck. 2nd ed. Baltimore: Williams & Wilkins, 1979: 226-228. [DOI] [Full Text] |
| 16. | Fried MP, Vernick DM. Dermoid cyst of the middle ear and mastoid. Otolaryngol Head Neck Surg. 1984;92:594-596. [PubMed] [DOI] [Full Text] |