Published online Oct 16, 2013. doi: 10.12998/wjcc.v1.i7.227
Revised: August 29, 2013
Accepted: September 3, 2013
Published online: October 16, 2013
Processing time: 146 Days and 21.7 Hours
The term “intracystic papillary ductal carcinoma in situ”, has recently changed and is now more appropriately referred to as “intracystic papillary carcinoma’’ constituting only 0.5% to 1% of all breast cancers. Herein, we discuss an unusual case of intracystic insitu papillary carcinoma of breast in a postmenopausal woman, the diagnosis of which was made on histopathology and confirmed by immunohistochemistry. Patient responded well to postoperative adjuvant radiotherapy without any recurrence, thereby preventing further morbidity and mortality related to invasion or tumor progression. So careful histopathological evaluation is the mainstay to arrive at the correct diagnosis to avoid untoward complications related to under diagnosis and /over diagnosis.
Core tip: The onco surgeon and onco pathologist should keep in mind this rare type of insitu carcinoma as a differential diagnosis in palpable breast lumps as it often mimics a benign lesion clinically. However, careful histopathological evaluation superadded by immunohistochemistry is an effective tool to arrive at the correct diagnosis to avoid untoward complications related to under diagnosis and/over diagnosis.
- Citation: Ingle SB, Hinge(Ingle) CR, Murdeshwar HG, Adgaonkar BD. Unusual case of insitu (intracystic) papillary carcinoma of breast. World J Clin Cases 2013; 1(7): 227-229
- URL: https://www.wjgnet.com/2307-8960/full/v1/i7/227.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i7.227
Intracystic papillary carcinoma (IPC) is an uncommon breast cancer constituting only 0.5% to 1% of all breast cancers[1]. Benign and malignant papillary lesions of the breast can be very difficult to distinguish on cytology[2,3]. It is said to occur more frequently among whites and postmenopausal women[2]. Papillary lesions of breast have been evaluated in a wide spectrum ranging from intraductal papilloma to insitu papillary carcinoma of breast and invasive papillary carcinoma[3,4]. Herein, we discuss an unusual case of IPC of breast in a postmenopausal woman in sharp contrast with the clinicoradiological diagnosis.
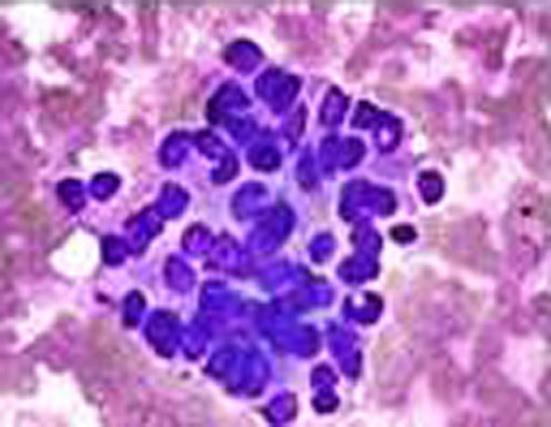
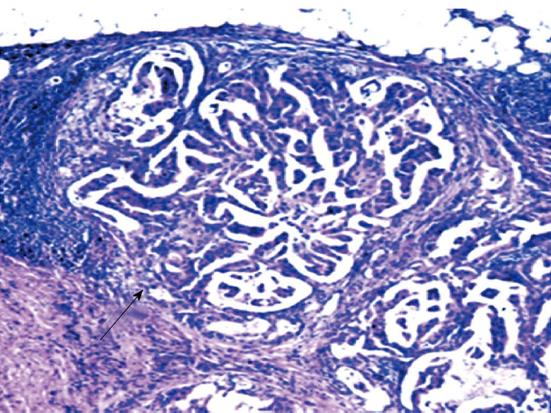
A 49-year-old female presented with a well-circumscribed swelling in the upper outer quadrant of left breast measuring 3 cm in diameter. The lump was freely mobile and not fixed to skin and deeper tissue. Mammography showed a circumscribed mass in breast with partially obscured margins. Sonography showed a cystic mass with internal echoes without posterior acoustic shadowing. All hematological parameters were within normal limits. On examination there was no palpable axillary lymphadenopathy. Fine Needle Aspiration Cytology confirmed the presence of atypical cells (Figure 1). A core biopsy of the lesion revealed atypical ductal hyperplasia, but no evidence of malignancy. In view of the atypical cells and the residual swelling, the lesion was excised. Gross examination revealed a lesion 3 cm × 2 cm × 2 cm in size. The cut surface was grey white and firm with focal areas of hemorrhages and necrosis (Figure 2). Histology showed an intracystic tumor composed of papillary, adenoid and cribriform structures lined by columnar cells exhibiting features of marked cytological atypia, i.e., nuclear hyperchromasia, pleomorphism, abnormal mitosis and increased N:C ratio (Nucleocytoplasmic ratio) with fibro vascular cores (Figure 3). The myoepithelial layer was intact. On immunohistochemical staining 3+ nuclear staining was obtained by estrogen and progesterone, whereas a negative result was obtained by cerB2. The case was finally diagnosed as insitu papillary carcinoma of breast (IPC). Left simple mastectomy with sentinel lymph-node mapping was performed. There was no evidence of tumor in the mammary tissue and the sentinel node. Adjuvant radiotherapy (40 Gy in 25 fractions) was advised due to tumor extension close to deep margin and patient is doing well since last one year without any recurrence.
The terminology applied to describe papillary breast lesions in the literature is relatively confusing. The traditional term “intracystic papillary carcinoma” generally refers to a localized in situ lesion, in a cystically dilated duct. In view of the desmoplasia often surrounding these lesions, the distinction between in situ and invasive papillary carcinoma can be very difficult to make. Therefore, IPC had been divided it into three subgroups which seem to correlate with the prognosis: IPC alone, IPC plus DCIS and IPC with invasion[5]. In this manner, the term “papillary DCIS” would refer to a more diffuse process that involves multiple ducts as opposed to a localized lesion[5].
Recently, Hill et al[6] using myoepithelial cell staining, suggested a spectrum of progression from in situ disease to invasive disease, signifying that what appears to be DCIS on histology may potentially cause distant metastases. The lack of an intact basal myoepithel cell layer can be identified by calponin, smooth-muscle myosin heavy chain cytoplasmic stains and by p63 nuclear stains. This “gold standard” method has a relatively high sensitivity and denotes the invasiveness of the tumor cells in malignant papillary breast lesions[7].
The diagnosis of IPC of the breast should be made carefully. Triple assessment is essential and the goal is to achieve a preoperative diagnosis prior to surgery. The radiological diagnosis of IPC is relatively challenging. The typical appearance of IPC on sonography is a hypo echoic area with soft tissue echoes projecting from the wall of the cyst[6,8]. However, variations exist on ultrasounds from intraductal lesions associated with ductal dilatation and a predominantly solid pattern with the intraductal or intracystic mass totally filling the duct[9]. Importantly, IPCs are vascular tumors demonstrating a characteristic flow pattern on color-flow studies, which are sensitive to identifying even very small IPCs. A distinct vascular pedicle can be identified within the central core with branching vessels arborising within the mass[9].
The mammographic appearance of IPCs is less specific. Small IPCs are often negative on mammography, while larger lesions may resemble any other focal well-circumscribed dense mass[9]. Both can cause minimal to moderate duct dilatation in a tapering band-like density pattern from the nipple towards the parenchyma. In addition, one report suggested the use of pneumocystography[10], and another MRI[11], in combination with mammography and ultrasound to diagnose IPC.
Fine Needle Aspiration Cytology and core biopsy are usually performed. However, false negative results with cytology are relatively frequent[12]. Therefore, excisional biopsy should be carried out in all cystic lesions of the breast, which are suspicious on any of the above diagnostic modalities.
There are no clear guidelines about the management of IPC, which is due to various factors. On one hand IPC is a rarity, on the other hand, the histopathological classification and detection of invasiveness in IPC is rather confusing[5]. Since the prognosis of IPC is excellent with low loco regional and distant recurrence rates, mastectomy is usually not necessary, unless it is technically unavoidable[13]. Axillary node metastasis can occur in up to 14% of the cases[13] therefore, an axillary staging procedure or clearance is recommended by most authors[9,13]. Others argue that IPC should be generally regarded as an in situ disease, therefore axillary surgery is not recommended by these authors[6,8]. There has been no clear indication for adjuvant endocrine therapy, even for patients with estrogen-receptor-positive tumors. The addition of hormonal treatment does not appear to have influenced the outcome[13]. On the contrary, Fayanju et al[14] recently reviewed the usual adjuvant treatment applied for IPC and found that patients with DCIS or micro invasive disease in association with IPC were more likely to receive radiotherapy and tamoxifen
In a conclusion, the oncosurgeon and oncopathologist should keep in mind this rare type of carcinoma as a differential diagnosis in palpable breast lumps as it often mimics a benign lesion clinically. In such a scenario triple assessment, i.e., clinical examination, radiology and histological assessment with a high level of clinical suspicion, is necessary to diagnose insitu papillary carcinoma due to its rarity.
P- Reviewers Lin JH, Shao R S- Editor Wen LL L- Editor A E- Editor Wang CH
| 1. | Solorzano CC, Middleton LP, Hunt KK, Mirza N, Meric F, Kuerer HM, Ross MI, Ames FC, Feig BW, Pollock RE. Treatment and outcome of patients with intracystic papillary carcinoma of the breast. Am J Surg. 2002;184:364-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 95] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Fisher ER, Palekar AS, Redmond C, Barton B, Fisher B. Pathologic findings from the National Surgical Adjuvant Breast Project (protocol no. 4). VI. Invasive papillary cancer. Am J Clin Pathol. 1980;73:313-322. [PubMed] |
| 3. | Reid-Nicholson MD, Tong G, Cangiarella JF, Moreira AL. Cytomorphologic features of papillary lesions of the male breast: a study of 11 cases. Cancer. 2006;108:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Dawson AE, Mulford DK. Benign versus malignant papillary neoplasms of the breast. Diagnostic clues in fine needle aspiration cytology. Acta Cytol. 1994;38:23-28. [PubMed] |
| 5. | Collins LC, Carlo VP, Hwang H, Barry TS, Gown AM, Schnitt SJ. Intracystic papillary carcinomas of the breast: a reevaluation using a panel of myoepithelial cell markers. Am J Surg Pathol. 2006;30:1002-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Hill CB, Yeh IT. Myoepithelial cell staining patterns of papillary breast lesions: from intraductal papillomas to invasive papillary carcinomas. Am J Clin Pathol. 2005;123:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Sinha S, Hughes RG, Ryley NG. Papillary carcinoma in a male breast cyst: a diagnostic challenge. Ann R Coll Surg Engl. 2006;88:W3-W5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Andrés B, Aguilar J, Torroba A, Martínez-Gálvez M, Aguayo JL. Intracystic papillary carcinoma in the male breast. Breast J. 2003;9:249-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Blaumeiser B, Tjalma WA, Verslegers I, De Schepper AM, Buytaert P. Invasive papillary carcinoma of the male breast. Eur Radiol. 2002;12:2207-2210. [PubMed] |
| 10. | Kinoshita T, Fukutomi T, Iwamoto E, Takasugi M, Akashi-Tanaka S, Hasegawa T. Intracystic papillary carcinoma of the breast in a male patient diagnosed by core needle biopsy: a case report. Breast. 2005;14:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Ganesan S, Karthik G, Joshi M, Damodaran V. Ultrasound spectrum in intraductal papillary neoplasms of breast. Br J Radiol. 2006;79:843-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Levine PH, Waisman J, Yang GC. Aspiration cytology of cystic carcinoma of the breast. Diagn Cytopathol. 2003;28:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Grabowski J, Salzstein SL, Sadler GR, Blair S. Intracystic papillary carcinoma: a review of 917 cases. Cancer. 2008;113:916-920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Fayanju OM, Ritter J, Gillanders WE, Eberlein TJ, Dietz JR, Aft R, Margenthaler JA. Therapeutic management of intracystic papillary carcinoma of the breast: the roles of radiation and endocrine therapy. Am J Surg. 2007;194:497-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |