Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.283
Peer-review started: April 11, 2021
First decision: October 16, 2021
Revised: November 16, 2021
Accepted: November 29, 2021
Article in press: November 29, 2021
Published online: January 7, 2022
Processing time: 262 Days and 21.7 Hours
Ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare, and there is no reference for fracture classification and treatment options.
We report a 27-year-old male patient who sustained ipsilateral femoral neck and intertrochanteric fractures and was treated with a proximal femoral locking compression plate (PFLCP). The literature on these fractures was also reviewed. At the last follow-up three years after surgery, the patient had no obvious pain in the hip, and the range of motion in the hip joint was slightly limited, but met the normal life and work needs. There were no complications such as necrosis of the femoral head.
The PFLCP can be used to treat these complex proximal femoral fractures, and selection should be based on the patient's specific fractures.
Core Tip: Ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare. We report a 27-year-old patient who sustained ipsilateral femoral neck and intertrochanteric fractures and was treated with a proximal femoral locking compression plate. At the last follow-up three years after surgery, satisfactory outcomes were achieved. There were no complications such as necrosis of the femoral head.
- Citation: Li ZY, Cheng WD, Qi L, Yu SS, Jing JH. Complex proximal femoral fracture in a young patient followed up for 3 years: A case report. World J Clin Cases 2022; 10(1): 283-288
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/283.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.283
Proximal femoral fractures (PFFs) are one of the most common orthopedic injuries, which mainly occur in the elderly and are uncommon in young people[1,2]. PFFs mainly refer to femoral head fracture, femoral neck fracture, and intertrochanteric fracture, while ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare. PFFs in young patients are mostly caused by high-energy trauma[3,4]. The fracture mechanism, bone quality, and treatment requirements of young patients are different from those of elderly patients. Although there are a large number of reports of PFFs in elderly patients, there is no reference for the treatment of young patients, especially those with ipsilateral femoral neck and intertrochanteric fractures. Therefore, we report the case of a 27-year-old patient who sustained a complex proximal femoral fracture that involved ipsilateral femoral neck and intertrochanteric fractures. The literature on ipsilateral femoral neck and intertrochanteric fractures was also reviewed.
A 27-year-old male patient was admitted to the Department of Orthopedics of our hospital with left hip pain and limited mobility 5 h after a car accident.
The patient was involved in a car accident 5 h previously and underwent clinical and radiological examinations due to left hip pain and limited mobility.
The patient had no previous medical history.
There was no previous medical history.
The patient’s left lower limb showed external rotation malformation, which was shorter than that of the healthy side. The patient's peripheral sensation and blood flow were normal, and there were no clinical manifestations of vascular and nerve damage.
No abnormalities were detected on preoperative examinations.
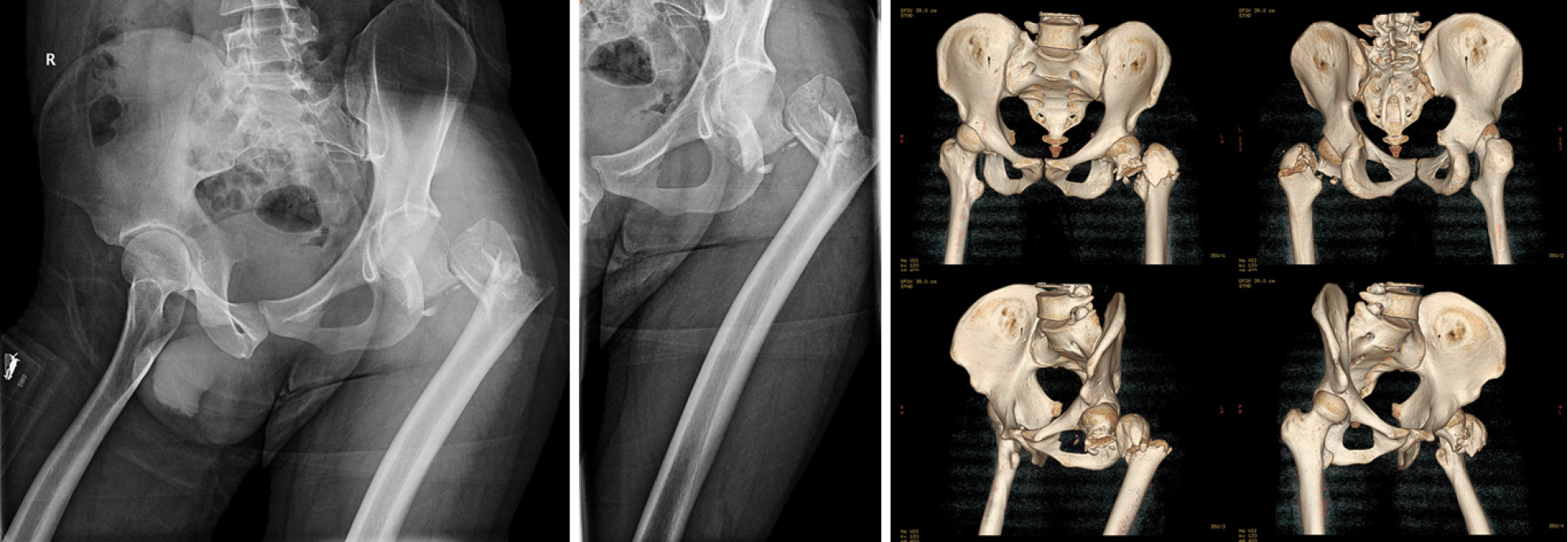
Radiological examinations including X-rays and three-dimensional computed tomography of bilateral hips showed that the femoral neck base fracture was accompanied by a greater trochanteric comminuted fracture, and the displacements were obvious (Figure 1).
Due to the lack of suitable fracture classification criteria, we defined the patient's fractures as complex proximal femoral fractures.
After confirming the patient's fractures, we immediately performed skeletal traction of the left lower extremity tibial tubercle and provided symptomatic treatment such as analgesia and elimination of swelling before surgery.
A collective discussion on the patient's condition and surgical plan was held which mainly consisted of selection of the internal fixation method. Considering the complicated fractures and obvious displacements, we planned to perform open reduction and internal fixation. The fixation methods for proximal femoral fractures mainly included intramedullary fixation such as proximal femoral nail anti-rotation (PFNA) and extramedullary fixation such as a proximal femoral locking compression plate (PFLCP). In order to ensure the success of the operation, we prepared both intramedullary and extramedullary fixation systems before surgery[5-9].
Following skin and soft tissue incision, the femoral neck base fracture and the greater trochanteric comminuted fracture were found under direct vision. We first used towel forceps and Kirschner wires to sequentially reduce and fix the proximal fractures, including the comminuted intertrochanteric fracture and femoral neck fracture. Then the distal and proximal femoral fractures were reduced by lower limb traction and temporarily fixed with Kirschner wires. The C-arm X-ray machine showed that the fracture reduction and cervico-diaphyseal angle of the femur were satisfactory. Considering that the greater trochanteric comminuted fracture was difficult to maintain by intramedullary fixation such as PFNA, the PFLCP was used. In addition, wire binding was used to strengthen fixation of the intertrochanteric comminuted fracture. Finally, the C-arm X-ray machine was used to further ensure anatomical reduction of the femoral neck and intertrochanteric fractures.
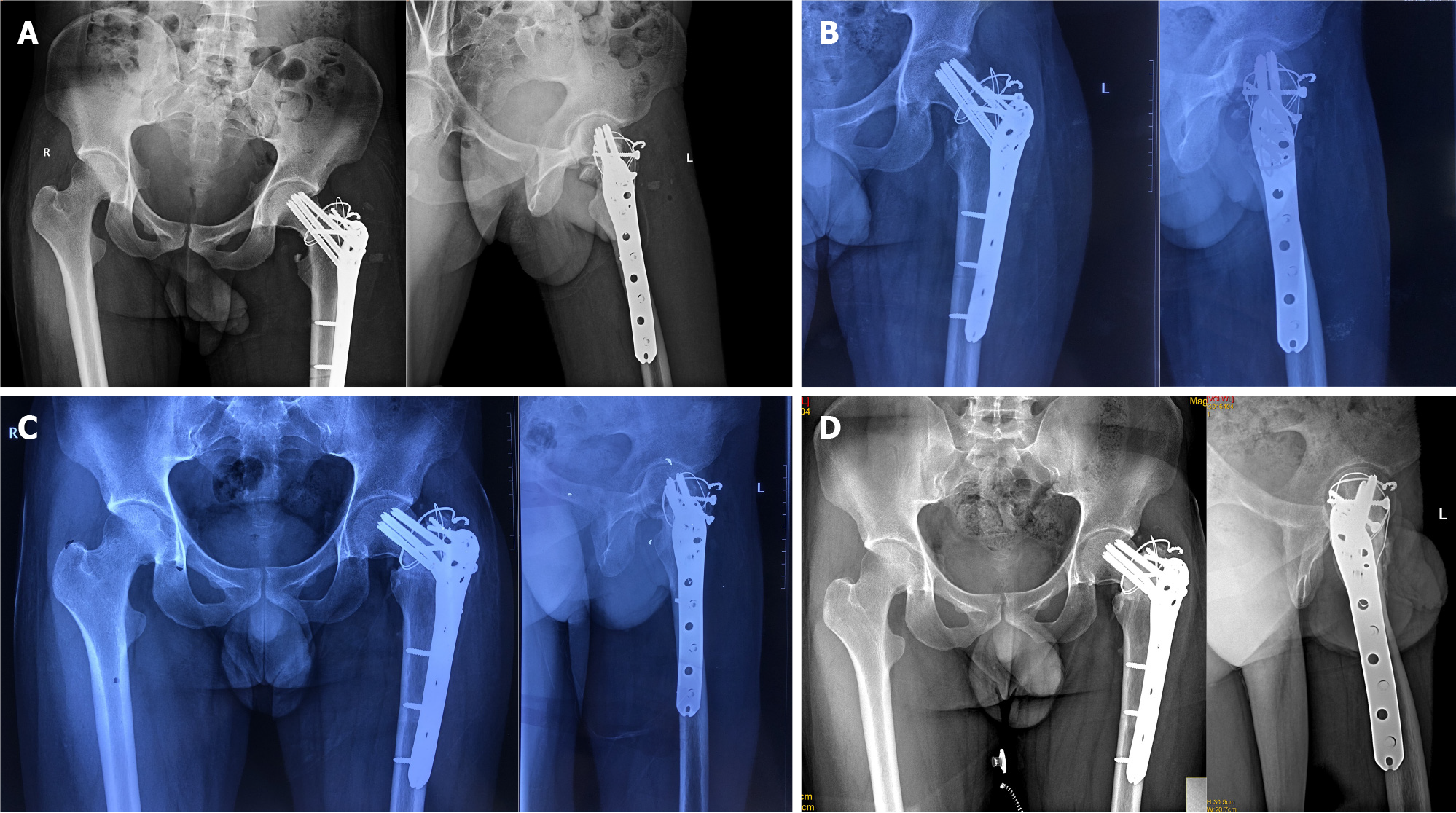
The patient received symptomatic treatment such as anti-infection and elimination of swelling after surgery. Postoperative X-rays showed that the fractures were well reduced, the cervico-diaphyseal angle of the femur was satisfactory, and the internal fixation position was normal (Figure 2A). The patient was discharged 1 wk after surgery and was instructed to rest in bed, raise the affected limb, strengthen lower limb muscle function by exercising and avoid weight-bearing. He was followed regularly, including physical and radiological examinations.
At 1 mo postoperatively, X-rays showed that a small amount of callus had formed around the greater trochanter, and the internal fixation position was normal. The Harris Hip Score (HHS) was 39. The patient was instructed to perform lower limb functional exercise without weight-bearing in bed.
At 3 mo postoperatively, X-rays showed that the fracture lines were blurred (Figure 2B). The HHS was 62. The patient was permitted to walk with partial weight-bearing using a walker, and gradually increase weight-bearing.
At 12 mo postoperatively, X-rays showed that the fractured end of the femoral neck had collapsed, the cervico-diaphyseal angle had reduced, and the fracture lines were blurred (Figure 2C). The fractures had healed completely, and complications such as hip varus deformity and slight limitation in the range of motion of the hip joint were observed. However, there were no complications such as necrosis of the femoral head and hip pain. The HHS was 91. The patient did not engage in exercise-related work, and his hip function after surgery met his life and work needs.
At 24 mo (Figure 2D) and 36 mo postoperatively, X-rays were similar to those at 12 mo postoperatively, and the hip varus deformity did not significantly worsen. The HHS was 93. No complications such as necrosis of the femoral head and hip pain were observed.
Fractures such as PFFs mainly occur in the elderly, mostly due to low-energy injury. However, high-energy injuries, such as car accidents and fall injuries, have led to an increasing number of PFFs in young patients[1,3]. PFFs mainly include femoral head fracture, femoral neck fracture, and intertrochanteric fracture. Cannulated screw internal fixation is most commonly used for femoral neck fracture in young patients[10]. Non-weight bearing is required for at least 8 wk after surgery, and weight bearing is resumed gradually when the radiological examination shows fracture healing progress[10-13]. The most common complications include nonunion, varus collapse, limb shortening, and osteonecrosis[10-13]. PFNA internal fixation is most frequently used for intertrochanteric fracture in young patients, and the patients are advised to get out of bed as soon as possible for gradual weight bearing training[8,9]. The most common complications include limb shortening and coxa vara[8,9]. Anatomical reduction, effective internal fixation, and rehabilitation exercises are the main strategies to avoid complications. The ipsilateral femoral neck and intertrochanteric fractures in young patients are extremely rare, and there is no good reference for the classification and internal fixation of this complex proximal femoral fracture.
The goal of treatment in young patients with PFFs is to preserve the femoral head and prevent osteonecrosis and pseudoarthrosis to avoid total hip replacement[14]. The early treatment and correct choice of implant to achieve anatomical reduction and effective internal fixation are essential. The fixation methods for intertrochanteric fracture in young patients mainly include PFNA and PFLCP[5-9].
In 2016, Giancola et al[14] reported a 39-year-old patient with a complex proximal femoral fracture that involved the neck and trochanteric region. The multifragmentary comminution of the femoral neck associated with rupture of the greater trochanteric region, without involving the lesser trochanter was treated with skeletal traction in the first stage and then implantation of an intramedullary nail. Twenty months after surgery, the fractures were healed and the patient was able to walk and run without pain. Giancola et al[14] suggested that early surgery and suitable internal fixation options were essential in the treatment of the patient and the transverse component of the proximal femur fracture determined the choice of intramedullary nail.
In 2018, Su et al[15] reported two cases of ipsilateral femoral neck and inter
In this study, we report a 27-year-old male patient who was involved in a car accident. The radiological examinations showed that the femoral neck base fracture was accompanied by a greater trochanteric comminuted fracture, and the displacements were obvious. After confirming the patient's fractures, skeletal traction of the left lower extremity tibial tubercle was performed and he received symptomatic treatment such as analgesia and elimination of swelling before surgery. Considering that the greater trochanteric comminuted fracture was difficult to maintain by PFNA, a PFLCP was used[2,16,17]. In addition, a PFLCP can be used as a stress barrier in the lateral wall of the trochanter to prevent lateral movement of the proximal femoral fracture fragments, and has a strong antagonistic effect on the rotation and bending of the femoral neck. The multiple locking screw holes of the PFLCP provide a variety of options to overcome any complex fracture pattern and can minimize pressure on the periosteum, thereby promoting rapid biological healing[3,9,18].
Postoperative X-rays showed that the fractures were well reduced, the cervico-diaphyseal angle was satisfactory, and the internal fixation position was normal. At the last follow-up three years after surgery, the patient had no obvious pain in the hip, and the range of motion of the hip joint was slightly limited, but it met the normal life and work needs of the patient. The HHS was 91. X-ray examinations showed that the fractured end of the femoral neck had collapsed, the cervico-diaphyseal angle had reduced, and a hip varus deformity was observed. However, there were no complications such as necrosis of the femoral head. The patient was satisfied with the prognosis of the fractures.
Ipsilateral femoral neck fractures and intertrochanteric fractures in young patients are extremely rare and lack appropriate fracture classification criteria and treatment guidelines. Therefore, this type of case report is of great significance. Early diagnosis and treatment, as well as appropriate internal fixator selection, are essential for the treatment of such complex fractures. As an important treatment before surgery, skeletal traction should be performed as soon as possible. A PFLCP can be used to treat this complex proximal femoral fracture, and selection should be based on the patient's specific fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Purudappa PP S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, Cosman F. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int. 2010;21:399-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 202] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 2. | Robinson CM, Court-Brown CM, McQueen MM, Christie J. Hip fractures in adults younger than 50 years of age. Epidemiology and results. Clin Orthop Relat Res. 1995;238-246. [PubMed] |
| 3. | Ibrahim S, Meleppuram JJ. A retrospective analysis of surgically-treated complex proximal femur fractures with proximal femoral locking compression plate. Rev Bras Ortop. 2017;52:644-650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Askin SR, Bryan RS. Femoral neck fractures in young adults. Clin Orthop Relat Res. 1976;259-264. [PubMed] |
| 5. | Li AB, Zhang WJ, Wang J, Guo WJ, Wang XH, Zhao YM. Intramedullary and extramedullary fixations for the treatment of unstable femoral intertrochanteric fractures: a meta-analysis of prospective randomized controlled trials. Int Orthop. 2017;41:403-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Griffin XL, Costa ML, Phelps E, Parsons N, Dritsaki M, Png ME, Achten J, Tutton E, Lerner R, McGibbon A, Baird J. Retrograde intramedullary nail fixation compared with fixed-angle plate fixation for fracture of the distal femur: the TrAFFix feasibility RCT. Health Technol Assess. 2019;23:1-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Tazawa R, Minehara H, Matsuura T, Kawamura T, Sakai R, Yoshida K, Inoue G, Takaso M. Biomechanical evaluation of internal fixation for the treatment of comminuted subtrochanteric femur fractures. J Orthop Sci. 2021;26:261-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Andalib A, Etemadifar M, Yavari P. Clinical Outcomes of Intramedullary and Extramedullary Fixation in Unstable Intertrochanteric Fractures: A Randomized Clinical Trial. Arch Bone Jt Surg. 2020;8:190-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Zang W, Liu PF, Han XF. A comparative study of proximal femoral locking compress plate, proximal femoral nail antirotation and dynamic hip screw in intertrochanteric fractures. Eur Rev Med Pharmacol Sci. 2018;22:119-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Sun H, Shu LY, Sherrier MC, Zhu Y, Liu JW, Zhang W. Decreased complications but a distinctive fixation loosening mechanism of fully threaded headless cannulated screw fixation for femoral neck fractures in young adults. J Orthop Surg Res. 2021;16:234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Duffin M, Pilson HT. Technologies for Young Femoral Neck Fracture Fixation. J Orthop Trauma. 2019;33 Suppl 1:S20-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Yang Q, Chen N, Fu W. External fixation via the anterior inferior iliac spine for proximal femoral fractures in young patients. Open Med (Wars). 2021;16:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Fan Z, Huang Y, Su H, Jiang T. How to choose the suitable FNS specification in young patients with femoral neck fracture: A finite element analysis. Injury. 2021;52:2116-2125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 14. | Giancola R, Marchesi LP, Lettera MG, Antonini G. A complex proximal femoral fracture. Injury. 2016;47 Suppl 4:S121-S123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 15. | Su C, Liu Y, Wu P, Yuan J, Lang J, Wu C, Zhang Y, Chen L. Ipsilateral femoral neck and intertrochanteric fractures with posterior dislocation of the hip: A report of two cases. J Orthop Surg (Hong Kong). 2020;28:2309499019900449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;82-86. [PubMed] |
| 17. | Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P; Hip Fracture Study Group. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007;89:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 18. | Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 497] [Article Influence: 23.7] [Reference Citation Analysis (0)] |