Published online May 16, 2013. doi: 10.12998/wjcc.v1.i2.92
Revised: April 10, 2013
Accepted: April 27, 2013
Published online: May 16, 2013
Processing time: 130 Days and 22.4 Hours
Squamous papillomas (SPs) are common benign neoplastic lesions, usually affecting the skin, oral mucosa, upper aerodigestive tract and genital organs. However, SPs of the external auditory canal (EAC) are rarely reported in the English literature. In this report, we present a 19-year-old female with left EAC SP. The etiology, natural course, diagnosis and management of this disease are discussed, with a brief review of the literature.
Core tip: Squamous papillomas (SPs) are common benign neoplastic lesions. However, SPs of the external auditory canal (EAC) are rarely reported in the English literature. A case of EAC SPs is presented here with a discussion and brief review of the literature.
- Citation: Chang NC, Chien CY, Wu CC, Chai CY. Squamous papilloma in the external auditory canal: A common lesion in an uncommon site. World J Clin Cases 2013; 1(2): 92-95
- URL: https://www.wjgnet.com/2307-8960/full/v1/i2/92.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i2.92
Squamous papillomas (SPs) are benign neoplastic lesions usually affecting the skin, oral mucosa, upper aerodigestive tract and genital organs. It is believed that the human papilloma virus (HPV) is an etiological factor of papillomas; thus, they are also called viral warts. Cutaneous SPs are a very common skin condition; however, SPs of the external auditory canal (EAC) are rarely reported in the English literature although they commonly occur in the southern Chinese population. This indicates that SPs of EAC might be an ethnically specific disease. There are several cutaneous neoplastic lesions similar to SPs in appearance. The definitive diagnosis of SPs relies on histopathological examination. Here, we present a clinical case and briefly review the literature concerning the etiology, natural course, diagnosis and management of EAC papillomas.
The presented case is a 19-year-old young Taiwanese female who visited our office with a history of left external ear canal blockage for several months. Surgical intervention for bilateral external ear canal tumors had been performed in another institute about 2 mo previously. Unfortunately, not long after the surgical procedure, left ear auditory canal fullness recurred and she visited our clinic for evaluation and management. She did not bring the report of the pathological examinations in the previous institute when she came to our office and merely described that they were benign lesions, as related by the previous surgeon.
Under otoscopic examination, an irregular, granular, mulberry-like neoplastic lesion was found, located at the cartilaginous part of the left EAC (Figure 1), and non-specific findings were noted in the contralateral ear. A surgical removal with ordinary instruments under microscope was arranged and performed.
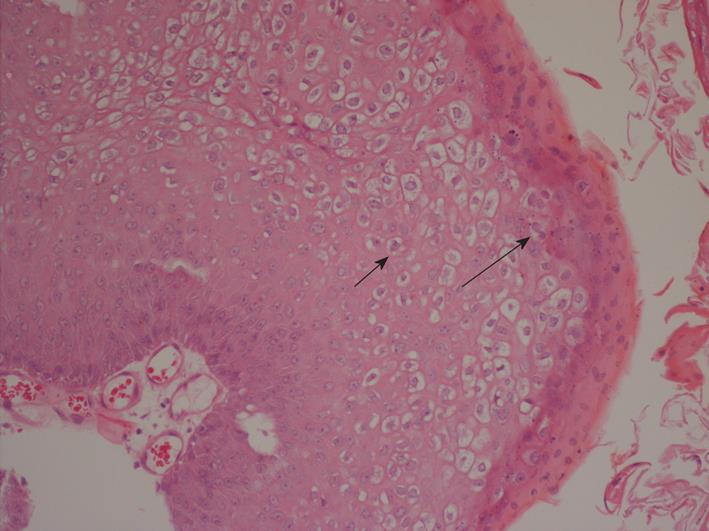
The histopathological examination showed hyperkeratosis, papillomatosis, parakeratosis, acanthosis, koilocytosis and inflammatory infiltrates in the upper dermis, characteristic features of SPs (Figure 2). The wound healed well without specific complications during the post-operative follow-up (Figure 3).
SPs are very common skin lesions. There is a high prevalence of SPs in the EAC. Papillomas, accounting for up to 78.9% of benign ear tumors, have been reported, with 95.2% of ear papillomas located in the EAC[1]. However, SPs of the external ear have been reported infrequently in the English literature, although they occur commonly in the southern Chinese population. This is probably secondary to the cultural ritual of mechanical cleansing with unsterilized re-used instruments by which infectious agent inoculation may take place[1-3]. Surgical procedures of the ear may also be a route for the dissemination of SP[4]. It is generally assumed that SPs are caused by HPV infections and SP is considered to be a viral wart[5]. Cutaneous SPs are caused most frequently by HPV types 1, 2, 3, 4, 27 and 57[6,7]. However, HPV types 6 and 11 were found to be the main causative agents for SPs of the EAC[1,8]. HPV types 6 and 11 are the most common pathogens for oral papillomas, recurrent respiratory papillomatosis and anogenital warts[7]. Like the disseminations of HPV types 6 and 11 in the aerodigestive tract and genital papillomas, vertical infection of HPV from the mother at delivery might be the primary route of the virus acquisition. The hair follicles have been suggested as possible reservoirs[7]. SPs are rare in children younger than 5 years of age; however, EAC SP in a 3-year-old patient has been reported[9].
EAC SP is a benign lesion which is generally solitary and has a low risk of bony destruction. It grows slowly and may cause a mechanical obstruction of the EAC, leading to pressure necrosis of the adjacent bone or conductive hearing impairments[10]. Involvement of the tympanic membrane is seldom reported[3,4]. Viral warts of the skin are not harmful and usually go away without any treatment[6]; however, the possibility of spontaneous resolution of EAC SPs is still unclear. The common causative HPV types are quite different in skin warts (types 1, 2, 3, 4, 27 and 57) from that in EAC SPs (types 6 and 11); the behaviors may be different with distinct HPV types. Although EAC SPs are generally believed to be mainly caused by the “low-risk” HPV types 6 and 11, malignant transformation has been reported[11].
Most neoplastic lesions of the EAC are benign and up to 80% of these lesions are papillomas[1]. Grossly, SPs commonly appear as a round or oval, flat papule with a broad base on the skin or mucous membranes. Histologically, they arise from stratified squamous epithelium and are characterized by the growth of multiple papillary fronds (papillomatosis), hyperkeratosis, parakeratosis, acanthosis, infrequent mitosis and rare nuclear atypia[1,11]. Squamous cells with clear cytoplasm, dense dark nuclei and occasionally bi-nuclei are called koilocytic cells, which indicate an infection of the cells by HPV[8].
Inverted papilloma (IP) in the EAC is similar to SP in gross appearance. However, IP has a distinct behavior from SP and should be carefully differentially diagnosed. IP, or Schneiderian papilloma inverted type, is an aggressive benign neoplastic lesion with a tendency for local recurrence and association with carcinoma. Microscopically, IP is characterized by the digitiform proliferation of squamous epithelium into the underlying connective tissue stroma[12]. HPV types 6, 11, 16 and 18 are the most common causative agents associated with IP and types 16 and 18 are more commonly associated with malignancy[9,12,13].
Surgical removal of the lesion remains the most effective method in the treatment of EAC SPs. Several methods, including cryosurgery, electrodesiccation with/without curettage and carbon dioxide laser, have been described and are believed to be effective[5]. The major complication of surgical treatment is possible scarring and subsequent stenosis of the EAC. Insertion of a silastic tube in the canal as a stent and meticulous postoperative care to prevent wound infection may provide uncomplicated healing[9].
Some agents are reported to be effective in topical treatments for viral warts. Salicylic acid and cryotherapy have shown significant effects in the clearance of cutaneous warts, especially in the hand and foot areas. Dinitrochlorobenzene, 5-fluorouracil, intralesional bleomycin, intralesional interferon, photodynamic therapy and intralesional antigen have been tried in previous studies but without much evidence for their effectiveness[6]. The effects of the above topical treatments for SPs in the EAC are not clear; hence, topical methods are not recommended as primary management for EAC SPs.
Radiotherapy for SPs in the EAC was tried in an earlier report[3]. The authors reported an excellent result for the treatment of recurrent SP in the EAC, middle ear and the mastoid cavity by radiotherapy. However, radiotherapy carries potential risks for malignant transformation of the cells and other complications, such as hearing impairment, EAC stenosis and vestibular, trigeminal and facial nerve neuropathies[14,15], so it is not recommended as the primary treatment method.
There are HPV vaccinations to prevent anogenital warts and cancers[16]. These vaccines mainly protect against HPV types 6, 11, 16 and 18, the major types causing cervical cancer, anogenital wart/cancer, recurrent respiratory papillomatosis and EAC SP. These vaccines have been approved for use of prevention of genital cancers by the United States Food and Drug Administration since 2006[16,17]. The vaccines are not indicated to prevent cutaneous and oral mucosal SPs; however, along with increasing HPV vaccination rates, the decrease of SP prevalence would be expected.
SP in the EAC is a common benign neoplastic lesion located in an uncommonly reported site. It may be caused by the infection of HPV. Surgical removal remains the treatment of choice for EAC SPs.
P- Reviewer Chandra R S- Editor Zhai HH L- Editor Roemmele A E- Editor Zheng XM
| 1. | Xia MY, Zhu WY, Lu JY, Lu Q, Chen L. Ultrastructure and human papillomavirus DNA in papillomatosis of external auditory canal. Int J Dermatol. 1996;35:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Myer CM, Woodruff SM. Pathologic quiz case 2. Squamous papilloma of the external auditory canal. Arch Otolaryngol. 1983;109:200-201, 203. [PubMed] |
| 3. | Rogers KA, Snow JB. Squamous cell papilloma of the external auditory canal and middle ear treated with radiation therapy. Laryngoscope. 1968;78:2183-2188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Welsh RL, Gluckman JL. Dissemination of squamous papilloma by surgical manipulation: a case report. Laryngoscope. 1984;94:1568-1570. [PubMed] |
| 5. | Blair RL, Irani BS, Low C. Aural papillomatosis--treatment with the carbon dioxide laser. J Laryngol Otol. 1998;112:565-566. [PubMed] |
| 6. | Kwok CS, Gibbs S, Bennett C, Holland R, Abbott R. Topical treatments for cutaneous warts. Cochrane Database Syst Rev. 2012;9:CD001781. [PubMed] |
| 7. | Syrjänen S. Current concepts on human papillomavirus infections in children. APMIS. 2010;118:494-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Wang S, Yee H, Wen HY, Wang BY. Papillomas of the external ear canal: report of ten cases in Chinese patients with HPV in situ hybridization. Head Neck Pathol. 2009;3:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Yadav SP, Chanda R, Goyal N, Chanda S. Aural papillomatosis in a 3-year-old child. Int J Pediatr Otorhinolaryngol. 2002;66:185-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Kim J, Lee DH, Cho KJ, Lee SY. Huge verruca vulgaris (wart) of the external auditory canal. Otolaryngol Head Neck Surg. 2008;139:865-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Miah MS, Crawford M, White SJ, Hussain SS. Malignant transformation from benign papillomatosis of the external auditory canal. Otol Neurotol. 2012;33:643-647. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Wood JW, Casiano RR. Inverted papillomas and benign nonneoplastic lesions of the nasal cavity. Am J Rhinol Allergy. 2012;26:157-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Shen J, Baik F, Mafee MF, Peterson M, Nguyen QT. Inverting papilloma of the temporal bone: case report and meta-analysis of risk factors. Otol Neurotol. 2011;32:1124-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Smouha EE, Karmody CS. Non-osteitic complications of therapeutic radiation to the temporal bone. Am J Otol. 1995;16:83-87. [PubMed] |
| 15. | Likhterov I, Allbright RM, Selesnick SH. LINAC radiosurgery and radiotherapy treatment of acoustic neuromas. Otolaryngol Clin North Am. 2007;40:541-570, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | D'Souza G, Dempsey A. The role of HPV in head and neck cancer and review of the HPV vaccine. Prev Med. 2011;53 Suppl 1:S5-S11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 183] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 17. | Brotherton JM, Gertig DM. Primary prophylactic human papillomavirus vaccination programs: future perspective on global impact. Expert Rev Anti Infect Ther. 2011;9:627-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |