Published online Nov 16, 2013. doi: 10.12998/wjcc.v1.i8.249
Revised: September 20, 2013
Accepted: October 17, 2013
Published online: November 16, 2013
Processing time: 98 Days and 5 Hours
AIM: To evaluate the effect of priming the tooth surface with 2% chlorhexidine gluconate on antibacterial activity of resin cement.
METHODS: Ten patients in whom a single missing tooth was present on both the right and left side in the upper or lower arch were selected. Two fixed partial dentures (FPDs) in each patient on the right and left side were planned. Each FPD was assigned either to the control or test group. In the control group, FPD was luted with resin cement and in the test group, the tooth surface was primed with 2% chlorhexidine gluconate before luting with resin cement. Bacteriological samples were collected at base line level, as the patient came to the outpatient department before the start of any treatment, 5 wk prior to cementation of FPD and at 13 wk (8 wk after final cementation). Microbiological processing of all samples was done and the results were statistically analyzed.
RESULTS: In the test group, a predominance of aerobic/facultative gram positive cocci rod was seen which indicates a healthy periodontal site, whereas in the control group, a predominance of anaerobic gram negative rods was present which indicates an unhealthy periodontal condition. This is evident by the fact that the anaerobic bacteria percentage in the control sample is 57% and 15% in the test sample after 13 wk, whereas the aerobic/facultative bacteria percentage is 43% in the control sample and 85% in the test sample after 13 wk. The percentage of gram negative bacteria in the control sample is 61% and in the test sample is 20% after 13 wk, whereas the percentage of gram positive bacteria in the control sample is 39% and in the test sample is 80% after 13 wk. The shift from anaerobic gram negative bacteria to aerobic gram positive bacteria is clearly seen from the control to test sample after 13 wk.
CONCLUSION: The present study demonstrated that priming the tooth surface with 2% chlorhexidine gluconate may enhance antibacterial activity of the resin cement.
Core tip: Fixed prosthodontics is one of the most sought after services by patients in dentistry, but periodontal problems around fixed partial dentures have been the Achilles heel to date, reducing the longevity of the prosthesis. Generally, cements that are used for luting fixed partial dentures might not be as effective in controlling periodontal problems. Resin cement is the cement of choice nowadays but lacks antibacterial activity. The role of 2% chlorhexidine in reducing periodontal problems has been established in dentistry. The present study focuses on a method to increase the antibacterial activity of the cement by priming the tooth surface with chlorhexidine 2% before luting the fixed partial dentures.
- Citation: Saini M, Singh Y, Garg R, Pandey A. Priming the tooth surface with chlorhexidine and antibacterial activity of resin cement. World J Clin Cases 2013; 1(8): 249-255
- URL: https://www.wjgnet.com/2307-8960/full/v1/i8/249.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i8.249
The establishment and maintenance of periodontal health is a prerequisite for long term success for fixed prosthesis. Periodontal diseases have been associated with bacterial origin[1]. Retention of plaque around fixed prosthesis giving rise to periodontal problems has been Achilles heel to date[2].
There are various reasons for the existence of periodontal diseases. Traumatic preparations, faulty impression procedures, poor provisional restorations with unsuitable laboratory support and improper crown contour[3,4] cause insult to the gingival tissues. Subgingival margin[5] placement is also associated with undesirable effects on the periodontium and is considered to be one of the causes for failure in fixed prosthesis. Despite advancements in materials used for castings and impression making for fixed partial dentures (FPD), we still depend on the integrity of the luting cement[6-8] to maintain the marginal seal. Ideal luting cement should possess low viscosity, optimal film thickness, low solubility, long working time with rapid set at oral temperature, high compressive and tensile strengths, high proportional limit, adhesion to tooth structure and restorative materials, radiopacity, translucency, biocompatibility and anticariogenic activity[9-11]. Microleakage solubility and disintegration have been common problems among a number of luting agents (water-activated polycarboxylate cement, glass ionomer, zinc oxide-eugenol, silicophosphate, zinc phosphate, etc.). These unwanted properties cause growth of micro-organisms in and around fixed prosthesis. Therefore, cements with antibacterial properties have been studied in the past and have been co-related with long term success of FPD[12-15].
The antimicrobial efficacy of 2% chlorhexidine gluconate (CHX) is well established. It is bactericidal against gram positive and gram negative oral microorganisms. CHX is retained on tooth surfaces, pellicle substances, plaque and mucous membranes and is released over several hours. This phenomenon is substantial and can be accounted for the prolonged in vivo antiplaque effect of CHX. The effectiveness of CHX has been well documented for reduction of periodontal inflammation when used in the form of a mouth rinse[16,17]. Chlorhexidine also promotes the formation of a hybrid layer when resin cement is[18,19] applied to a tooth surface. CHX has been seen in the past to improve the physical properties of the resin cement. It has been found to diminish the loss of bonding effectiveness over time, associated with etch-and-rinse and self-etch cements[20]. Chlorhexidine application in etch-rinse resin cement also reduced microleakage at gingival margins after storage[21]. Antibacterial activity of zinc polycarboxylate cement was increased by using CHX based cement compared to water based cement[22]. The same effect of CHX is also expected in resin cements. The aim of this clinical study was to evaluate the effect of priming the tooth surfaces with 2% CHX on antibacterial activity of resin cement.
Patients who required fixed prosthodontic therapy were selected from the outpatient department (OPD) of Subharti Dental College, Meerut, UP. The procedures were explained in detail to the patients and a written informed consent was taken before beginning with the treatment. Patients with any systemic disease or who were taking medications (including antibiotics, antimicrobials or fluoride rinses) affecting gingival health 2 mo before the baseline data collection were excluded from study. At the beginning of the study, all subjects demonstrated a mean Silness-Löe Plaque Index[23] and Löe-Silness Gingival Index[24] of less than 2 and probing sulcus depths of less than 4 mm at the abutment teeth. Clinical measurements were made at 6 points around each tooth. Ten patients in whom a single missing tooth was present on both the right and left side in the upper or lower arch were selected. Abutment teeth were evaluated for tooth preparation. Porcelain fused to metal FPD was planned for each patient and thus two FPDs in each patient on the right and left side were planned. Each FPD was assigned either to the control group or test group. In the control group, resin cement (Multilink Automix, Ivoclar Vivadent, Mumbai, India) was used as the luting agent and in test group, the abutment tooth surface was primed with 2% CHX (Hexidine, ICPA, India) before luting with resin cement.
The prepared tooth is etched with Total Etch (Ivoclar Mumbai India) for 15 s. Total Etch has 30% phosphoric acid. Cotton pellets saturated with 2% chlorhexidine are placed on the prepared tooth for 60 s and then dried for 10 s[21]. Primer A and B are mixed in 1:1 ratio and applied to the prepared tooth surface for 30 s (as per scientific documentation provided by manufacturer). The inner surface of FPD is sandblasted and cleaned in an ultrasonic unit for 1 min. The restoration is thoroughly rinsed with water and dried. Monobond plus is applied with a brush for 60 s to the inner surface of the restoration and dispersed with a strong stream of air. Finally, Multilink Automix luting cement is applied on to the restoration’s inner surface and the restoration is luted. After the cementation was done, excess cement was removed and post cementation instructions were given to the patient[18].
Bacteriological samples were collected 3 times. One at base line level, as patient came to OPD before start of any treatment; one at 5 wk prior to cementation of FPD; and one at 13 wk (8 wk after final cementation).
After bacteriological samples were collected at the baseline visit, all patients received oral prophylaxis treatment and were given oral hygiene instructions. Porcelain fused to metal FPDs was fabricated with minimal trauma and a chamfer finish line was given in all preparations. The margins were located at the gingival margin. Forty teeth were prepared for FPD in total. A total of 12 subgingival plaque specimens (2 tests, 2 control samples per patient at three different sample times) were collected for each patient. Thus, a total of 120 samples were collected in ten patients.
Subgingival microbiological samples were obtained by inserting sterile standardized endodontic paper points (Dia Dent, South Korea) for 30 s into the gingival sulcus subjacent to the restoration. Paper points were gently placed at 4 locations (mesiobuccal, distobuccal, midbuccal and midlingual/palatal regions) on each abutment tooth after isolating the quadrant from saliva contamination with the help of cotton wool rolls and a saliva ejector. All four samples per tooth were pooled into a single broth, providing one broth sample per tooth per patient.
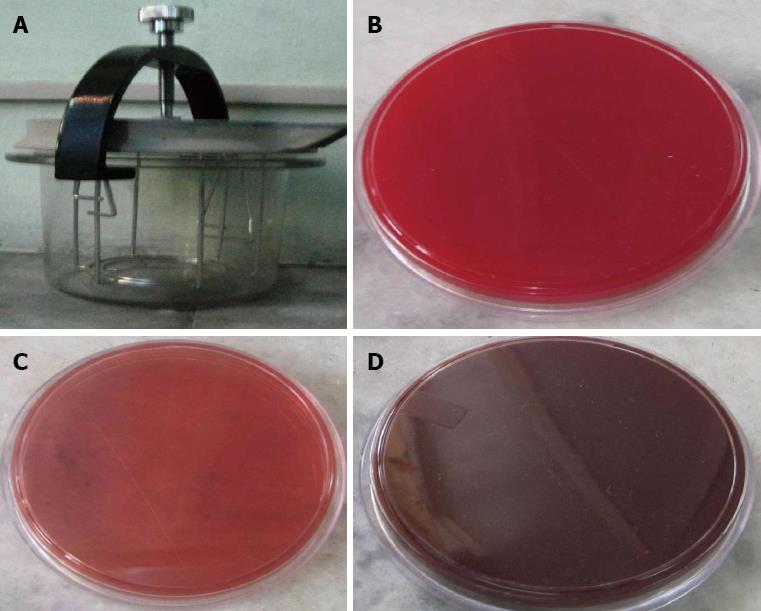
The microbiological samples obtained from all subgingival sites were inserted into a Robertson’s cooked medium broth and dispatched immediately to the Microbiology Department for anaerobic and aerobic culture procedures. For anaerobic bacteria, samples were cultured on (1) brucella blood agar; (2) kanamycin-vancomycin laked blood agar; and (3) Bacteroides bile esculin agar (HiMedia Laboratories Pvt. Ltd., Mumbai, India). The plates were placed into an anaerobic chamber (Figure 1) containing a gas mixture of 80% to 90% nitrogen, 5% to 10% hydrogen, and 5% to 10% carbon dioxide (CO2), and biological control (Pseudomonas aeruginosa) incubated at 37 °C for 48 to 72 h. Later, aerotolerance tests were performed for each different colony, prior to gram-staining, to determine the purity, spore formation and morphologies. Catalase and pigment activities were also evaluated. API 20A and ID32A strips (BioMerieux SA, France) were used for identification of anaerobes. Categorization of bacterial pathogenicity was done according to whether the organism was associated with progressive periodontal disease (periodontally suspected bacteria or not-periodontally suspected bacteria).
Samples were cultured for aerobic bacteria on (1) 5% blood agar (Figure 1B); (2) MacConkey agar (Figure 1C); and (3) chocolate (Figure 1D) (with vancomycin, clindamycin and bacitracin) agars in laminar air flow (Labline instruments, Kochi, India). Blood and MacConkey agars were incubated aerobically and the chocolate agar was incubated in air + 5% CO2 at 37 °C for 24 h. Isolated bacteria were identified by using both standard microbiological methods and API automated systems.
Table 1 describes the overall distribution of bacteria in test and control samples at all sample times (2 test and 2 control samples per subject at baseline, 5 wk and 13 wk). Out of 338 bacterial colonies: 42.3% were facultative gram positive cocci; 13.4% were facultative gram negative bacilli; 11.8% were aerobic gram negative bacilli; 10.9% were aerobic gram positive bacilli; 9.2% were aerobic gram negative bacilli; 5 were aerobic and anaerobic gram negative cocci; and 2% anaerobic gram positive cocci. Pathogenic anaerobic gram negative bacilli were significantly less in the test group (1.9%) than in the control group (9.3%). Pathogenic anaerobic gram negative cocci were also significantly less in the test group (3.9%) than in the control group (6.04%). The total number of pathogenic bacteria was less in the test group (n = 20) than in the control group (n = 39).
| Bacteria type | Control (n = 182) | Test (n = 156) | Total | ||
| PSB | N-PSB | PSB | N-PSB | ||
| Facultative GNB | 2 (1.1) | 17 (9.3) | 5 (3.2) | 21 (13.5) | 45 (13.4) |
| Aerobic GPB | 6 (3.2) | 11 (6.04) | - | 20 (12.8) | 37 (10.9) |
| Aerobic GNC | - | 9 (4.9) | - | 8 (5.1) | 17 (5.02) |
| Facultative GPC | 3 (1.64) | 62 (34.1) | 6 (3.9) | 72 (46.2) | 143 (42.3) |
| Anaerobic GNB | 17 (9.3) | 21 (11.5) | 3 (1.9) | - | 40 (11.8) |
| Anaerobic GPB | - | 16 (8.8) | - | 15 (9.6) | 31 (9.2) |
| Anaerobic GNC | 11 (6.04) | - | 6 (3.9) | - | 17 (5) |
| Anaerobic GPC | - | 7 (3.8) | - | - | 7 (2.1) |
| Totals | 39 | 143 | 20 | 136 | 338 |
Tables 2 and 3 represent the distribution and number of bacteria isolated at all sample times. In the control group at base line level, predominantly Streptococci (32.8%), Haemophilus (13.1%) and Campylobacter (7.8%) were present, as well as aerobic/facultative gram positive cocci and rods atmosphere. In the test group at baseline level, predominantly Streptococci (35.7%), Campylobacter (9.5%) and Diptheroid (9.5%) were present, as well as aerobic/facultative gram positive cocci and rods atmosphere. The P value at baseline was 0.595. The application of a χ2 test shows that the distribution of bacteria does not differ significantly at baseline at 5% level of significance.
| Baseline | 5 wk | 13 wk | ||||
| Control | Test | Control | Test | Control | Test | |
| Actinomycesnaeslundii FG+veR | 3 (3.9) | - | - | - | 1 (1.7) | 1 (1.6) |
| Actinomycesviscosus FG+veR | 2 (2.6) | - | - | - | 1 (1.7) | 1 (1.6) |
| Bifidobacterium spp FG+veR | 4 (5.2) | 3 (7.1) | 2 (4) | 2 (3.6) | 1 (1.7) | 3 (4.9) |
| Clostridium spp FG+veR | - | - | 7 (14) | 6 (11.3) | - | - |
| Diphtheroid bacilli AG+veR | 2 (2.6) | 4 (9.5) | 2 (4) | 2 (3.6) | 3 (5.3) | 1 (1.6) |
| Escherichia coli FG-veR | - | - | 1 (2) | 2 (3.6) | - | - |
| Eubacterium spp FG+veR1 | 1 (1.3) | - | - | 2 (3.6) | - | - |
| Fusobacteriumnucleatum AnG-veR1 | 2 (2.6) | - | 3 (6) | 4 (7.5) | 8 (14.2) | - |
| Haemophilus spp FG-veR | 10 (13.1) | 3 (7.1) | 4 (8) | 2 (3.6) | 5 (8.9) | 3 (4.9) |
| Coagulase-negative Staphylococci FG+veC | 2 (2.6) | 2 (4.7) | 2 (4) | 1 (1.8) | - | 4 (6.5) |
| Neisserria spp AG-veC | 8 (10.5) | 2 (4.7) | 2 (4) | 2 (3.6) | 1 (1.7) | - |
| Peptostreptococcus AnG+veC | 5 (6.5) | - | - | - | - | - |
| Porphyromonasgingivalis AnG-veR1 | - | - | - | - | 2 (3.2) | - |
| Prevotellaintermedia AnG-veR1 | 1 (1.3) | 1 (2.3) | 1 (2) | 1 (1.8) | 8 (14.2) | - |
| Propionibacteriumgranulosum FG+veR | - | 1 (2.3) | - | - | - | - |
| Staphylococcus aureus FG+veC | 2 (2.6) | 1 (2.3) | 3 (6) | 7 (13.2) | - | 2 (3.2) |
| Veillonellaparvula AnG-veC1 | 1 (1.3) | 1 (2.3) | 3 (6) | 1 (1.8) | 10 (17.8) | 1 (1.6) |
| Streptococci AG-veC | 25 (32.8) | 15 (35.7) | 15 (30) | 19 (35.8) | 11 (19.6) | 39 (63.9) |
| Campylobacter rectus FG-veR | 6 (7.8) | 4 (9.5) | 3 (6) | - | 4 (7.1) | 2 (3.2) |
| Treponemadenticola AnG-veC1 | 1 (1.3) | 2 (4.7) | 1 (2) | 1 (1.8) | - | - |
| Gemella spp FG+veC | - | - | - | - | 2 (3.2) | |
| Filifactoralocis FG+veR | 1 (1.3) | 3 (7.1) | 1 (2) | 1 (1.8) | 1 (1.7) | 2 (3.2) |
| Total (n) | 76 | 42 | 50 | 53 | 56 | 61 |
| P value | 0.595 | 0.895 | 0.0062 | |||
| Type of bacteria | Control | Test | χ2 | P value |
| Baseline | ||||
| Aerobic/facultative | 55 | 71 | 4.913 | 0.0839 |
| Anaerobic | 45 | 29 | ||
| Gram-positive | 69 | 71 | 2.391 | 0.00521 |
| Gram-negative | 31 | 29 | ||
| Cocci | 72 | 58 | 2.598 | 0.00181 |
| Rods | 28 | 42 | ||
| 5 wk | ||||
| Aerobic/facultative | 60 | 62 | 0.721 | 0.02511 |
| Anaerobic | 40 | 38 | ||
| Gram-positive | 75 | 75 | 0.593 | 0.01341 |
| Gram-negative | 25 | 25 | ||
| Cocci | 65 | 51 | 0.398 | 0.00311 |
| Rods | 35 | 45 | ||
| 13 wk | ||||
| Aerobic/facultative | 43 | 85 | 5.821 | 0.00511 |
| Anaerobic | 57 | 15 | ||
| Gram-positive | 39 | 80 | 6.321 | 0.00321 |
| Gram-negative | 61 | 20 | ||
| Cocci | 38 | 55 | 7.229 | 0.00051 |
| Rods | 72 | 35 | ||
At 5 wk, in the control samples, predominantly Streptococci (30%) and Clostridium (14%) were present, as well as aerobic/facultative gram positive cocci atmosphere. In the test group, predominantly Streptococci (35.8%) and Clostridium (11.3%) were present, as well as aerobic/facultative gram positive cocci and rods atmosphere. The P value at 5 wk was 0.895. The application of a test shows that the distribution of bacteria does not differ significantly at baseline at 5% level of significance.
At 13 wk, in control samples, predominantly Streptococci (19.6%), Veionella parvula (V. parvula) (17.8%), Prevotella intermedia (P. intermedia) (14.2%) and Fusobacterium nucleatum (F. nucleatum) (14.2%) were present, as well as anaerobic gram negative rod atmosphere. In the test group, predominantly Streptococci (63.9%), coagulase negative Staphylococci (6.5%) and Bifidobacterium (4.9%) were present, as well as aerobic/facultative gram positive cocci and rods atmosphere. The P value at thirteen weeks was 0.006. The application of a χ2 test shows that there is a significant association between the distributions of bacteria at 13 wk between control and test groups at 5% level of significance.
Table 4 shows the distribution of bacteria isolated in the control sample at baseline, 5 wk and 13 wk. There is an increase in anaerobic bacteria from 45% at baseline level to 57% at 13 wk. There is an increase in gram negative bacteria from 31% at baseline level to 61% at 13 wk. There is also an increase in rod shape bacteria from 28% at base line level to 72% at 13 wk. Table 4 shows the distribution of bacteria isolated in the test sample at baseline, 5 wk and 13 wk. There is a decrease in anaerobic bacteria from 29% at baseline level to 15% at 13 wk. There is a decrease in gram negative bacteria from 29% at baseline level to 20% at 13 wk. There is also a decrease in rod shape bacteria from 42% at base line level to 35% at 13 wk.
| Time | Bacteria (control group) | Bacteria (test group) | ||||
| Anaerobic | Gram-negative | Rod-shaped | Anaerobic | Gram-negative | Rod-shaped | |
| Baseline | 45% | 31% | 28% | 29% | 29% | 42% |
| 5 wk | 40% | 25% | 35% | 38% | 25% | 45% |
| 13 wk | 57% | 61% | 72% | 15% | 20% | 35% |
| 2 | 6.022 | 2.091 | 5.412 | 10.171 | 5.021 | 6.118 |
| P value | 0.089 | 0.0211 | 0.098 | 0.081 | 0.285 | 0.192 |
Cardinal signs of gingival inflammation are redness, edema and bleeding. Primary etiology of gingival inflammation is the presence of local irritants initiated by the presence of plaque. If plaque accumulation and growth can be limited, gingival inflammation can be controlled. Chlorhexidine is bactericidal and its role as an antibacterial agent is well established. Orug et al[22] reported an increase in antibacterial activity of CHX based Zn polycarboxylate cement.
Chlorhexidine also promotes the formation of a hybrid layer[18,19] and improves the physical properties of the resin cement. It has been found to diminish the loss of bonding effectiveness over time associated with etch-and-rinse and self-etch cements[20]. Chlorhexidine application in etch-rinse resin cement also reduced microleakage at gingival margins after storage[21].
In the present study, changes in subgingival microflora were detected following the cementation of FPDs with or without priming the tooth surface with 2% CHX. It was seen that the priming of a tooth surface with CHX significantly affected the distribution of bacteria compared with that of the control group of patients.
The bacteria cultivated from periodontally healthy sites consist predominantly of gram-positive facultative rods and cocci (approximately 75%). Small proportions of gram-negative species are also found. The most frequently found bacteria are P. intermedia, F. nucleatum, Capnocytophaga, Neisseria spp and Veillonella spp[25]. The bacteria found in chronic gingivitis comprise of roughly equal proportions of gram-positive species (56%) (predominantly Streptococcus sanguis, Streptococcus mitis, Actinomyces viscosus, Actinomyces naeslundii and Peptostreptococcus micros) and gram-negative species (44%) (predominantly F. nucleatum, P. intermedia, V. parvula, Haemophilus and Campylobacter spp), as well as facultative (59%) and anaerobic (41%) microorganisms[26].
In the present study, at 13 wk, the subgingival microflora of control sites had a significant shift towards a gram negative anaerobic rod atmosphere. It is evident as the % of Fusobacterium nucleatum increased from 2.6% at baseline to 14.2% at 13 wk. Similarly, Porphyromonas gingivalis was missing at the baseline level in the control group and was 3.2% at 13 wk in the control group. Prevotella intermedia increased from 1.3% at baseline level to 14.2% at 13 wk in the control group. Veionella parvula increased from 1.3% to 17.8% from baseline to 13 wk in the control group. In contrast to this, subgingival microflora in the test group at 13 wk had a composition that was similar to the microflora at baseline. The difference which was present at these two sample times in the test group at 13 wk was an increased percent of Coagulase negative Staphylococci from 4.7% to 6.5%, an increase in Streptococci from 35.7% to 63.9%. Neisseria was 4.7% at baseline in test group and was found to be missing at 13 wk. Gemsella was missing at baseline level and was 3.2% at 13 wk. The percent of anaerobic and gram negative bacteria decreased from 29% to 15% and 29% to 20% consecutively. Thus, it was found that in the test group, the atmosphere of aerobic/facultative gram positive cocci rod was present which indicates a healthy periodontal site, whereas in the control group, an anaerobic gram negative rod atmosphere was present which indicates an unhealthy periodontal condition. To evaluate only the effects of CHX treatment, no professional scaling, root planing or oral prophylaxis was performed after cementation of the crowns in this study.
In the present study, the tooth preparation margins were completed with a chamfer finish line and crown margins placed at the gingival margin. Many luting agents show bacteriostatic/bactericidal properties but polycarboxylate cement and resin cement does not show such properties. This study shows a favorable shift in distribution of bacteria towards gram positive facultative aerobes in the test group compared to the control group in which a shift in distribution of bacteria towards gram negative facultative anaerobes was observed.
In conclusion, this study has shown that priming the tooth surfaces with 2% CHX before luting FPDs with resin cement significantly increased inhibition of periodontally suspected bacteria. This is evident from the finding that the number of aerobic/facultative gram positive cocci rod which enhances the periodontal health increased in the test group from 1.6% at baseline to almost 4% at 13 wk. At the same time, the number of anaerobic gram negative rods which decrease periodontal health was significantly found in the control group. Thus, we can conclude that priming tooth surfaces with 2% CHX may enhance antibacterial activity of the cement and create favorable distribution of bacteria towards aerobic/facultative gram positive cocci rods atmosphere at least 13 wk post-cementation of the prostheses.
P- Reviewers: Ferreira MM, Hotta M, Kukiattrakoon B S- Editor: Gou SX L- Editor: Roemmele A E- Editor: Wang CH
| 1. | Lang NP. Periodontal considerations in prosthetic dentistry. Periodontol 2000. 1995;9:118-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Singh Y, Saini M. Designing crown contour in fixed prosthodontics: a neglected arena. Annal and Essence of clinical dentistry. 2011;3:142-147. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Eissmann HF, Radke RA, Noble WH. Physiologic design criteria for fixed dental restorations. Dent Clin North Am. 1971;15:543-568. [PubMed] |
| 4. | Skurow HM, Lytle JD. The interproximal embrasure. Dent Clin North Am. 1971;15:641-647. [PubMed] |
| 5. | Flores-de-Jacoby L, Zafiropoulos GG, Ciancio S. Effect of crown margin location on plaque and periodontal health. Int J Periodontics Restorative Dent. 1989;9:197-205. [PubMed] |
| 6. | Walton JN, Gardner FM, Agar JR. A survey of crown and fixed partial denture failures: length of service and reasons for replacement. J Prosthet Dent. 1986;56:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 172] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Holm C, Tidehag P, Tillberg A, Molin M. Longevity and quality of FPDs: a retrospective study of restorations 30, 20, and 10 years after insertion. Int J Prosthodont. 1986;16:283-289. [PubMed] |
| 8. | Libby G, Arcuri MR, LaVelle WE, Hebl L. Longevity of fixed partial dentures. J Prosthet Dent. 1997;78:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 74] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Rosenstiel SF, Land MF, Crispin BJ. Dental luting agents: A review of the current literature. J Prosthet Dent. 1998;80:280-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 256] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 10. | Myers ML, Staffanou RS, Hembree JH, Wiseman WB. Marginal leakage of contemporary cementing agents. J Prosthet Dent. 1983;50:513-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Andrews JT, Hembree JH. In vivo evaluation of marginal leakage of four inlay cements. J Prosthet Dent. 1976;35:532-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Vermeersch G, Leloup G, Delmée M, Vreven J. Antibacterial activity of glass-ionomer cements, compomers and resin composites: relationship between acidity and material setting phase. J Oral Rehabil. 2005;32:368-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Matalon S, Slutzky H, Weiss EI. Antibacterial properties of 4 orthodontic cements. Am J Orthod Dentofacial Orthop. 2005;127:56-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Imazato S. Antibacterial properties of resin composites and dentin bonding systems. Dent Mater. 2003;19:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 293] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 15. | Boeckh C, Schumacher E, Podbielski A, Haller B. Antibacterial activity of restorative dental biomaterials in vitro. Caries Res. 2002;36:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 16. | Hanes PJ, Purvis JP. Local anti-infective therapy: pharmacological agents. A systematic review. Ann Periodontol. 2003;8:79-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 145] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Stanley A, Wilson M, Newman HN. The in vitro effects of chlorhexidine on subgingival plaque bacteria. J Clin Periodontol. 1989;16:259-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Carrilho MR, Geraldeli S, Tay F, de Goes MF, Carvalho RM, Tjäderhane L, Reis AF, Hebling J, Mazzoni A, Breschi L. In vivo preservation of the hybrid layer by chlorhexidine. J Dent Res. 2007;86:529-533. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 344] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 19. | Hebling J, Pashley DH, Tjäderhane L, Tay FR. Chlorhexidine arrests subclinical degradation of dentin hybrid layers in vivo. J Dent Res. 2005;84:741-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 349] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 20. | Shafiei F, Memarpour M. Effect of chlorhexidine application on long-term shear bond strength of resin cements to dentin. J Prosthodont Res. 2010;54:153-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Shafie F, Doozandeh M, Alavi A. Effect of resin coating and chlorhexidine on microleakage of two resin cements after storage. J Dent (Tehran). 2010;7:31-40. [PubMed] |
| 22. | Orug BO, Baysallar M, Cetiner D, Kucukkaraaslan A, Dogan B, Doganci L, Akca E, Bal B. Increased antibacterial activity of zinc polycarboxylate cement by the addition of chlorhexidine gluconate in fixed prosthodontics. Int J Prosthodont. 2005;18:377-382. [PubMed] |
| 23. | Silness J, Loe H. Periodontal disease in pregnancy. II. correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4958] [Cited by in RCA: 5453] [Article Influence: 89.4] [Reference Citation Analysis (0)] |
| 24. | Loe H, Silness J. Periodontal disease in pregnancy. I. prevalence and severity. Acta Odontol Scand. 1963;21:533-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4615] [Cited by in RCA: 5039] [Article Influence: 81.3] [Reference Citation Analysis (0)] |
| 25. | Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol 2000. 2005;38:135-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 980] [Cited by in RCA: 1046] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 26. | Feng Z, Weinberg A. Role of bacteria in health and disease of periodontal tissues. Periodontol 2000. 2006;40:50-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 163] [Article Influence: 8.6] [Reference Citation Analysis (0)] |