Published online Apr 16, 2013. doi: 10.12998/wjcc.v1.i1.19
Revised: February 12, 2013
Accepted: March 21, 2013
Published online: April 16, 2013
Processing time: 110 Days and 15 Hours
AIM: To evaluate the efficacy and safety of endoscopic balloon dilation (EBD) performed for common bile duct (CBD) stones.
METHODS: From a computer database, we retrospectively analyzed the data relating to EBD performed in patients at the gastrointestinal unit of the Sandro Pertini Hospital of Rome (small center with low case volume) who underwent endoscopic retrograde cholangiopancreatography (ERCP) for CBD from January 1, 2010 to February 29, 2012. All patients had a proven diagnosis of CBD stones studied with echography, RMN-cholangiography and, when necessary, with computed tomography of the abdomen (for example, in cases with pace-makers). Prophylactic therapies, with gabexate mesilate 24 h before the procedure and with an antibiotic (ceftriaxone 2 g) 1 h before, were administered in all patients. The duodenum was intubated with a side-viewing endoscope under deep sedation with intravenous midazolam and propofol. The patients were placed in the supine position in almost all cases. EBD of the ampulla was performed under endoscopic and fluoroscopic guidance with a balloon through the scope (Hercules, wireguided balloon®, Cook Ireland Ltd. and CRE®, Microvasive, Boston Scientific Co., Natick, MA, United States).
RESULTS: A total of 14 patients (9 female, 5 male; mean age of 73 years; range 57-82 years) were enrolled in the study, in whom a total of 15 EBDs were performed. All patients underwent minor endoscopic sphincterotomy (ES) prior to the EBD. The size of balloon insufflation depended on stone size and CBD dilation and this was performed until it reached 16 mm in diameter. EBD was performed under endoscopic and fluoroscopic guidance. The balloon was gradually filled with diluted contrast agent and was maintained inflated in position for 45 to 60 s before deflation and removal. The need for precutting the major papilla was 21.4%. In one patient (an 81-year-old), EBD was performed in a Billroth II. Periampullary diverticula were found only in a 74-year-old female. The adverse event related to the procedures (ERCP + ES) was only an intra procedural bleeding (6.6%) that occurred after ES and was treated immediately with adrenaline sclerotherapy. No postoperative complications were reported.
CONCLUSION: With the current endoscopic techniques, very few patients with choledocholithiasis require surgery. EBD is an efficacious and safe procedure.
Core tip: Choledocholithiasis is frequently found in the adult population. Endoscopic sphincterotomy (ES) is considered the standard therapy for the treatment of this condition. However, several complications are associated with ES. Endoscopic balloon dilation (EBD) is actually recognized as an alternative to ES for the extraction of difficult bile duct stones. Reading the literature, we have found that most of the studies use small diameter balloons (6-10 mm), while the ones using larger balloons (from 12-20 mm) are rare. The aim of this retrospective study was to evaluate the efficacy and safety of large EBD performed for common bile duct difficult stones.
- Citation: Zippi M, De Felici I, Pica R, Traversa G, Occhigrossi G. Endoscopic papillary balloon dilation for difficult common bile duct stones: Our experience. World J Clin Cases 2013; 1(1): 19-24
- URL: https://www.wjgnet.com/2307-8960/full/v1/i1/19.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i1.19
Choledocholithiasis is found in about 10%-15% of the adult population[1]. Since 1974, when Classen et al[2] and Kawai et al[3] introduced the endoscopic sphincterotomy (ES), this procedure has become the standard therapy for the treatment of various biliary diseases, especially common bile duct (CBD) stones. Several complications associated with ES have been reported: early ones, such as acute pancreatitis, hemorrhage, duodenal perforation, acute cholangitis, and late ones, such as recurrence of stones and papillary stenosis[4]. Balloon dilation of the biliary sphincter has been introduced as an alternative to sphincterotomy for the extraction of bile duct stones[5,6]. Endoscopic balloon dilation (EBD) was first described by Staritz et al[7] in 1983. EBD is still not widely embraced, especially due to the fear of complications, in particular acute pancreatitis. However, EBD does not have the short term complications of bleeding and perforation and it may preserve the biliary sphincter, with a decrease in long term complications. There are several controversies regarding EBD, such as the difficulty of removing larger stones because of the smaller biliary opening, the more frequent need for mechanical lithotripsy (ML) and the higher incidence of pancreatitis after the procedure compared with ES[8,9]. Most of the studies used small diameter balloons (6-10 mm). Studies using larger balloon (esophageal/pyloric/colonic dilatation balloons, from 12-20 mm) are rare[10,11]. In particular, EBD is performed for large stones (a stone measured more than 2 cm), hard stones (a stone difficult to be crushed by ML or to remove after papillary balloon dilation) and for confluence stones (multiple stones or stones located at the hepatocholedochal junction).
The aim of this retrospective study was to evaluate the efficacy and safety of EBD performed for CBD difficult stones.
Starting from a computer database, we retrospectively analyzed the data relating to EBD performed in patients at the gastrointestinal unit of the Sandro Pertini Hospital of Rome (small center with low case volume) who underwent endoscopic retrograde cholangiopancreatography (ERCP) for CBD from January 1, 2010 to February 29, 2012. All patients had a proven diagnosis of CBD stones studied with echography, RMN-cholangiography and, when necessary, with computed tomography of the abdomen (for example, in cases of pace-makers).
Prophylactic therapies, with gabexate mesilate 24 h before the procedure and with an antibiotic (ceftriaxone 2 g) 1 h before, were administered in all patients.
The duodenum was intubated with a side-viewing endoscope (TJF 140 or 145®, Olympus Optical, Hamburg, Germany) under deep sedation with intravenous midazolam and propofol. The patients were placed in the supine position in almost all cases. During the ERCP, the arterial oxygen saturation, pulse rate and blood pressure were continuously monitored. During the procedure, oxygen supplementation through nasal cannulae was used for all patients. ES, using appropriate sphincterotomy (Ultratome XL, triple lumen sphincterotomy® and Ultratome, double lumen sphincterotomy®, Microvasive, Boston Scientific Co., Natick, MA, United States) was performed via a hydrophilic guide wire (Jagwire 0.025-inch or 0.035-inch®, Microvasive, Boston Scientific Co., Natick, MA, United States) to achieve controlled cutting. The length of ES performed depended on stone size. In cases of difficult cannulation, a precut technique was performed using a needle-knife sphincterotome (Microknife XL, triple lumen Needle Knife®, Microvasive, Boston Scientific Co., Natick, MA, United States). EBD of the ampulla was carried out using a balloon through the scope (Hercules, wire guided balloon®, Cook Ireland Ltd. and CRE®, Microvasive, Boston Scientific Co., Natick, MA, United States). The size of the balloon’s insufflation depended on the stone’s size and CBD dilation and it was performed until achieving a 16 mm diameter. EBD was performed under endoscopic and fluoroscopic guidance. The balloon was gradually filled with diluted contrast agent and it was maintained inflated in position for 45 to 60 s before deflation and removal. After EBD, stone clearance was routinely performed under fluoroscopic guidance using a basket (Retrival staintess steel basket umbrella 5 Fr or 7 Fr, Innoflex®, Innovamedica, Milan, Italy) and balloon catheter (Extractor XL triple lumen retrieval balloon®, Microvasive, Boston Scientific Co., Natick, MA, United States). In cases of difficult stone extraction with these techniques, we adopted ML (Soehendra lithotriptor®, Wilson-Cook Ireland Ltd.). As extracorporeal shock wave lithotripsy is not available at our center, when complete stone extraction was not achieved, a biliary plastic stent (Cotton-Huibregtse® Biliary stent, Cook Ireland Ltd.) or a naso-biliary tube (Flexima nasobiliary catheter®, Microvasive, Boston Scientific Co., Natick, MA, United States) was positioned for bile duct drainage. Post-ERCP complications and their severity were defined according to the 1991 consensus guidelines[4].
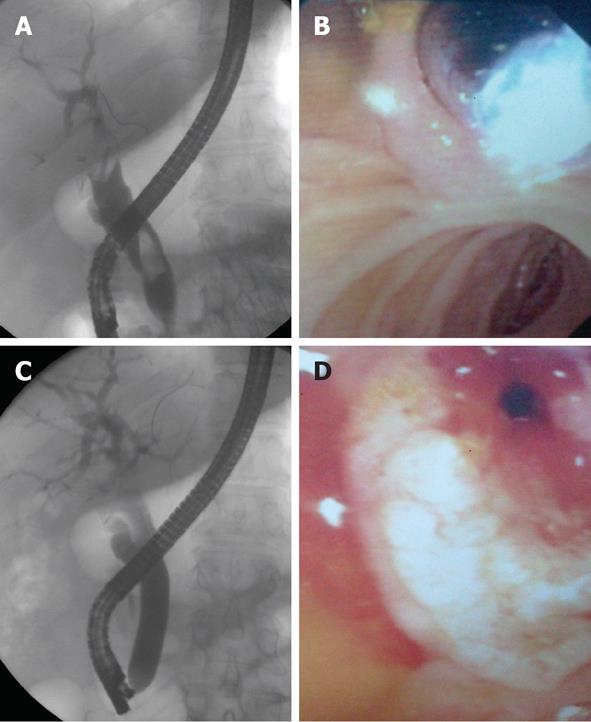
A total of 14 patients (9 female, 5 male; mean age of 73 years; range 57-82 years) were enrolled in the study, in whom a total of 15 EBDs were performed. The main patient characteristics are summarized in Table 1. All patients underwent minor ES prior to the EBD. The size of balloon insufflation depended on stone size and CBD dilation and this was performed until it reached 16 mm in diameter (Figure 1). The need for precutting the major papilla was 21.4% (3/14 ERCPs-EBD). In one case of an 81-year-old male, EBD was performed in a Billroth II (B-II) surgery. Periampullary diverticula (PAD) were found only in a 74-year-old female. Stone removal was achieved in a single session in 78.6% (11/14 ERCPs-EBD). Four patients required ML (26.6%), two stent insertions (13.3%) and two Silverman needle biopsy placement (13.3%).
| No. | Pre-cut | CBD dilation | Stone (mm) | EBD (mm) | ML | Stent | NBD | Complications |
| 1 | --- | Yes | 151 | 10 | Yes | --- | --- | --- |
| 2 | Yes | Yes | 30 | 10 | --- | --- | --- | --- |
| 3 | Yes | Yes | 101 | 12 | --- | --- | --- | --- |
| 4 | --- | Yes | 101 | 12 | --- | --- | --- | --- |
| 5 | --- | Yes | 201 | 12 | --- | --- | --- | --- |
| 6 | --- | Yes | 201 | 12 | Yes | --- | --- | --- |
| 7 | --- | Yes | 201 | 12 | --- | --- | --- | --- |
| 8 | --- | Yes | 15 | 10 | --- | --- | --- | --- |
| 9 | --- | Yes | 40 | 12 | --- | --- | --- | --- |
| 10 | --- | Yes | 251 | 13 | Yes | 10 Fr | --- | Bleeding |
| 11 | --- | Yes | 251 | 16 | --- | 10 Fr | 6 Fr | --- |
| 12 | --- | Yes | 151 | 12 | --- | --- | --- | --- |
| 13 | Yes | Yes | 20 | 12 | --- | --- | --- | --- |
| 14 | --- | Yes | 201 | 12 | --- | --- | --- | --- |
| 15 | --- | Yes | 35 | 16 | Yes | --- | 6 Fr | --- |
The adverse event related to the procedures (ERCP + ES) was intra procedural bleeding in 1 case (6.6%) which occurred after ES and was immediately treated with adrenaline sclerotherapy (1:10 000 dilution, 10 mL), with no further intervention, and no postoperative complications were reported.
The success rate of stone extraction following EBD ranges from 85% to 100%[7]. In patients with small stones (> 10 mm), EBD allows successful stone extraction, generally without the need for ES or ML. Bergman et al[12], in a prospective randomized controlled trial, assessed the outcome of 101 patients with CBD stones treated with EBD or ES. The authors concluded that the success rate of EBD was similar to ES, with no difference in the rate of early complications, such as pancreatitis. However, in patients with difficult stones (> 10 mm or number > 3), the success rate of EBD and ES is comparable but lithotripsy is required in about 50% of cases and an additional sphincterotomy or repeat ERCP in 15%-30% of patients[12]. A systematic review underlines that EBD is less successful than ES[13]. In our series, we performed ML in 4 cases, followed by the temporary placement of a plastic stent in one and naso-biliary drainage in another.
However, EBD seems to have several advantages over ES. The function of the biliary sphincter is preserved after EBD, while it is permanently lost after ES[14]. Regarding this consideration, Bergman et al[15] showed that the biliary sphincter was absent for up to 17 years after ES. This condition leads to chronic reflux of gastroduodenal contents into the biliary system, with subsequent bacterial colonization and inflammation. The potential benefit of EBD is in preventing this kind of reflux, even if until now, it is still controversial whether EBD is more efficacious in preventing bacterial contamination of the biliary tract than ES. Recently, Natsui et al[16] investigated the bacterial flora in the bile after these two procedures (EBD and ES). The authors concluded that EBD has the possibility of suppressing bacterial contamination of the biliary tract compared with ES in patients with small stones.
The risk of bleeding seems to be decreased in EBD compared to ES. In fact, while bleeding has been reported in 2%-5% of patients undergoing ES for bile duct stones[17], no significantly bleeding has been observed in over 1000 reported EBD procedures[12,15,18,19]. This characteristic makes EBD a safe procedure, especially in patients with an increased risk of bleeding, such as those with cirrhosis who have a six to eight fold risk of bleeding after ES[17,20]. In our cohort of patients, we had only 1 case of mild bleeding that occurred after ES and was successfully treated with sclerotherapy.
It is not clear whether or not this procedure is associated with a major risk of post-procedure pancreatitis since the available published studies report conflicting data. The meta-analysis of randomized, controlled trials by Baron et al[21] showed that the early complication rate of EBD was comparable to ES for removing CBD stones during ERCP. In particular, the rate of pancreatitis was higher in the EBD group compared to the ES group (7.4% vs 4.3%, P = 0.05). The mechanism of post-EBD hyperamylasemia and pancreatitis is not clear, even if it is implicated in the compression of the pancreatic duct. In fact, Bergman et al[22] underline how the balloon compression of the papilla or the pancreatic duct orifice may provoke peri-papillary edema or sphincter of Oddi spasm, leading to hyperamylasemia or pancreatitis. In this regard, a randomized controlled trial demonstrated that a 5 min dilation time rather than the conventional 1 min time resulted in an adequately loosened sphincter of Oddi and consequently reduced the risk of post ERCP pancreatitis and improved its efficacy[23].
We have not reported such complications but we want to underline that all our patients underwent prophylactic therapy, with gabexate mesilate 24 h before the procedure. Bergman et al[24] reported a randomized trial of EBD and ES for removing bile duct stones in patients with a prior B-II gastrectomy. Compared to patients with a normal anatomy, patients with a prior B-II gastrectomy had a significantly increased risk of bleeding after ES. Early complications occurred in 19% of the patients who underwent EBD compared to 39% of the patients who underwent ES[24].
In 2003, Ersoz et al[10] introduced the technique of endoscopic papillary large balloon dilatation (EPLBD) using a balloon larger than 12 mm after mid-incision ES for the removal of large CBD stones. Starting from that, multiple studies showed that EPLBD alone or in combination with other techniques can be useful for managing difficult biliary stones[25-28]. Several studies on EPLBD have demonstrated a relatively high technical success rate (74%-99%) for the removal of large bile duct stones and also for patients with PAD and relatively low rates of pancreatitis, without recurring to ML[10,29,30]. Recently, the incidence of biliary complications have been reported to be significantly lower in patients after EPLBD than in those after ES and this outcome appeared most markedly in patients who also underwent cholecystectomy[31].
Some authors have suggested that the stone recurrence rate may also be higher with EPLBD than with ES and ML[32]. However, the results of a Japanese multicenter trial with a mean follow up of 6.7 years demonstrated that there is a lower risk of stone recurrence following EPLBD when compared with ES[33]. Another study that evaluated the short term clinical outcomes after removing CBD stones using EPLBD showed a recurrence rate of 24.0% with a mean follow-up period of 10.8 ± 4.5 mo[34].
EBD and EPLBD are considered safe procedures for patients with an increased risk of bleeding. In fact, EPLBD is especially attractive in patients who are at risk for bleeding after ES or in those with altered anatomy, such as patients with a B-II gastrectomy in whom a full sphincterotomy cannot be successfully achieved. Choi et al[35] evaluated the efficacy and safety of EPLBD for removal of bile duct stones in patients with B-II gastrectomy. In all cases, stones were successfully removed without significant complications, such as bleeding, pancreatitis or perforation.
According to the study of Youn et al[36], EPLBD with a large balloon of over 15 mm with ES is an effective and safe procedure with a very low probability of severe post-procedural pancreatitis. The authors found five cases of not severe post-EPLBD pancreatitis. This complication was not associated with larger balloon size (17.0 ± 2.4 mm) but was associated with longer procedure time (30.0 ± 3.5 min) and smaller dilation of the CBD (17.6 ± 6.7 mm).
To date, there are no data on the optimal duration of papillary balloon dilation after a biliary sphincterotomy. Paspatis et al[37] compared effectiveness and complications of the endoscopic papillary balloon dilation for 60 s vs 30 s after ES. A total of 124 patients were prospectively randomized to either the 60 s dilation group (G60, n = 60) or the 30 s dilation group (G30, n = 64). The complete removal of bile duct stones was similar between the two groups (86% vs 85%, P = 0.9), such as the rates of post-ERCP pancreatitis (3.1% vs 3.3%, P = 0.9). The authors concluded that 30 s papillary balloon dilation, performed after ES for the management of bile duct stones, is equally effective as the 60 s papillary balloon dilation. In our cohort of patients, we maintained the inflated balloon in position for 45 to 60 s before deflation and removal.
In conclusion, therapeutic ERCP, including in a low-volume center, represents the first line management option for CBD stones. With the current endoscopic techniques, very few patients with choledocholithiasis require surgery. The data emerging from our study confirm that EBD, performed for large CBD stones, is an efficacious and safe procedure.
Endoscopic sphincterotomy (ES) was always considered the standard therapy for the treatment of common bile duct (CBD) stones but this procedure may fail in cases of difficult stones (large, hard and confluence). Endoscopic balloon dilation (EBD) is actually recognized as an alternative to ES for the treatment of these conditions. Many studies have reported the use of small diameter balloons (6-10 mm), while the ones using larger balloons (from 12 to 20 mm) are rare.
EBD is not still widely embraced, especially due to the fear of complications, in particular, of acute pancreatitis. However, EBD does not have the short term complications of bleeding and perforation compared to ES and it may preserve the biliary sphincter with a decrease in long term complications.
For the extraction of difficult bile duct stones, the dilation of the biliary orifice with a large balloon after a small ES appears to be a promising technique.
The study results suggest that large EBD is an efficacious and safe procedure that could be used for treating difficult CBD stones.
EBD is a procedure performed under endoscopic and fluoroscopic guidance in which the balloon is inflated with diluted contrast agent and is located across the papilla. The size of the balloon’s insufflation depends on the stone size and CBD dilation; mechanical lithotripsy (ML) is a method of stone extraction performed under fluoroscopic guidance. MLs are devices designed to break stones which have been captured within a basket.
The authors report the results of 14 patients who underwent endoscopic papillary balloon dilatation for difficult CBD stones. The patients had good outcomes, without major short and long term complications.
P- Reviewers Souza JLS, Conti A, Skok P S- Editor Zhai HH L- Editor Roemmele A E- Editor Zheng XM
| 1. | Mugica F, Urdapilleta G, Castiella A, Berbiela A, Alzate F, Zapata E, Zubiaurre L, Lopez P, Arenas JI. Selective sphincteroplasty of the papilla in cases at risk due to atypical anatomy. World J Gastroenterol. 2007;13:3106-3111. [PubMed] |
| 2. | Classen M, Demling L. [Endoscopic sphincterotomy of the papilla of vater and extraction of stones from the choledochal duct (author’s transl)]. Dtsch Med Wochenschr. 1974;99:496-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 391] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 3. | Kawai K, Akasaka Y, Murakami K, Tada M, Koli Y. Endoscopic sphincterotomy of the ampulla of Vater. Gastrointest Endosc. 1974;20:148-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 453] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2036] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 5. | May GR, Cotton PB, Edmunds SE, Chong W. Removal of stones from the bile duct at ERCP without sphincterotomy. Gastrointest Endosc. 1993;39:749-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 67] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Mathuna PM, White P, Clarke E, Merriman R, Lennon JR, Crowe J. Endoscopic balloon sphincteroplasty (papillary dilation) for bile duct stones: efficacy, safety, and follow-up in 100 patients. Gastrointest Endosc. 1995;42:468-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 146] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 7. | Staritz M, Ewe K, Meyer zum Büschenfelde KH. Endoscopic papillary dilation (EPD) for the treatment of common bile duct stones and papillary stenosis. Endoscopy. 1983;15 Suppl 1:197-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 8. | Gerke H, Baillie J. To cut or stretch. Am J Gastroenterol. 2004;99:1461-1463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Watanabe H, Yoneda M, Tominaga K, Monma T, Kanke K, Shimada T, Terano A, Hiraishi H. Comparison between endoscopic papillary balloon dilatation and endoscopic sphincterotomy for the treatment of common bile duct stones. J Gastroenterol. 2007;42:56-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 256] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 11. | Bang S, Kim MH, Park JY, Park SW, Song SY, Chung JB. Endoscopic papillary balloon dilation with large balloon after limited sphincterotomy for retrieval of choledocholithiasis. Yonsei Med J. 2006;47:805-810. [PubMed] |
| 12. | Bergman JJ, Rauws EA, Fockens P, van Berkel AM, Bossuyt PM, Tijssen JG, Tytgat GN, Huibregtse K. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bileduct stones. Lancet. 1997;349:1124-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 274] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Weinberg BM, Shindy W, Lo S. Endoscopic balloon sphincter dilation (sphincteroplasty) versus sphincterotomy for common bile duct stones. Cochrane Database Syst Rev. 2006;4:CD004890. [PubMed] |
| 14. | Minami A, Nakatsu T, Uchida N, Hirabayashi S, Fukuma H, Morshed SA, Nishioka M. Papillary dilation vs sphincterotomy in endoscopic removal of bile duct stones. A randomized trial with manometric function. Dig Dis Sci. 1995;40:2550-2554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 130] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Bergman JJ, van Berkel AM, Groen AK, Schoeman MN, Offerhaus J, Tytgat GN, Huibregtse K. Biliary manometry, bacterial characteristics, bile composition, and histologic changes fifteen to seventeen years after endoscopic sphincterotomy. Gastrointest Endosc. 1997;45:400-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Natsui M, Honma T, Genda T, Nakadaira H. Effects of endoscopic papillary balloon dilation and endoscopic sphincterotomy on bacterial contamination of the biliary tract. Eur J Gastroenterol Hepatol. 2011;23:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Freeman ML. Complications of endoscopic biliary sphincterotomy: a review. Endoscopy. 1997;29:288-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Fujita N, Maguchi H, Komatsu Y, Yasuda I, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K. Endoscopic sphincterotomy and endoscopic papillary balloon dilatation for bile duct stones: A prospective randomized controlled multicenter trial. Gastrointest Endosc. 2003;57:151-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 167] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Disario JA, Freeman ML, Bjorkman DJ, Macmathuna P, Petersen BT, Jaffe PE, Morales TG, Hixson LJ, Sherman S, Lehman GA. Endoscopic balloon dilation compared with sphincterotomy for extraction of bile duct stones. Gastroenterology. 2004;127:1291-1299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 239] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 20. | Nelson DB, Freeman ML. Major hemorrhage from endoscopic sphincterotomy: risk factor analysis. J Clin Gastroenterol. 1994;19:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Baron TH, Harewood GC. Endoscopic balloon dilation of the biliary sphincter compared to endoscopic biliary sphincterotomy for removal of common bile duct stones during ERCP: a metaanalysis of randomized, controlled trials. Am J Gastroenterol. 2004;99:1455-1460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 212] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 22. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. Is endoscopic balloon dilation for removal of bile duct stones associated with an increased risk for pancreatitis or a higher rate of hyperamylasemia. Endoscopy. 2001;33:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 23. | Liao WC, Lee CT, Chang CY, Leung JW, Chen JH, Tsai MC, Lin JT, Wu MS, Wang HP. Randomized trial of 1-minute versus 5-minute endoscopic balloon dilation for extraction of bile duct stones. Gastrointest Endosc. 2010;72:1154-1162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 24. | Bergman JJ, van Berkel AM, Bruno MJ, Fockens P, Rauws EA, Tijssen JG, Tytgat GN, Huibregtse K. A randomized trial of endoscopic balloon dilation and endoscopic sphincterotomy for removal of bile duct stones in patients with a prior Billroth II gastrectomy. Gastrointest Endosc. 2001;53:19-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 26. | Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 27. | Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720-76; quiz 768, 771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 28. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Kim JH. Factors Predictive of Adverse Events Following Endoscopic Papillary Large Balloon Dilation: Results from a Multicenter Series. Dig Dis Sci. 2012;Epub ahead of print. [PubMed] |
| 29. | Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW, Bhattacharya K, Gupta K. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 125] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 30. | Lee JW, Kim JH, Kim YS, Choi HS, Kim JS, Jeong SH, Ha MS, Ku YS, Kim YS, Kim JH. [The effect of periampullary diverticulum on the outcome of bile duct stone treatment with endoscopic papillary large balloon dilation]. Korean J Gastroenterol. 2011;58:201-207. [PubMed] |
| 31. | Doi S, Yasuda I, Mukai T, Iwashita T, Uemura S, Yamauchi T, Nakashima M, Adachi S, Shimizu M, Tomita E. Comparison of long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation: a propensity score-based cohort analysis. J Gastroenterol. 2012;Epub ahead of print. [PubMed] |
| 32. | Lee DK, Jahng JH. Alternative methods in the endoscopic management of difficult common bile duct stones. Dig Endosc. 2010;22 Suppl 1:S79-S84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 33. | Yasuda I, Fujita N, Maguchi H, Hasebe O, Igarashi Y, Murakami A, Mukai H, Fujii T, Yamao K, Maeshiro K. Long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation for bile duct stones. Gastrointest Endosc. 2010;72:1185-1191. [PubMed] |
| 34. | Kim JH, Kim YS, Kim DK, Ha MS, Lee YJ, Lee JJ, Lee SJ, Won IS, Ku YS, Kim YS. Short-term Clinical Outcomes Based on Risk Factors of Recurrence after Removing Common Bile Duct Stones with Endoscopic Papillary Large Balloon Dilatation. Clin Endosc. 2011;44:123-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Choi CW, Choi JS, Kang DH, Kim BG, Kim HW, Park SB, Yoon KT, Cho M. Endoscopic papillary large balloon dilation in Billroth II gastrectomy patients with bile duct stones. J Gastroenterol Hepatol. 2012;27:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 36. | Youn YH, Lim HC, Jahng JH, Jang SI, You JH, Park JS, Lee SJ, Lee DK. The increase in balloon size to over 15 mm does not affect the development of pancreatitis after endoscopic papillary large balloon dilatation for bile duct stone removal. Dig Dis Sci. 2011;56:1572-1577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 37. | Paspatis GA, Konstantinidis K, Tribonias G, Voudoukis E, Tavernaraki A, Theodoropoulou A, Chainaki I, Manolaraki M, Chlouverakis G, Vardas E. Sixty- versus thirty-seconds papillary balloon dilation after sphincterotomy for the treatment of large bile duct stones: A randomized controlled trial. Dig Liver Dis. 2013;45:301-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |