Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.117
Peer-review started: June 18, 2021
First decision: September 28, 2021
Revised: October 4, 2021
Accepted: November 26, 2021
Article in press: November 26, 2021
Published online: January 7, 2022
Processing time: 194 Days and 16.8 Hours
Most greater tuberosity fractures can be treated without surgery but some have a poor prognosis. The surgical procedures for avulsion fractures of the humeral greater tuberosity include screw fixation, suture anchor fixation, and plate fixation, all of which have treatment-associated complications. To decrease surgical complications, we used a modified suture bridge procedure under direct vision and a minimally invasive small incision to fix fractures of the greater tuberosity of the humerus.
To investigate the clinical efficacy and outcomes of minimally invasive modified suture bridge open reduction of greater tuberosity evulsion fractures.
Sixteen patients diagnosed between January 2016 and January 2019 with an avulsion-type greater tuberosity fracture of the proximal humerus and treated by minimally invasive open reduction and modified suture bridges with anchors were studied retrospectively. All were followed up by clinical examination and radiographs at 3 and 6 wk, 3, 6 and 12 mo after surgery, and thereafter every 6 mo. Outcomes were assessed preoperatively and postoperatively by a visual analog scale (VAS), the University of California Los Angeles (UCLA) shoulder score, the American Shoulder and Elbow Surgeon score (ASES), and range of motion (ROM) for shoulders.
Seven men and nine women, with an average age of 44.94 years, were evaluated. The time between injury and surgery was 1-2 d, with an average of 1.75 d. The mean operation time was 103.1 ± 7.23 min. All patients achieved bone union within 3 mo after surgery. VAS scores were significantly decreased (P = 0.002), and the mean degrees of forward elevation (P = 0.047), mean degrees of abduction (P = 0.035), ASES score (P = 0.092) were increased at 3 wk. The UCLA score was increased at 6 wk (P = 0.029) after surgery. The average degrees of external rotation and internal rotation both improved at 3 mo after surgery (P = 0.012 and P = 0.007, respectively). No procedure-related deaths or incision-related superficial or deep tissue infections occurred.
Modified suture bridge was effective for the treatment of greater tuberosity evulsion fractures, was easier to perform, and had fewer implants than other procedures.
Core Tip: Greater tuberosity fractures are special proximal humerus fractures that are often accompanied by rotator cuff injury. We used a modified suture bridge procedure with a minimally invasive small incision under direct vision to fix fractures of the greater tuberosity. The technique reduces the risk of weakly or loosely fixed implants, and avoids secondary surgery to remove the screw and plate internal fixation. The limited incision and direct vision not only allows repair of rotator cuff injury but also eliminates the use of knotless anchors, reducing the cost of implants.
- Citation: Kong LP, Yang JJ, Wang F, Liu FX, Yang YL. Minimally invasive open reduction of greater tuberosity fractures by a modified suture bridge procedure. World J Clin Cases 2022; 10(1): 117-127
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/117.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.117
Proximal humerus fractures are common injuries, accounting for approximately 5% of all fractures[1]. About 20% involve the greater tuberosity and are often accompanied by rotator cuff injuries of varying severity. The greater tuberosity of the humerus is the point of attachment of the rotator cuff, which often pulls the fractured fragments apart after avulsion[2,3]. Most greater tuberosity fractures can be treated without surgery, but some have a poor prognosis because of shoulder joint pain, movement limitation, acromion impingement, limb weakness, and other functional disorders[4-6]. The main surgical procedures for simple avulsion fractures are screw fixation, suture anchor fixation, and plate fixation[3]. Open reduction and internal plate fixation are widely used but are not free of problems, such as relatively large incision, damage to blood circulation in the bone and periosteum, and influence on fracture healing[7]. Conventional plates and locking plates have differing effects on fracture management[8,9], with locking plates being associated with a higher than expected incidence of plate fixation complications, such as ischemic necrosis, delayed healing, malunion, nonunion, and implant failure[10-12]. Procedures using cannulated screws and washers are simple and of short duration, but the incidence of postoperative stiffness and pain is higher that seen with other procedures[13]. Arthroscopic double-row anchor suture procedures are expensive and complicated to perform[14-16]. Inability to achieve adequate reduction and fixation of severely displaced fracture fragments with wire anchors in an arthroscopic procedure can lead to postoperative stiffness[17]. Inspired by the repair of rotator cuff injuries using the suture bridge technique, we modified that procedure to fix avulsion fractures of the greater tuberosity of the humerus through a minimally invasive small incision under direct vision. The aim was to reduce surgical complications and improve treatment. In this study, we retrospectively evaluated the clinical outcomes of 16 patients, including resuming work activity as well as restoration of strength and function.
Patients with avulsion fractures of the greater tuberosity of the humerus confirmed by X-ray, computed tomography (CT) or magnetic resonance imaging were eligible for study inclusion, provided that the fractures were closed, surgically fixed within 3 wk, and followed-up for more than 1 year. The fractures were classified as described by Mutch et al[18]. Patients were excluded according to: (1) Split and compressed fractures of the greater tuberosity; (2) Fractures of the greater tuberosity associated with proximal humerus fracture; (3) Shoulder joint dysfunction before admission; or (4) Greater tuberosity fracture of the humerus combined with brachial plexus injury. Between January 2016 and January 2019, 16 patients with avulsed fractures of the greater tuberosity were treated by a single orthopedic trauma surgeon in our orthopedics department using minimally invasive open reduction by a modified suture bridge with anchors.
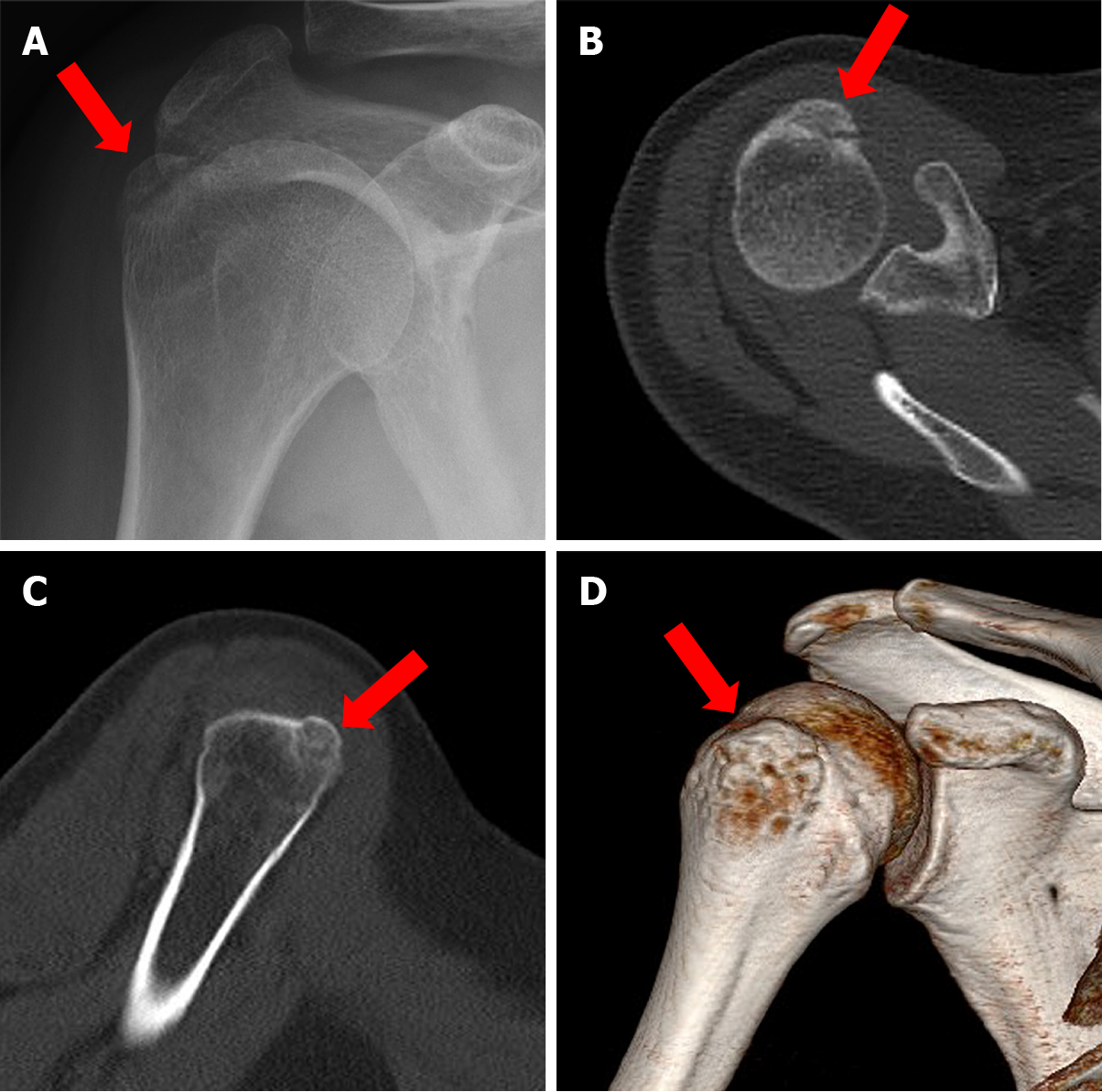
Avulsion fractures of the humeral greater tuberosity were diagnosed preoperatively by X-ray (Figure 1A), axial CT scan (Figure 1B), coronal CT scan (Figure 1C), and three-dimensional reconstruction image (Figure 1D) of the humerus. Fragment size and displacement were measured by the longest fracture line observed in coronal and axial views on CT. After surgery, true anteroposterior views (i.e., neutral, 20° of external rotation, and axillary) were taken at 3 and 6 wk, 3, 6 and 12 mo, and then every 6 mo.
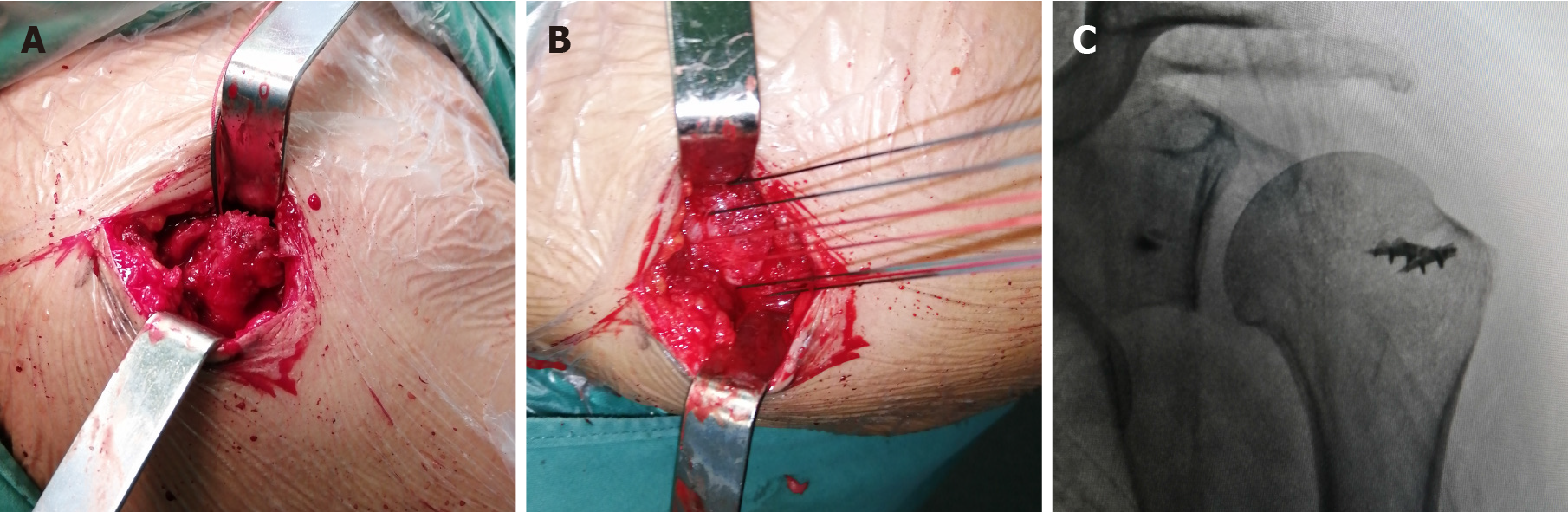
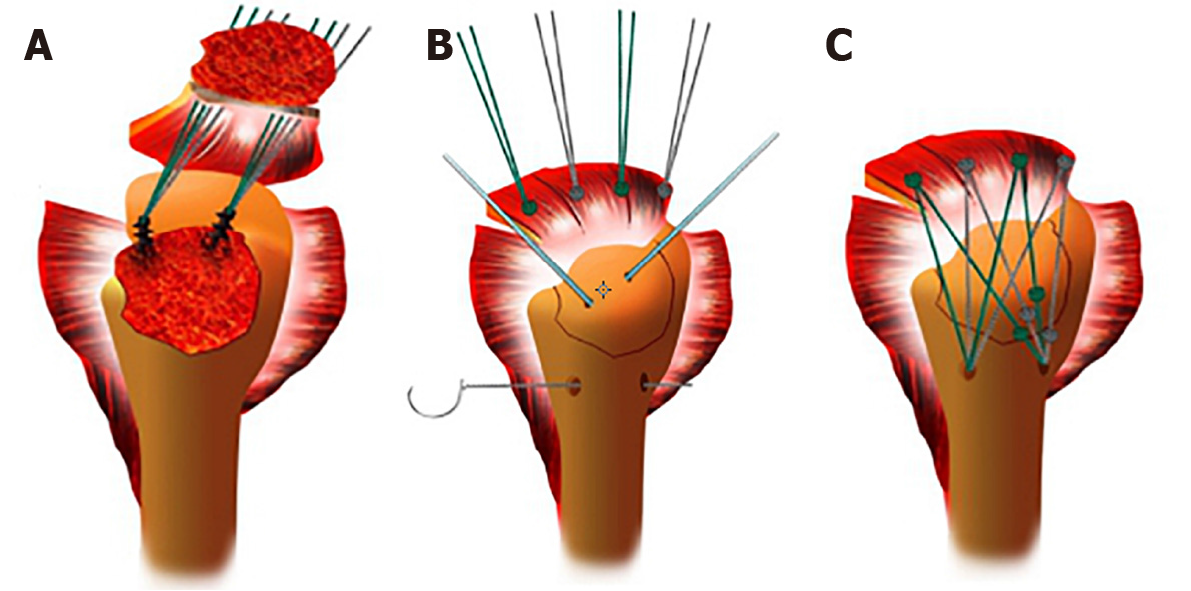
Surgery was performed under general anesthesia, with the patient in a 20° beach chair position. A 3-cm longitudinal skin incision was made from the anterolateral angle of the acromion. The deltoid muscle was dissected bluntly to expose the subacromial bursa. Supraspinatus and infraspinatus muscle avulsion fractures, greater tuberosity area fractures, multiple fracture fragments and rotator cuff lacerations were observed (Figure 2A). The broken end of the bone was cleaned, and the free bone fragments were removed. Two 5.0-mm anchors were inserted into the cartilaginous margin of the humeral head, and then the anchor lines were passed through the rotator cuff tissue and knotted (Figure 2B). A Kirschner wire was used for temporary fixation of the greater tuberosity fracture fragments, and a bone tunnel of appropriate length and 5-10 mm diameter (depending on the size of the fracture fragment) was drilled at the distal outer edge of the fracture line. One end of the anchor lines was guided through the bone tunnel by ordinary sutures and a knot was tied at the other end of the bone tunnel. The large tubercle fracture was reduced and fixed by the suture bridge technique, and the torn rotator cuff tissue was repaired. Intraoperative fluoroscopy showed the position of the anchors and the reduction of the fracture (Figure 2C). Figure 3 shows the main steps of the surgical procedure.
The arm was immobilized in a neutral position with a brace for 4 wk, to prevent internal rotation. The patients began pendulum exercises and continuous passive motion exercises within 48 h of surgery, similar to rehabilitation after rotator cuff repair. Passive forward flexion and abduction by use of a bar were allowed after 1 wk. After 4 wk, passive range of motion (ROM) exercises, including table sliding and stretching exercises, in addition to forward flexion in the supine position, were encouraged and preferably performed during or after a hot bath or shower. Three months after surgery, complete active ROM and strengthening exercises were allowed.
All patients were followed-up, with clinical examinations carried out at 3 and 6 wk, 3, 6 and 12 mo after surgery, and thereafter every 6 mo. Visual analog scale (VAS) pain assessment, American Shoulder and Elbow Surgeon (ASES) score, University of California Los Angeles (UCLA) shoulder score and ROM of the joint were used to assess the function of the affected shoulder joint. Active joint ROM was measured by the forward flexion of the scapula plane and the external and internal rotation of the lateral arm. Internal rotation was estimated by determining the highest spinal segment the patient could reach with the thumb. For ease of statistical analysis, spinal segments were converted into numbers: segments T1 through T12 were designated as 1 through 12, segments L1 through L5 were designated as 13 through 17, and the sacrum was designated as 18[19,20]. The pain scale, shoulder function score, and active ROM were assessed by an independent reviewer.
The statistical analysis was performed with SPSS Statistics 20.0 (IBM Corp., Armonk, NY, United States). Postoperative clinical results, including ASES, UCLA and VAS scores, and degrees of ROM, were each reported as mean ± SE. Differences were compared using Student’s t-tests. Proportional values were compared using the χ2 exact test, where applicable. For each test, a P value < 0.05 was considered significant.
The 16 patients included 7 men and 9 women, with an average age of 45 (range: 20-65) years. The injuries had resulted from falls for 9 patients, traffic accidents for 4, and a crash for 3. Six fractures involved the left shoulder and ten involved the right shoulder. The time between injury and surgery was between 1 d and 2 d, with an average of 1.75 d. Seven patients had other fractures. One had had a right clavicle fracture, one patient had a left tibia and fibula fractures, and one patient had a left radius fracture. The demographic data are summarized in Table 1.
| Patient | Sex | Age | BMI | Complication | Other fractures | Cause of injury | Side | Time between injury and surgery | |||
| HBP | DM | CHD | Other | ||||||||
| 1 | F | 63 | 22.86 | No | No | No | COPD | No | Fall | R | 1 |
| 2 | F | 52 | 27.66 | No | No | No | No | No | Fall | L | 2 |
| 3 | F | 62 | 20.57 | Yes | Yes | No | No | Right clavicle fracture | Crash | R | 2 |
| 4 | M | 25 | 23.62 | No | No | No | No | No | Traffic accident | L | 2 |
| 5 | M | 50 | 22.65 | No | No | Yes | CVA | No | Crash | L | 1 |
| 6 | M | 44 | 20.33 | Yes | No | No | No | No | Fall | L | 2 |
| 7 | M | 49 | 23.95 | No | No | No | No | No | Fall | R | 2 |
| 8 | F | 28 | 22.87 | No | No | No | No | No | Fall | R | 2 |
| 9 | F | 30 | 25.69 | No | No | No | No | No | Fall | R | 2 |
| 10 | F | 46 | 21.61 | No | No | No | No | No | Fall | L | 2 |
| 11 | M | 53 | 23.69 | No | Yes | No | No | No | Traffic accident | R | 2 |
| 12 | M | 20 | 26.33 | No | No | No | No | Left tibia and fibula fracture | Traffic accident | L | 2 |
| 13 | F | 30 | 28.57 | No | No | No | No | No | Crash | R | 2 |
| 14 | F | 65 | 21.50 | No | No | No | No | No | Traffic accident | R | 1 |
| 15 | M | 41 | 28.78 | No | No | No | HCV | No | Fall | R | 2 |
| 16 | F | 61 | 29.33 | Yes | No | No | No | Left radius fracture | Fall | R | 1 |
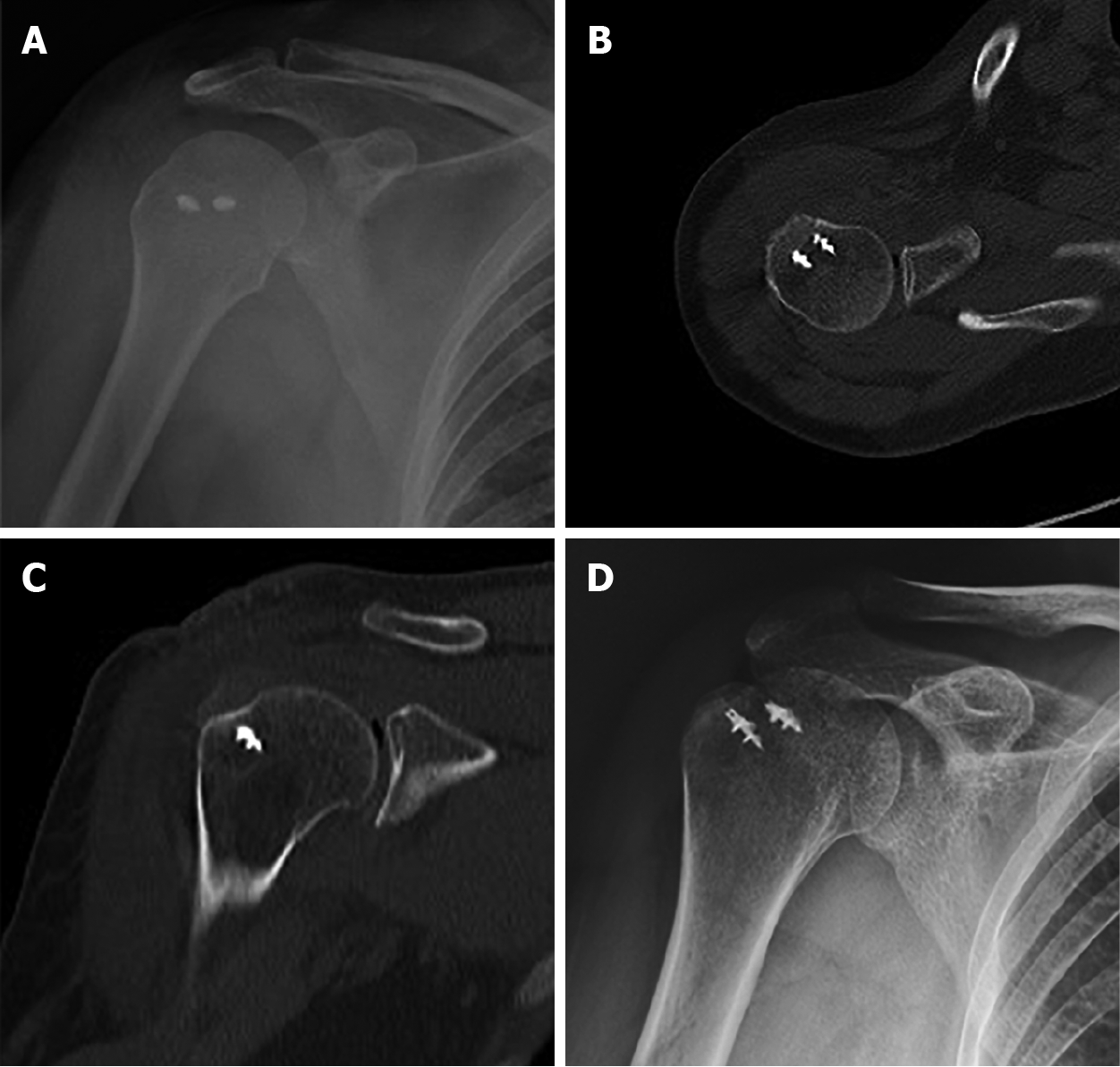
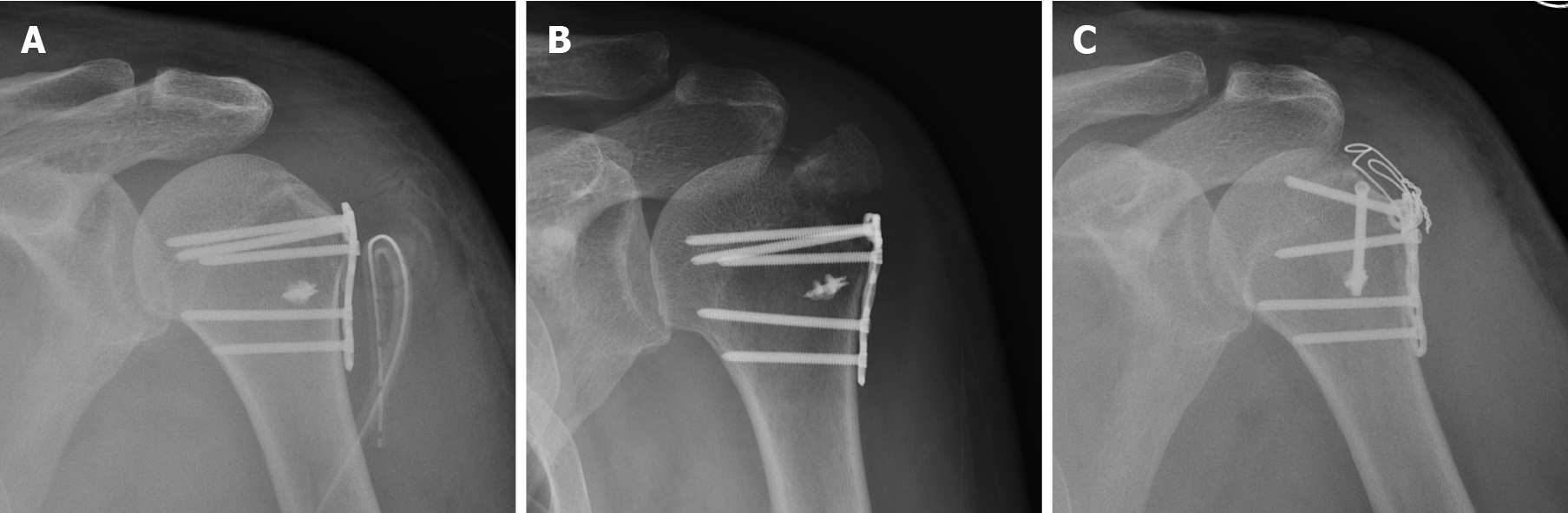
As shown in Table 2, the average height and width of the fracture fragments were 22.69 ± 1.88 (range: 10-33) mm and 16.94 ± 1.71 (range: 8-26) mm, respectively. The average displacement was 19.75 ± 2.05 (range: 5-30) mm. The average length of stay was 4.94 ± 0.25 (range: 4-7) d, mean procedure time was 103.1 ± 7.23 (range: 60-150) min, and mean operative blood loss was 51.88 ± 6.40 (range: 30-100) mL. Radiography and CT evaluation at 1 d after surgery demonstrated satisfactory reduction of the greater tuberosity (Figure 4A-C), and the fracture was healed at 1 mo after surgery (Figure 4D).
| Patients | Height of the fragments (mm) | Width of the fragments (mm) | Displacement (mm) | Operative time (h) | Bleeding volume (mL) | Length of stay (d) |
| 1 | 15 | 25 | 10 | 2 | 100 | 4 |
| 2 | 20 | 19 | 15 | 1 | 50 | 4 |
| 3 | 30 | 8 | 5 | 1.5 | 50 | 4 |
| 4 | 10 | 26 | 20 | 1.5 | 30 | 6 |
| 5 | 33 | 8 | 30 | 1.5 | 30 | 5 |
| 6 | 25 | 10 | 16 | 3 | 30 | 4 |
| 7 | 17 | 19 | 20 | 1 | 50 | 5 |
| 8 | 33 | 9 | 15 | 2.5 | 100 | 6 |
| 9 | 26 | 15 | 30 | 2 | 50 | 6 |
| 10 | 30 | 10 | 26 | 2 | 30 | 5 |
| 11 | 19 | 22 | 30 | 2 | 50 | 4 |
| 12 | 20 | 24 | 8 | 2 | 100 | 4 |
| 13 | 28 | 15 | 25 | 2 | 50 | 6 |
| 14 | 16 | 23 | 14 | 1.5 | 30 | 5 |
| 15 | 12 | 26 | 24 | 1 | 50 | 7 |
| 16 | 29 | 12 | 28 | 1.5 | 30 | 4 |
The mean patient follow-up 16.31 ± 1.01 (range: 12-24) mo. Plain radiographs or CT scans demonstrated solid fusion at 3 mo after surgery for all 16 patients. Postoperative outcomes observed at the follow-up evaluations from 3 wk to 1 year after surgery are shown in Table 3. Forward elevation was significantly improved at 3 wk, from 65.63° ± 1.82° preoperatively to 71.88° ± 2.41° (P = 0.047). External rotation improved from 9.38° ± 1.93° to 15.00° ± 2.19° at 3 mo (P = 0.012), and internal rotation improved from 17.56° ± 0.16° to 16.81° ± 0.21° at 3 mo (P = 0.007). Abduction increased from 48.13° ± 2.09° to 56.88° ± 3.38° 6 wk after surgery (P = 0.035). The VAS score significantly decreased from 6.19 ± 0.21 points to 5.19 ± 0.21 points at 3 wk (P = 0.002). The ASES score was significantly improved at 6 wk, from 38.69 ± 2.03 points to 43.56 ± 1.93 points (P = 0.092). The mean UCLA score improved from 9.94 ± 0.52 points to 11.5 ± 0.44 points at 6 wk (P = 0.029). The mean VAS score was 0.63 ± 0.22, UCLA score was 29.75 ± 0.90 at 12 mo, and the mean ASES score was 89.81 ± 1.69. The mean active forward flexion, external rotation, abduction and internal rotation of vertebral levels were 138.1° ± 2.23°, 33.44° ± 2.53°, 140.60° ± 3.35° and 13.31° ± 0.25°, respectively. None of the patients developed superficial or deep infections at the surgical site, and there were no wound healing problems in any of the patients. No sensory loss in the upper arm or shoulder associated with the axillary nerve or displacement was observed during the follow-up period. No procedure-related deaths occurred.
| Postoperative | ||||||
| Outcome | Preoperative | 3 wk | 6 wk | 3 mo | 6 mo | 12 mo |
| VAS | 6.19 ± 0.21 | 5.19 ± 0.21a | 3.81 ± 0.16a | 2.38 ± 0.20a | 1.0 ± 0.20a | 0.63 ± 0.22a |
| Forward elevation (degree) | 65.63 ± 1.82 | 71.88 ± 2.41a | 77.81 ± 2.12a | 95.31 ± 1.91a | 116.3 ± 2.07a | 138.1 ± 2.23a |
| External rotation (degree) | 8.13 ± 1.36 | 9.38 ± 1.93 | 10.94 ± 2.1 | 15 ± 2.19a | 27.81 ± 2.28a | 33.44 ± 2.53a |
| Abduction (degree) | 48.13 ± 2.09 | 50.63 ± 2.66 | 56.88 ± 3.38a | 82.5 ± 3.10a | 108.8 ± 3.52a | 138.8 ± 2.72a |
| Internal rotation | 17.56 ± 0.16 | 17.44 ± 0.16 | 17.19 ± 0.16 | 16.81 ± 0.21a | 15.19 ± 0.23a | 13.31 ± 0.25a |
| ASES | 38.69 ± 2.03 | 40.13 ± 2.05 | 43.56 ± 1.93a | 58.69 ± 1.82a | 74.44 ± 1.98a | 89.81 ± 1.69a |
| UCLA | 9.94 ± 0.52 | 10.19 ± 0.65 | 11.5 ± 0.44a | 14.69 ± 0.51a | 22.25 ± 0.64a | 29.75 ± 0.90a |
When selecting the optimal surgical fixation procedure for fractures of the greater tuberosity of the humerus, the deforming force caused by rotator cuff muscle elongation should be taken into account. The insertions of the supraspinatus, infraspinatus, and teres minor are on the greater tuberosity of the humerus, and their coupling force controls the function of the shoulder joint. Ogawa et al[21] reported that most fractures of the greater tubercle of the humerus (57%) involve the supraspinatus and supraspinatus, resulting in upward and backward displacement of the tubercle in the same direction as the rotator cuff pull by an intact supraspinatus tendon, and noted that posterior displacement is important because it is often underestimated and delays treatment. On the other hand, Mutch et al[18,22] reported that 20% of the fractured pieces of the greater tuberculum shifted downward. Bahrs et al[23] reported that downward displacement occurred in 25.2% of fractures, suggesting that it might be caused by direct downward force or the impact of the greater tuberculum on the acromion during extreme abduction of the upper limb. With anterior dislocation of the shoulder, the shear force at the glenoid margin can also lead to fracture of the greater tuberosity. Figure 5 shows a case of steel plate treatment failure for a greater tuberosity fracture. Its attachment to the rotator cuff moves the greater tuberosity of the humerus closer to the shoulder joint, and because of its anatomical position, it is difficult achieve fixation with traditional steel plates. The greater tuberosity was displaced because rotator cuff traction was neglected. After a second operation, the fracture was fixed with screws and steel wire against rotator cuff pull, and satisfactory results were obtained.
The suture bridge technique covers the fracture block with high-strength thread at the end of the anchor, which effectively disperses the shear and torsion forces of the suture line to achieve satisfactory suture and fixation effects. The network structure formed by the high-strength thread crossing firmly fixes the avulsion bone and rotator cuff. Lin et al[24] reported that the supraspinatus muscle has obvious superiority to the traction tension of the greater tuberosity fragment using suture bridge in comparison to canulated screw fixation. The fracture fragment covered 100% of the rotator cuff footprint by the suture bridge technique. It not only reduced the tension of the supraspinatus muscle but also provided maximum contact area, which increased the fixation strength of the fracture block and decreased gap formation. In this study, clinical follow-up was conducted at 3 and 6 wk, 3, 6 and 12 mo after surgery, and every 6 mo afterward. Figure 4 shows good reduction of the greater tuberosity and a firmly fixed fractured mass. Operative records (Table 2) and follow-up results (Table 3) showed that the surgical trauma was small, postoperative complications were few, pain was light, and recovery was rapid. The suture bridge procedure achieved good therapeutic results and patient benefits. Minimally invasive open reduction by a modified suture bridge with anchors reconstructed the original footprint area of the rotator cuff, which allowed an increase in surface and fixation area. Our technique allows for a broad contact surface and fixation area, the stability of the greater tuberosity was enhanced, which facilitated fracture union and allowed early functional exercise. We also found that an even distribution of load was provided by the four fixation points, which dispersed stress and was conducive to recovery of rotator cuff function.
The double-row anchor bridge suture technique has been widely used in arthroscopic surgery[25]. Compared with traditional surgical methods, it has better biomechanical advantages for repairing rotator cuff injuries and fixing fractures of the greater tuberosity[17]. However arthroscopic surgery also has some limitations, including complicated operations and longer operation time that increase surgical risk, and the procedures have a high learning curve[26]. It has also been reported that arthroscopic double-row anchoring is unlikely to adequately reduce and repair severely displaced fracture fragments and may even damage the rotator cuff[27]. Using minimally invasive open reduction with suture bridge technology can overcome the disad
Rouleau et al[3] described a surgical approach similar to ours that used three anchors in the proximal row, with two anchors or an interference screw placed distal to the fracture bed in the distal row. They did not drill a bone tunnel at the distal outer edge of the fracture line, but both techniques use the suture bridge technique to cover the fracture block and 100% of the rotator cuff footprint, providing maximum contact area and increasing the fixation strength of the fracture block. However, our technique eliminates the use of knotless anchors, which not only reduces the cost of implants but also reduces the rejection reaction of some patients with external anchors and reduces the risk of surgical infection. For some patients with osteoporosis, the use of knotless anchors increases the risk of anchor extraction, leading to failure of fixation. Also, more procedure steps, a longer procedure time, and a longer learning curve are involved in positioning and inserting knotless anchors. Although there is a possibility of suture cut-out with our surgical approach to the bone tunnel, our follow-up results (Table 3) indicate that the efficacy of this technique is reliable. We use more than three sutures through the bone tunnel, and by selecting the right location of the bone tunnel, we can reduce the pressure and the risk of suture cut-out. In short, our technique is not only effective but also has fewer implants, lower cost, a simpler surgical procedure, and easier promotion compared with their technique.
However, this technique is only suitable for avulsion fractures of the greater tuberosity of the humerus. An analysis of 199 cases by Mutch et al[18] in 2014, described avulsion fractures (smaller fracture mass, horizontal fracture line), crackle fractures (larger fracture mass, vertical fracture line), and compression fractures (internal displacement of fracture mass into the cancellous bone). In this study, the average height and width of the fracture blocks were 22.69 ± 1.88 (range: 10-33) mm and 16.94 ± 1.71 (range: 8-26) mm. Because the avulsion fracture fragments were small, it was difficult to fix the blocks with canulated screws. The avulsion fracture block is often located above the greater tuberosity, and plates cannot be positioned properly, which leads to complications and possible failure of fixation. However, the split fracture block is so large that is difficult to maintain stability of the fracture fragment with the suture bridge. If the compression fracture block is stable, then nonoperative treatment is generally adopted.
Our study has some limitations. First, it was a retrospective study without a control group using other fixation techniques, such as locking compression plates or arthroscopic fixation. Second, the average age of the patients was 44.94 (range: 20-65) years. As there were few patients with overt osteoporosis, to determine whether they would be suited for this procedure will require further investigation. Last, the sample size was small, with only 16 cases, and the follow-up durations were no more than 2 years. Further evaluation of the effectiveness of our minimally invasive suture bridge open reduction technique for the treatment of fractures of the greater tuberosity requires accumulation of more cases, longer follow-up, and inclusion of a control group using other treatment methods.
Minimally invasive open reduction of greater tuberosity avulsion fractures by a modified suture bridge with anchors of the humerus yielded an acceptable clinical result, with firm fixation that allowed early postoperative passive shoulder movement. The technique requires fewer implants than other procedures, is simpler to perform, and easier to begin using compared with other techniques. It is an efficient and reliable method for the treatment of avulsion-type greater tuberosity fractures of the humerus.
Most greater tuberosity fractures can be treated without surgery but some have a poor prognosis. The main surgical procedures for avulsion fractures of the humeral greater tuberosity are screw fixation, suture anchor fixation, and plate fixation; there are some complications after surgery.
Our experience with repair of rotator cuff injuries by the suture bridge technique led us adapt it to fixation of fractures of the greater tuberosity of the humerus using a modified minimally invasive small incision under direct vision. The aim was to improve patient care and reduce surgical complications.
The purpose of the study was to describe a modified minimally invasive surgical technique for the treatment of avulsion fractures of the greater tuberosity of the humerus. To this end, we investigated the clinical efficacy and outcomes of the procedure.
Sixteen patients with avulsion fractures of the greater tuberosity of the proximal humerus and were treated with minimally invasive open reduction by modified suture bridges with anchors between January 2016 and January 2019 were retrospectively studied. All were followed-up by clinical examinations and radio
All patients achieved bone union within 3 mo after surgery. VAS scores significantly decreased within 3 wk after surgery (P = 0.002). The mean degrees of forward elevation increased at 3 wk (P = 0.047). The mean degrees of abduction, ASES and UCLA scores increased at 6 wk (P = 0.035, P = 0.092 and P = 0.029, respectively). The average degrees of external and internal rotation improved at 3 mo (P = 0.012 and P = 0.007, respectively).
Minimally invasive open reduction of avulsion fractures of the greater tuberosity of the humerus by a modified suture bridge with anchors yielded an acceptable clinical result, with firm fixation and allowed early postoperative passive shoulder movement. The technique requires fewer implants, is a simpler procedure, and is easier to begin using compared with other techniques. It is an effective and reliable method for the treatment of avulsion fractures of the greater tuberosity of the humerus.
This retrospective study lacked a control group using other fixation techniques, such as locking compression plates or arthroscopic fixation. Further evaluation of the effectiveness of our minimally invasive suture bridge open reduction technique for the treatment of fractures of the greater tuberosity requires accumulation of more cases, longer follow-up, and inclusion of a control group using other treatment methods.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Buckley RE, Pavone V S-Editor: Gao CC L-Editor: A P-Editor: Gao CC
| 1. | Vijayvargiya M, Pathak A, Gaur S. Outcome Analysis of Locking Plate Fixation in Proximal Humerus Fracture. J Clin Diagn Res. 2016;10:RC01-RC05. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Kim DR, Noh YM, Lee SY. Arthroscopic Reduction and Suture Bridge Fixation of a Large Displaced Greater Tuberosity Fracture of the Humerus. Arthrosc Tech. 2019;8:e975-e985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Rouleau DM, Mutch J, Laflamme GY. Surgical Treatment of Displaced Greater Tuberosity Fractures of the Humerus. J Am Acad Orthop Surg. 2016;24:46-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Chen YF, Zhang W, Chen Q, Wei HF, Wang L, Zhang CQ. AO X-shaped midfoot locking plate to treat displaced isolated greater tuberosity fractures. Orthopedics. 2013;36:e995-e999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | White EA, Skalski MR, Patel DB, Gross JS, Tomasian A, Heckmann N, Matcuk GR Jr. Isolated greater tuberosity fractures of the proximal humerus: anatomy, injury patterns, multimodality imaging, and approach to management. Emerg Radiol. 2018;25:235-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Sofu H, Gürsu S, Koçkara N, Oner A, Issın A, Camurcu Y. Recurrent anterior shoulder instability: Review of the literature and current concepts. World J Clin Cases. 2014;2:676-682. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 29] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (3)] |
| 7. | Alberio RL, Del Re M, Grassi FA. Minimally Invasive Plate Osteosynthesis for Proximal Humerus Fractures: A Retrospective Study Describing Principles and Advantages of the Technique. Adv Orthop. 2018;2018:5904028. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | George MS. Fractures of the greater tuberosity of the humerus. J Am Acad Orthop Surg. 2007;15:607-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Augat P, von Rüden C. Evolution of fracture treatment with bone plates. Injury. 2018;49 Suppl 1:S2-S7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (1)] |
| 10. | Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009;18:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 261] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 11. | Kavuri V, Bowden B, Kumar N, Cerynik D. Complications Associated with Locking Plate of Proximal Humerus Fractures. Indian J Orthop. 2018;52:108-116. [PubMed] |
| 12. | Panagiotopoulou VC, Varga P, Richards RG, Gueorguiev B, Giannoudis PV. Late screw-related complications in locking plating of proximal humerus fractures: A systematic review. Injury. 2019;50:2176-2195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Yoon TH, Choi CH, Choi YR, Oh JT, Chun YM. Clinical outcomes of minimally invasive open reduction and internal fixation by screw and washer for displaced greater tuberosity fracture of the humerus. J Shoulder Elbow Surg. 2018;27:e173-e177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Huang AL, Thavorn K, van Katwyk S, MacDonald P, Lapner P. Double-Row Arthroscopic Rotator Cuff Repair Is More Cost-Effective Than Single-Row Repair. J Bone Joint Surg Am. 2017;99:1730-1736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Bisson L, Zivaljevic N, Sanders S, Pula D. A cost analysis of single-row vs double-row and suture bridge rotator cuff repair methods. Knee Surg Sports Traumatol Arthrosc. 2015;23:487-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Song HS, Williams GR Jr. Arthroscopic reduction and fixation with suture-bridge technique for displaced or comminuted greater tuberosity fractures. Arthroscopy. 2008;24:956-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Ji JH, Shafi M, Song IS, Kim YY, McFarland EG, Moon CY. Arthroscopic fixation technique for comminuted, displaced greater tuberosity fracture. Arthroscopy. 2010;26:600-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Mutch J, Laflamme GY, Hagemeister N, Cikes A, Rouleau DM. A new morphological classification for greater tuberosity fractures of the proximal humerus: validation and clinical implications. Bone Joint J. 2014;96-B:646-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 60] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Kim SJ, Choi YR, Lee HH, Chun YM. Surgical Results of Delaminated Rotator Cuff Repair Using Suture-Bridge Technique With All-Layers or Bursal Layer-Only Repair. Am J Sports Med. 2016;44:468-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Park JS, Park HJ, Kim SH, Oh JH. Prognostic Factors Affecting Rotator Cuff Healing After Arthroscopic Repair in Small to Medium-sized Tears. Am J Sports Med. 2015;43:2386-2392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 133] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 21. | Ogawa K, Yoshida A, Ikegami H. Isolated fractures of the greater tuberosity of the humerus: solutions to recognizing a frequently overlooked fracture. J Trauma. 2003;54:713-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Mutch JA, Rouleau DM, Laflamme GY, Hagemeister N. Accurate Measurement of Greater Tuberosity Displacement Without Computed Tomography: Validation of a Method on Plain Radiography to Guide Surgical Treatment. J Orthop Trauma. 2014;28:445-451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Bahrs C, Lingenfelter E, Fischer F, Walters EM, Schnabel M. Mechanism of injury and morphology of the greater tuberosity fracture. J Shoulder Elbow Surg. 2006;15:140-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 67] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Lin CL, Hong CK, Jou IM, Lin CJ, Su FC, Su WR. Suture anchor vs screw fixation for greater tuberosity fractures of the humerus--a biomechanical study. J Orthop Res. 2012;30:423-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 25. | Li R, Cai M, Tao K. Arthroscopic reduction and fixation for displaced greater tuberosity fractures using the modified suture-bridge technique. Int Orthop. 2017;41:1257-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Lee SU, Jeong C, Park IJ. Arthroscopic fixation of displaced greater tuberosity fracture of the proximal humerus. Knee Surg Sports Traumatol Arthrosc. 2012;20:378-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Bhatia DN, van Rooyen KS, du Toit DF, de Beer JF. Surgical treatment of comminuted, displaced fractures of the greater tuberosity of the proximal humerus: a new technique of double-row suture-anchor fixation and long-term results. Injury. 2006;37:946-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |