Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.268
Peer-review started: March 9, 2021
First decision: April 4, 2021
Revised: April 18, 2021
Accepted: November 26, 2021
Article in press: November 26, 2021
Published online: January 7, 2022
Processing time: 295 Days and 21.1 Hours
Well-differentiated liposarcoma is the second most common pathologic type of retroperitoneal sarcoma. It is characterized by a huge mass, but multiple organ invasions are common. Surgery is the only treatment option for potential cure. Hyper-accuracy three-dimensional (3D) reconstruction is widely used in robotic partly nephrectomy owing to its ability to visualize overlapping anatomy.
A 54-year-old man was admitted for progressive abdominal distension over the preceding 2 mo. Computed tomography revealed a 32 cm × 21 cm × 12 cm lipomatous mass. Hyper-accuracy 3D reconstruction was performed because of the complex relationship between the mass and nearby tissue. The patient underwent surgical resection, and the tumor did not recur for over 16 mo.
Hyper-accuracy 3D reconstruction is useful for operative planning owing to its intuitiveness and precise determination of anatomical structures in both tumors and nearby tissues.
Core Tip: Surgical resection is the preferred treatment for well-differentiated liposarcoma (WDLPS). Hyper-accuracy three-dimensional (3D) reconstruction is widely used in robotic partial nephrectomy for its ability to visualize overlapping anatomy. Here, we report a case of giant WDLPS in the retroperitoneum treated by surgical resection using hyper-accuracy 3D reconstruction. To the best of our knowledge, our case was the first to use this technique for giant retroperitoneal WDLPS. We expect our case to highlight the value of hyper-accuracy 3D reconstruction for complicated open surgery and provide a basis for retroperitoneal liposarcoma treatment.
- Citation: Ye MS, Wu HK, Qin XZ, Luo F, Li Z. Hyper-accuracy three-dimensional reconstruction as a tool for better planning of retroperitoneal liposarcoma resection: A case report. World J Clin Cases 2022; 10(1): 268-274
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/268.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.268
Retroperitoneal pathologic processes might be asymptomatic and often present as large masses at initial imaging evaluation[1]. Retroperitoneal sarcomas accounts for 9% to 15% of all adult soft-tissue sarcomas[2], including liposarcoma, leiomyosarcoma, and malignant fibrous histiocytoma/undifferentiated pleomorphic sarcoma[3]. Retroperitoneal liposarcoma is the second most common, accounting for 45%[4]. Hyper-accuracy three-dimensional (3D) reconstruction is based on contrast-enhanced computed tomography (CT), including arterial and delayed phases. It provides surgeons with three key anatomic aspects, including 3D surface-rendered and semitransparent organs and tumors, and the 3D course of extra- and intrarenal arteries[5]. It is now widely used in robotic partly nephrectomy owing to its ability to visualize overlapping anatomy[6,7].
A 54-year-old man was admitted to our department for progressive abdominal distension over the preceding 2 mo.
The patient started to feel abdominal distension and noted his abdomen’s volume increasing 2 mo before presentation. He denied diarrhea, vomiting, abdominal pain, or constipation. He also denied any changes in bowel habits. He lost approximately 5 kg in the previous 2 mo.
The patient was previously healthy.
The patient had smoked for approximately 30 years, and his family history was unremarkable.
The patient was afebrile with stable vital signs. He was 163 cm in height and 56 kg in weight. Abdominal physical examination revealed a fixed abdominal mass with ill-defined margins occupying the entire abdomen. No other abnormal signs were found.
Laboratory tests showed a normal white count and hemoglobin level of 103.0 g/L (reference range, 120-160 g/L for man). His 8 AM cortisol level was 2.06 μg/dL (reference range, 8.7-22.4 μg /dL) and adrenocorticotrophic hormone level was 6.14 pg/mL (reference range, 0-46 pg/mL). The albumin level decreased slightly (30.9 g/L; reference range, 35.0-54.0 g/L), with no other liver function and kidney function abnormalities.
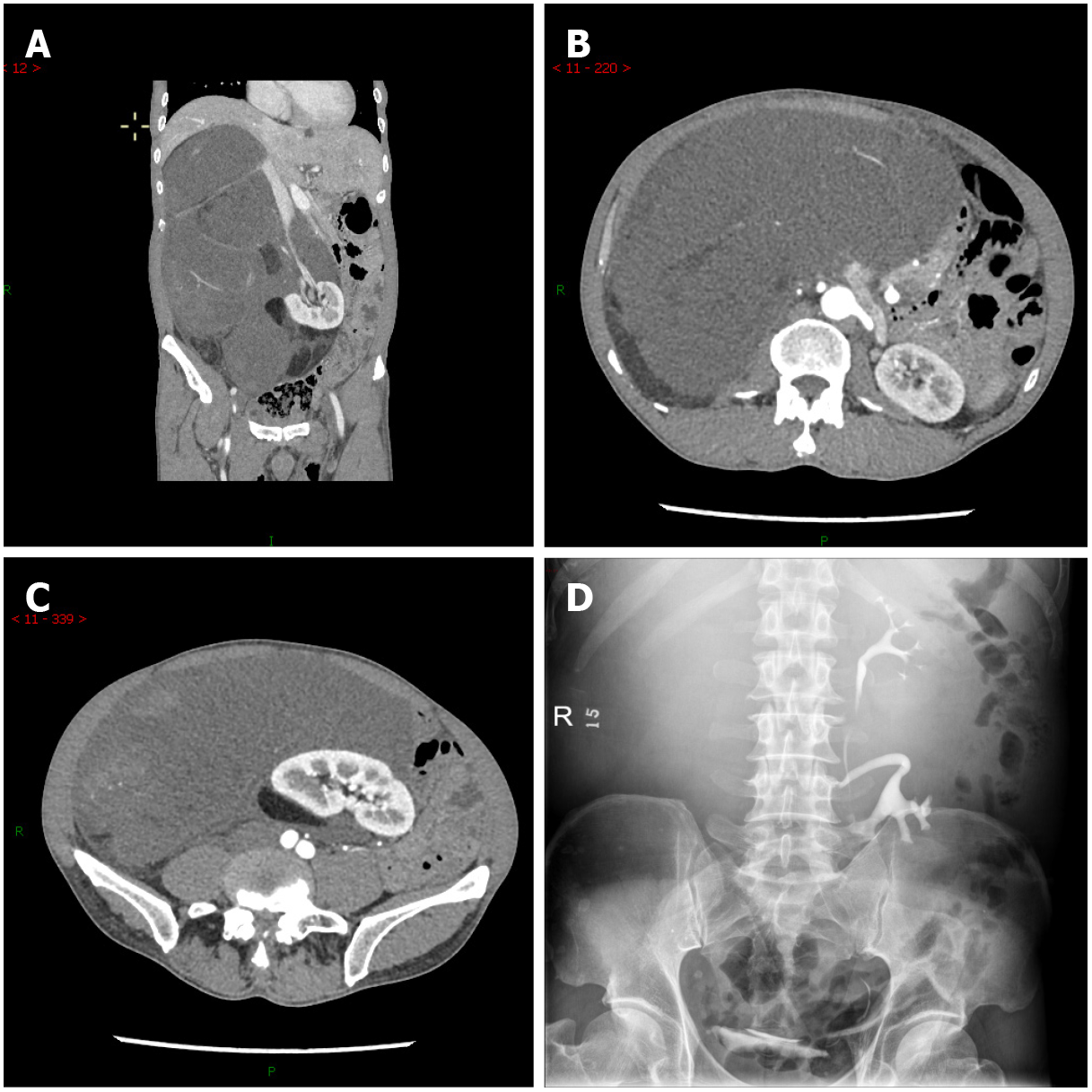
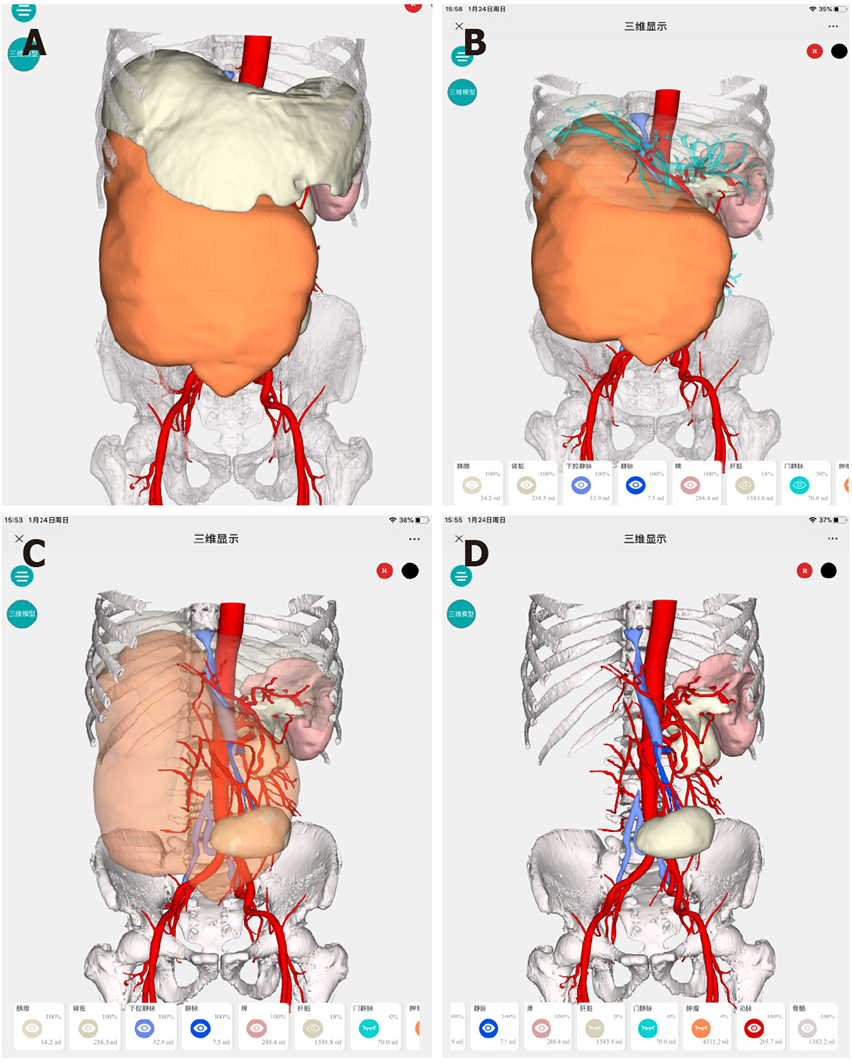
Abdominal CT angiography revealed a 32 cm × 21 cm × 12 cm lipoma-like mass extending from the sub-hepatic space to the pelvic cavity. There were no enlarged lymph nodes. Radiocontrast agent confirmed the displacement of the right kidney to the left lower quadrant (Figure 1). Because of the complex relationship between the mass and nearby tissue, we performed a hyper-accuracy three-dimensional reconstruction (Figure 2). This study revealed that the mass received blood vessels from a branch of the right renal artery. The celiac trunk, the superior mesenteric, the inferior vena cava, and the pancreas were displaced and compressed.
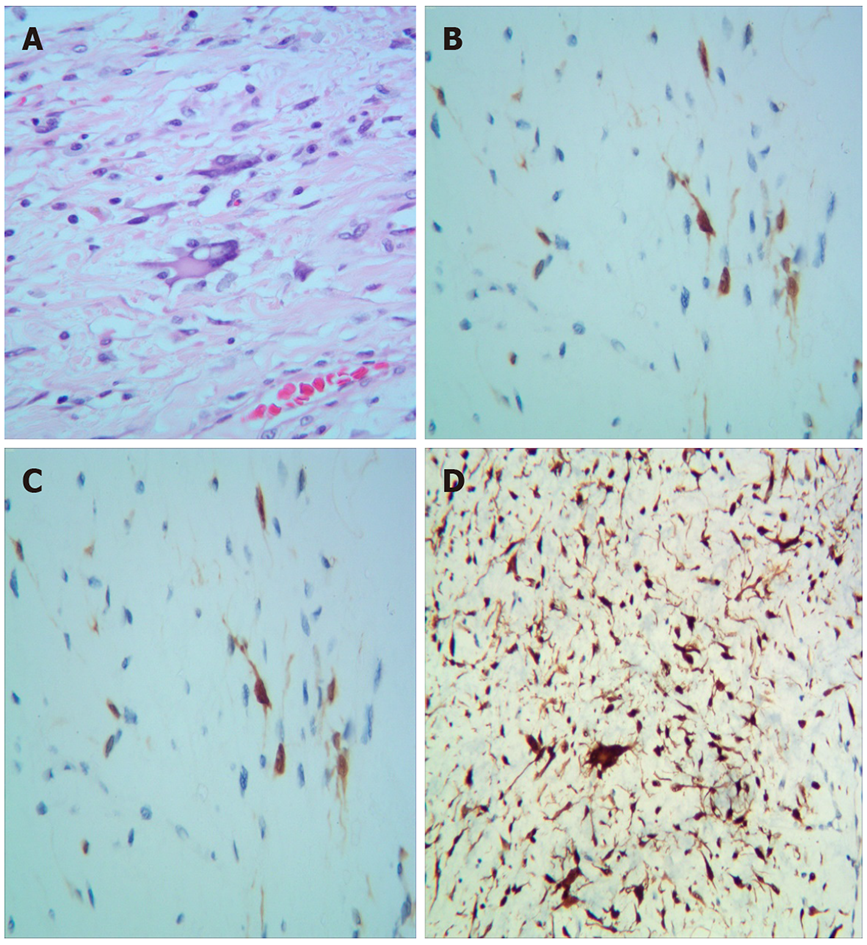
Pathological examination revealed well-differentiated liposarcoma (WDLPS). Macroscopically, the mass appeared oval but was separated into irregular lobulations. Its size was 37 cm × 26 cm × 10 cm and it weighed approximately 11 kg. The surface of the mass was covered with a smooth and grayish capsule. The mass wrapped the adrenal gland. Microscopically, the tumor was composed of well-differentiated adipocytes and spindle-shaped cells. Areas of necrosis were rare. Nuclear degeneration was found in some areas (1/10 high-powered fields). Immunohistochemically, the tumor was partly positive for MDM2, S100, CK34, and CKD4, with a low grade of dedifferentiation (Ki-67: 20%) (Figure 3).
WDLPS.
Explorative laparotomy was performed. We chose a median abdominal incision from the xiphoid process to the pubic symphysis. No signs of infiltration or metastasis were found in the abdominal cavity. Because we ensured that the tumor was localized in the retroperitoneum, we opened the retroperitoneum in the paracolic recess. After liberating the ascending colon and partial transverse colon and fully exposing the tumor, we began to liberate the tumor from the right iliac vessel. Finally, we released the tumor from the right kidney, inferior vena cava, and abdominal aorta. The operation took 6 h and the volume of blood loss was 100 mL approximately.
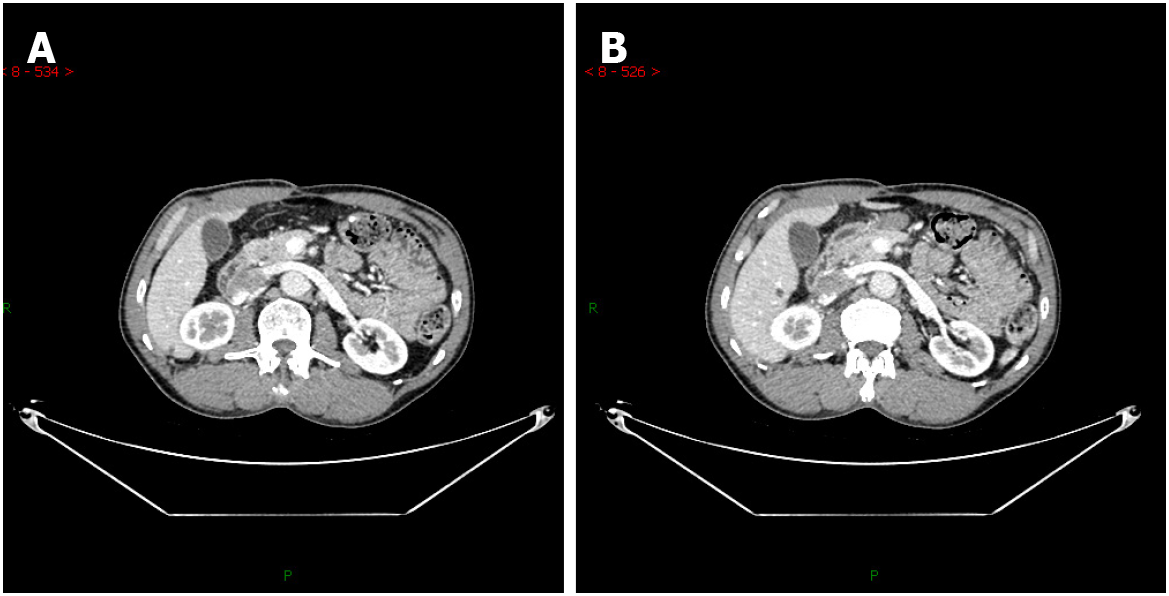
The hemoglobin level was 91.0 g/L (reference range, 120-160 g/L in men) on the 1st postoperative day. The postoperative course was uneventful, and the patient was discharged on the 6th postoperative day. At the final follow-up (about 16 mo after surgery), he was in good general condition, and a CT scan revealed no signs of tumor recurrence (Figure 4).
WDLPS is the second most common liposarcoma arising in the retroperitoneum[8]. WDLPS in the retroperitoneum carries higher risks of relapse[9-11]. Surgical resection is the standard of cure[11,12]. Macroscopic complete resection is essential to curative treatment[13]. Compared to complete resection, aggressive surgical policies reduce the local recurrence rate of primary retroperitoneal sarcomas, but it has not improved overall survival[14,15]. As for its asymptomatic nature in the early stage, WDLPS in the retroperitoneum is often diagnosed with a massive size[16]. Resection in such situations may involve multiple organs and vasculature, making it difficult to achieve clear resection margins[17]. It also carries a high risk of massive hemorrhage and hemodynamic instability. Contrast-enhanced CT is the most useful and widely available primary imaging technique[18]. The appearance of WDLPS on CT is a bland fat density mass[18]. CT provides size, consistency, and relations between the tumor and the adjacent tissue[19]. Hyper-accuracy three-dimensional reconstruction is a tool that provides more full-scale information of organs than does traditional CT. Three-dimensional reconstruction is also more helpful for diagnosis and operative planning[20]. It provides the surgeon with more detail regarding anatomical structures and more macroscopic images to select better surgery approaches and determine resection ranges. In our case, hyper-accuracy three-dimensional reconstruction of the abdomen revealed the intimate relationships between the adjacent organs and crucial vascular structures. This modality revealed that the right renal artery’s feeding artery had three branches, from the upper to the lower pole of the tumor. We also noted that the inferior vena cava and the right kidney adhered extensively with the tumor but had defined borders. The right kidney was displaced to the left lower quadrant and was partly involved by the tumor. The anatomical position of the left kidney was not affected. Because its density was similar to that of the tumor, we could not observe the right adrenal gland. We speculated that the tumor had already invaded the adrenal gland. According to the three-dimensional images, we identified and ligated the feeding artery precisely; this allowed us to minimize bleeding during the separation of the tumor and shortened the operative time substantially. Just as we observed preoperatively, the adventitia of the inferior vena cava and capsule of the right kidney were completely enclosed. Finally, we released the tumor from the adhesions to organs including the inferior vena cava, abdominal aorta, pancreas, and right kidney, with subsequent removal en bloc with the adrenal gland, which we confirmed on postoperative pathology.
Surgical resection of WDLPS is critical because of the high risk of recurrence. Retroperitoneal masses can complicate anatomical relationships, especially with blood vessels. Hyper-accuracy three-dimensional reconstruction of the abdomen or tumor is useful for operative planning owing to its intuitiveness and precise information regarding anatomical structures in both the tumor and nearby tissues. We recommend hyper-accuracy three-dimensional reconstruction when the tumor is large, and its anatomical relationships with nearby tissue are complex.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Novak M S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Zhang H
| 1. | Elias J Jr, Muglia VF. Magnetic Resonance Imaging of the Perirenal Space and Retroperitoneum. Magn Reson Imaging Clin N Am. 2019;27:77-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Ducimetière F, Lurkin A, Ranchère-Vince D, Decouvelaere AV, Péoc'h M, Istier L, Chalabreysse P, Muller C, Alberti L, Bringuier PP, Scoazec JY, Schott AM, Bergeron C, Cellier D, Blay JY, Ray-Coquard I. Incidence of sarcoma histotypes and molecular subtypes in a prospective epidemiological study with central pathology review and molecular testing. PLoS One. 2011;6:e20294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 335] [Cited by in RCA: 414] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 3. | Pham V, Henderson-Jackson E, Doepker MP, Caracciolo JT, Gonzalez RJ, Druta M, Ding Y, Bui MM. Practical Issues for Retroperitoneal Sarcoma. Cancer Control. 2016;23:249-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Gronchi A, Strauss DC, Miceli R, Bonvalot S, Swallow CJ, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro D, Hayes AJ, Honoré C, Fairweather M, Cannell A, Jakob J, Haas RL, Szacht M, Fiore M, Casali PG, Pollock RE, Raut CP. Variability in Patterns of Recurrence After Resection of Primary Retroperitoneal Sarcoma (RPS): A Report on 1007 Patients From the Multi-institutional Collaborative RPS Working Group. Ann Surg. 2016;263:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 390] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 5. | Ukimura O, Nakamoto M, Gill IS. Three-dimensional reconstruction of renovascular-tumor anatomy to facilitate zero-ischemia partial nephrectomy. Eur Urol. 2012;61:211-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 86] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 6. | Porpiglia F, Checcucci E, Amparore D, Piramide F, Volpi G, Granato S, Verri P, Manfredi M, Bellin A, Piazzolla P, Autorino R, Morra I, Fiori C, Mottrie A. Three-dimensional Augmented Reality Robot-assisted Partial Nephrectomy in Case of Complex Tumours (PADUA ≥10): A New Intraoperative Tool Overcoming the Ultrasound Guidance. Eur Urol. 2020;78:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 110] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 7. | Bertolo R, Autorino R, Fiori C, Amparore D, Checcucci E, Mottrie A, Porter J, Haber GP, Derweesh I, Porpiglia F. Expanding the Indications of Robotic Partial Nephrectomy for Highly Complex Renal Tumors: Urologists' Perception of the Impact of Hyperaccuracy Three-Dimensional Reconstruction. J Laparoendosc Adv Surg Tech A. 2019;29:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Vijay A, Ram L. Retroperitoneal liposarcoma: a comprehensive review. Am J Clin Oncol. 2015;38:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Zhang Q, Li JM, Liu JL, Wei YZ. [Evaluation of prognostic factors for liposarcoma]. Zhonghua Zhong Liu Za Zhi. 2019;41:943-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Vos M, Boeve WC, van Ginhoven TM, Sleijfer S, Verhoef C, Grünhagen DJ. Impact of primary tumor location on outcome of liposarcoma patients, a retrospective cohort study. Eur J Surg Oncol. 2019;45:2437-2442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 11. | Bagaria SP, Gabriel E, Mann GN. Multiply recurrent retroperitoneal liposarcoma. J Surg Oncol. 2018;117:62-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 12. | Beksac K, Aksel B, Yukruk FA, Kandemir O. Giant retroperitoneal dedifferentiated liposarcoma. Ann Ital Chir. 2017;6. [PubMed] |
| 13. | Crago AM, Dickson MA. Liposarcoma: Multimodality Management and Future Targeted Therapies. Surg Oncol Clin N Am. 2016;25:761-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 115] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 14. | Gronchi A, Lo Vullo S, Fiore M, Mussi C, Stacchiotti S, Collini P, Lozza L, Pennacchioli E, Mariani L, Casali PG. Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol. 2009;27:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 328] [Cited by in RCA: 350] [Article Influence: 20.6] [Reference Citation Analysis (0)] |
| 15. | Bonvalot S, Rivoire M, Castaing M, Stoeckle E, Le Cesne A, Blay JY, Laplanche A. Primary retroperitoneal sarcomas: a multivariate analysis of surgical factors associated with local control. J Clin Oncol. 2009;27:31-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 403] [Cited by in RCA: 446] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 16. | Mansfield SA, Pollock RE, Grignol VP. Surgery for Abdominal Well-Differentiated Liposarcoma. Curr Treat Options Oncol. 2018;19:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Trans-Atlantic RPS Working Group. Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the Trans-Atlantic RPS Working Group. Ann Surg Oncol. 2015;22:256-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 205] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 18. | Messiou C, Moskovic E, Vanel D, Morosi C, Benchimol R, Strauss D, Miah A, Douis H, van Houdt W, Bonvalot S. Primary retroperitoneal soft tissue sarcoma: Imaging appearances, pitfalls and diagnostic algorithm. Eur J Surg Oncol. 2017;43:1191-1198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 19. | Lahat G, Madewell JE, Anaya DA, Qiao W, Tuvin D, Benjamin RS, Lev DC, Pollock RE. Computed tomography scan-driven selection of treatment for retroperitoneal liposarcoma histologic subtypes. Cancer. 2009;115:1081-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Porpiglia F, Fiori C, Checcucci E, Amparore D, Bertolo R. Hyperaccuracy Three-dimensional Reconstruction Is Able to Maximize the Efficacy of Selective Clamping During Robot-assisted Partial Nephrectomy for Complex Renal Masses. Eur Urol. 2018;74:651-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 101] [Article Influence: 14.4] [Reference Citation Analysis (0)] |