Published online Jun 16, 2013. doi: 10.12998/wjcc.v1.i3.108
Revised: April 24, 2013
Accepted: May 9, 2013
Published online: June 16, 2013
Processing time: 142 Days and 23.5 Hours
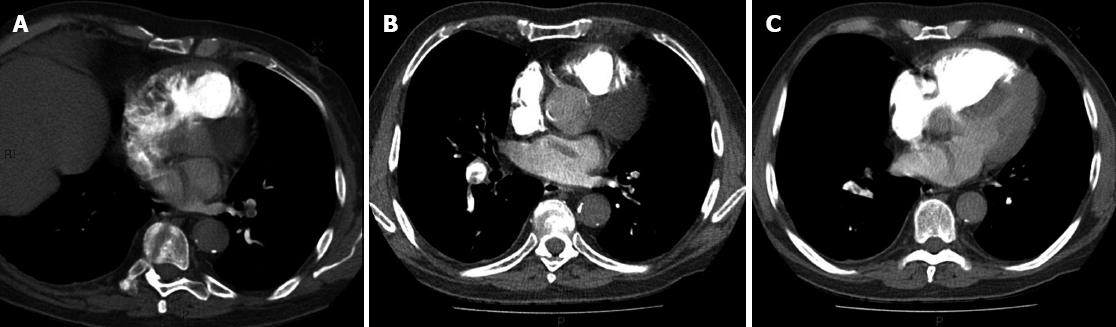
An elderly gentleman presented to the emergency department with a recent history of dyspnoea, collapse and transient neurological symptoms. He was noted to be hypoxic with a significantly elevated D Dimer. A computer tomography pulmonary angiogram demonstrated a large embolus with a further filling defects within the left and the right atria, abutting the inter-atrial septum. Suspicion of a paradoxical pulmonary embolus was raised and the patient subsequently underwent echocardiography which confirmed a patent foramen ovale (PFO). He was commenced on warfarin therapy. In patients with elevated right heart pressure, a PFO can be unmasked and give rise to cerebral emboli. Clinical suspicion should be raised in patients with pulmonary emboli or deep venous thrombosis if there is a concomitant history of focal neurological symptoms.
Core tip: Patent foramen ovale (PFO) are common but usually closed and asymptomatic due to the greater pressure in the left heart. They however pose a particular risk for patients with large pulmonary emboli (PE) where they can open providing a right to left shunt when the right heart pressure rises due to pulmonary arterial obstruction by PE. In these circumstances thrombus can transit the PFO paradoxically embolising systemically. We report a case of a patient with a large PE who had a cerebral embolus where thombus is imaged straddling the PFO at computer tomography pulmonary angiography.
- Citation: Cormack L, Murchison JT. Paradoxical embolus straddling patent foramen ovale demonstrated by computed tomographic pulmonary angiography. World J Clin Cases 2013; 1(3): 108-110
- URL: https://www.wjgnet.com/2307-8960/full/v1/i3/108.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i3.108
Patent foramen ovale (PFO) is estimated to be present in approximately 27% of the population[1]. Under normal physiological conditions where left-sided heart pressure exceeds right-sided pressure, the foramen remains closed. However, in circumstances where right-sided pressure is elevated, for example in pregnancy, cor pulmonale or in the presence of pulmonary thromboembolic disease, the foramen can be opened which may result in paradoxical emboli entering the left-heart and systemic circulation. The presence of thrombo-embolic disease and a PFO thus increases the risk of stroke.
This case highlights the value of computer tomography (CT) pulmonary angiogram, for example when compared to perfusion scanning, in assessing right heart strain as a result of pulmonary embolus, in addition to the possibility of detecting paradoxical embolus when present.
An 80-year-old gentleman with history of type 2 diabetes, chronic renal impairment and hypertension presented to the emergency department with marked dyspnoea, dizziness and collapse but without loss of consciousness. There were no features to suggest underlying infection. He also described transient left-sided paraesthesia and weakness, which had largely resolved by the time he was assessed. He was noted to be hypoxic and tachycardic with a markedly raised D Dimer (34704 μg/L). CT pulmonary angiography was requested which confirmed the presence of large pulmonary emboli, but also a further filling defects within the left and right atria (see investigations below). Bubble contrast echocardiography confirmed the presence of a PFO.
CT pulmonary angiogram: Large bilateral pulmonary artery emboli with a further serpiginous filling defect visible within the left atrium, abutting the inter-atrial septum and extending into the left atrium. Appearances represent a paradoxical embolus caught in a PFO (Figure 1).
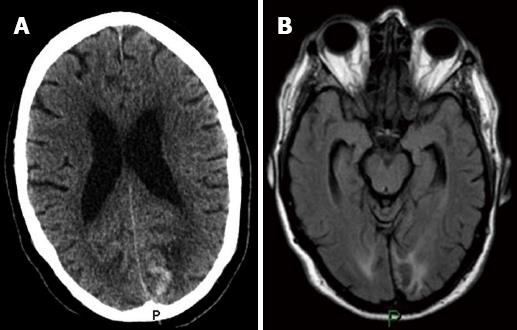
Unenhanced CT brain examination (performed the day after computed tomographic pulmonary angiography): High attenuation within the medial aspect of the left occipital lobe, in keeping with acute haemorrhage due to haemorrhagic transformation of an infarct/embolic infarct (Figure 2A).
Magnetic resonance imaging brain examination, without contrast: Performed 19 d after CT brain examination to rule out multiple emboli to the brain in order to help decide whether to surgically close the PFO. This showed bilateral occipital increased FLAIR signal with restricted diffusion in keeping with infarction. High T1 signal in the left occipital lobe consistent with a degree of haemorrhagic transformation (Figure 2B).
Echocardiography: With bubble contrast, confirmed the presence of a PFO.
The patient was commenced on warfarin therapy to treat pulmonary embolus. He was not considered for surgical closure of the PFO.
The patient made a good recovery initially. A follow-up CT brain performed because of a fall and head injury sustained at home eighteen months following initial presentation did not show any further ischaemic events.
Previous case reports of paradoxical pulmonary emboli have been able to demonstrate thrombus within a patent septal defect on echocardiography[2,3], however this finding has not been previously reported on CT pulmonary angiography. Further cases have shown a PFO only (without thrombus)[4], or have failed to demonstrate the source of the right-to-left shunt[5].
CT pulmonary angiography is the gold standard for detecting acute pulmonary embolus[6]. It has a high sensitivity (83%-100%) and specificity (89%-97%)[7,8]. An additional advantage of computed tomographic pulmonary angiography is the assessment of right ventricular/left ventricular (RV/LV) ratio as an indicator of severity in acute pulmonary embolism. Transverse RV/LV diameter ratio has been shown to be significantly higher in patients who die in hospital than amongst those who survive acute pulmonary embolus[9].
Visualisation of thrombus within the atria or ventricles is an unusual finding which should prompt further investigation of a septal defect and right-to-left shunt. Whilst the clinical history alone in this particular case may have been sufficient to provoke investigation of a PFO, the finding of thrombus within the left atrium made the presence of a PFO almost certain and may therefore have expedited echocardiography and neuro-imaging.
According to National Institute for Clinical Excellence guidelines, the optimal treatment of patients with a PFO who have had a thromboembolic event remains undefined[10]. Medical management with antiplatelet or anticoagulation therapy is frequently used to reduce the risk of further paradoxical thrombi. Closure of the PFO may be performed in patients who have further embolic events despite medical management, or in cases where anticoagulant therapy in contraindicated. Percutaneous procedures allow closure of the PFO without the need for major surgery. In this case the presence of acute haemorrhage, presumed to be haemorrhagic transformation of an embolic infarct, further complicated management, however the decision was made that it was in the patient’s best interest to proceed with anticoagulation.
P- Reviewers Kucuker A, Lovric Z, Sarica FB S- Editor Zhai HH L- Editor A E- Editor Ma S
| 1. | Hagen PT, Scholz DG, Edwards WD. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1669] [Cited by in RCA: 1576] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 2. | Ozgul U, Golbasi Z, Gulel O, Yildirim N. Paradoxical and pulmonary embolism due to a thrombus entrapped in a patent foramen ovale. Tex Heart Inst J. 2006;33:78-80. [PubMed] |
| 3. | Choong CK, Calvert PA, Falter F, Mathur R, Appleton D, Wells FC, Schofield PM, Crawford R. Life-threatening impending paradoxical embolus caught “red-handed”: successful management by multidisciplinary team approach. J Thorac Cardiovasc Surg. 2008;136:527-528.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Guo S, Roberts I, Missri J. Paradoxical embolism, deep vein thrombosis, pulmonary embolism in a patient with patent foramen ovale: a case report. J Med Case Rep. 2007;1:104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Narimatsu E, Kawamata M, Hase M, Kurimoto Y, Asai Y, Namiki A. Severe paradoxical intracranial embolism and pulmonary emboli during hip hemiarthroplasty. Br J Anaesth. 2003;91:911-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Available from: http://www.sign.ac.uk/pdf/sign122.pdf. |
| 7. | Hogg K, Brown G, Dunning J, Wright J, Carley S, Foex B, Mackway-Jones K. Diagnosis of pulmonary embolism with CT pulmonary angiography: a systematic review. Emerg Med J. 2006;23:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 38] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Moores LK, Jackson WL, Shorr AF, Jackson JL. Meta-analysis: outcomes in patients with suspected pulmonary embolism managed with computed tomographic pulmonary angiography. Ann Intern Med. 2004;141:866-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Ghaye B, Ghuysen A, Willems V, Lambermont B, Gerard P, D’Orio V, Gevenois PA, Dondelinger RF. Severe pulmonary embolism: pulmonary artery clot load scores and cardiovascular parameters as predictors of mortality. Radiology. 2006;239:884-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 182] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 10. | NICE Guidelines. Interventional procedure overview of percutaneous closure of patent foramen ovale for the secondary prevention of recurrent paradoxical embolism. Available from: http://www.nice.org.uk/nicemedia/live/11140/49940/49940.pdf. |