Published online Aug 16, 2013. doi: 10.12998/wjcc.v1.i5.159
Revised: July 3, 2013
Accepted: July 17, 2013
Published online: August 16, 2013
Processing time: 85 Days and 12.9 Hours
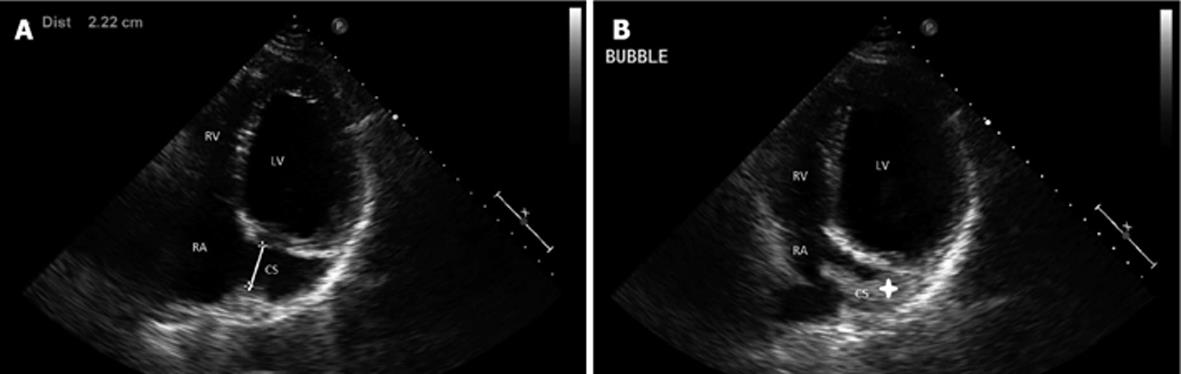
Persistent left superior vena cava, usually an incidental finding, is the most common thoracic vein anatomical variation draining into the coronary sinus. Central venous catheter procedures may be complicated secondary to the presence of a persistent left superior vena cava, leading to life-threatening complications such as arrhythmias, cardiogenic shock, and cardiac arrest. We present a case of persistent superior vena cava diagnosed on transthoracic echocardiogram (TTE) in a patient with congestive heart failure. A dilated coronary sinus was identified on TTE, followed by injection of agitated saline into the left antecubital vein resulting in filling of the coronary sinus prior to the right atrium-an indication of persistent left superior vena-cava. This also was confirmed on cardiac computed tomography. Such a diagnosis is critical in patients who may undergo central venous catheter procedures such as our patient’s potential requirement for an implantable cardiovertor defibrillator due to severe global left ventricular systolic dysfunction. The presence of a persistent left superior vena cava should always be suspected when the guidewire takes a left-sided downward course towards the right atrium at the level of the coronary sinus. Therefore, special attention should be paid to the imaging work-up prior to central venous catheter procedures.
Core tip: Although the diagnosis of persistent left superior vena cava (LSVC) does not make a pacemaker or implantable cardiovertor-defibrillator placement impossible, it does pose significant challenges and complications during the procedure. Accordingly, when patients are being considered for such central venous catheter devices, special attention should be paid to the imaging work-up prior to implantation to identify persistent LSVC if present.
- Citation: Siddiqui AM, Cao LB, Movahed A. Side matters: An intriguing case of persistent left superior vena-cava. World J Clin Cases 2013; 1(5): 159-161
- URL: https://www.wjgnet.com/2307-8960/full/v1/i5/159.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i5.159
Persistent left superior vena cava (LSVC) was first described by Edwards et al[1]. This is the most common thoracic vein anatomical variation with a prevalence of 0.3% in the general population[2]. The persistent LSVC drains into right atrium (RA) via the coronary sinus (CS). This is caused by failure in the degeneration of the left cardinal vein[1]. Central venous catheter based procedures, such as a right heart catheterization, implantable cardiovertor-defibrillator (ICD) implantation, and electrophysiological procedures, may become complicated by technical difficulties to access the right ventricle secondary to the presence of such an anomaly. Persistent LSVC is usually an incidental finding or recognized when a left cephalic or subclavian approach is used for the procedures mentioned above.
A 68 year-old Hispanic male with a past medical history of hypertension was referred to the cardiology clinic with shortness of breath, paroxysmal nocturnal dyspnea, lower extremity edema, but no associated chest pain or syncopal episodes. His cardiac risk factors include hypertension and class I obesity with a body mass index of 31 kg/m2. He was only taking hydrochlorothiazide 25 mg po daily. Twelve-lead electrocardiogram revealed frequent pre-mature ventricular contractions, otherwise unremarkable. Pertinent labs include a brain natriuretic peptide level of 46.8. No cardiac biomarkers were drawn. Transthoracic echocardiogram (TTE) revealed dilated left ventricle with a diminished left ventricular ejection fraction (LVEF) of 30% visually. By Modified Simpson’s method, an LVEF of 23% was calculated. In the parasternal long axis view, the interventricular septal diameter was 0.967 cm, the left ventricular posterior wall diameter (LVPwd) was 0.919 cm, the left ventricular end diastolic diameter was 6.29 cm, and the left ventricular mass index was greater than 138 g/m2. There was eccentric hypertrophy by relative wall thickness calculation. Grade 1 diastolic dysfunction was observed with E:A reversal, lateral e’ of 6.3 and medial e’ of 4.8. The left atrial size and volume was in the upper limits of normal. There was normal pulmonary vein flow. Tricuspid annular plane systolic excursion was 2.1 cm/s. No reliable right ventricular dimensions were obtained. Additionally, the CS was dilated at 22 mm (Figure 1A). During injection of agitated saline into the left antecubital vein, it was found that opacification in the CS occurred prior to that in the RA (Figure 1B), contrary to what would normally be expected in such a study. This finding led to the diagnosis of a persistent LSVC. He was additionally noted to have a dilated ascending aorta of 4.3 cm. The aortic root measured 4.1 cm at the sinotubular junction. For further evaluation, the patient underwent a cardiac computed tomography angiography (CCTA) revealing no significant coronary artery disease. The patient’s coronary CCTA further demonstrated a persistent LSVC (Figure 2). The patient was started on appropriate medical therapy of bisoprolol fumarate 2.5 mg and lisinopril for non-ischemic dilated cardiomyopathy upon discharge. He has responded well to these therapies (currently New York Heart Association class I) and is due for a follow-up to evaluate his left ventricular function and potential for ICD placement.
Multiple imaging modalities can be used to diagnose persistent LSVC including TTE, transesophageal echocardiography, computed tomography, and magnetic resonance imaging[3]. Our case illustrates how a persistent LSVC was diagnosed on a routine TTE. Although this patient had systolic dysfunction, he did not have chest pain or a history of unstable angina, with normal B-type natriuretic peptide on presentation, and thus, we elected for CCTA vs a cardiac catheterization to further evaluate his aortic aneurysm, but to also rule out significant coronary artery disease as CCTA’s negative predictive value of assessing coronary artery disease is high. In 2001, 1.73 million coronary angiograms were performed for diagnostic purposes only. Because coronary angiography is associated with a small but not negligible risk of complications (inherent in invasive procedures), inconvenience to patients, and significant costs, coronary CTA may be an attractive alternative to invasive selective coronary angiography, with the potential to reduce the number of purely diagnostic angiograms. Patients with an intermediate likelihood of CAD (between 30% and 70% probability of having significant CAD, as determined by age, sex, and quality of chest pain) may benefit from coronary CTA. According to “2013 ACCF/ACR/ASE/ASNC/SCCT/SCMR Appropriate Utilization of Cardiovascular Imaging in Heart Failure” by Patel et al[4], cardiac catheterization utilization is rarely appropriate in intermediate to low risk patients. Nonetheless, the importance of diagnosing a persistent LSVC can be realized when considering the complications of misplacing a central venous catheter or catheters for electrophysiological procedures that can result in complications such as angina, arrhythmia, cardiogenic shock, and cardiac arrest[5]. It is imperative to consider the presence of persistent LSVC during a central venous catheter implantation when the guide wire takes a left-sided downward course towards the right atrium at the level of the coronary sinus[6]. Although the diagnosis of persistent LSVC does not make a pacemaker or ICD placement impossible, it does pose significant challenges and complications during the procedure. Accordingly, when patients are being considered for such central venous catheter devices, special attention should be paid to the imaging work-up prior to implantation to identify persistent LSVC if present.
P- Reviewers Ciccone MMM, Fusai G S- Editor Gou SX L- Editor A E- Editor Lu YJ
| 1. | Edwards JE, Dushane JW, Alcottd L, Burchell HB. Thoracic venous anomalies. III. Atresia of the common pulmonary vein, the pulmonary veins draining wholly into the superior vena cava. AMA Arch Pathol. 1951;51:446-460. [PubMed] |
| 2. | Biffi M, Boriani G, Frabetti L, Bronzetti G, Branzi A. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter-defibrillator implantation: a 10-year experience. Chest. 2001;120:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Ratliff HL, Yousufuddin M, Lieving WR, Watson BE, Malas A, Rosencrance G, McCowan RJ. Persistent left superior vena cava: case reports and clinical implications. Int J Cardiol. 2006;113:242-246. [PubMed] |
| 4. | Patel MR, White RD, Abbara S, Bluemke DA, Herfkens RJ, Picard M, Shaw LJ, Silver M, Stillman AE, Udelson J. 2013 ACCF/ACR/ASE/ASNC/SCCT/SCMR appropriate utilization of cardiovascular imaging in heart failure: a joint report of the American College of Radiology Appropriateness Criteria Committee and the American College of Cardiology Foundation Appropriate Use Criteria Task Force. J Am Coll Cardiol. 2013;61:2207-2231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 151] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 5. | Fraser RS, Dvorkin J, Rossall RE, Eidem R. Left superior vena cava: a review of associated congenital heart lesions, catheterization data and roentgenologic findings. Am J Med. 1961;31:711-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 131] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Paraskevaidis S, Konstantinou DM, Theofilogiannakos E, Mantziari L, Tachmatzidis D, Kolettas V, Hadjimiltiades S, Styliadis I. Persistent left superior vena cava : Report of 3 patients undergoing device implantation. Herz. 2013;Apr 6; [Epub ahead of print]. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |