Copyright
©The Author(s) 2021.
World J Clin Cases. Dec 16, 2021; 9(35): 10927-10936
Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10927
Published online Dec 16, 2021. doi: 10.12998/wjcc.v9.i35.10927
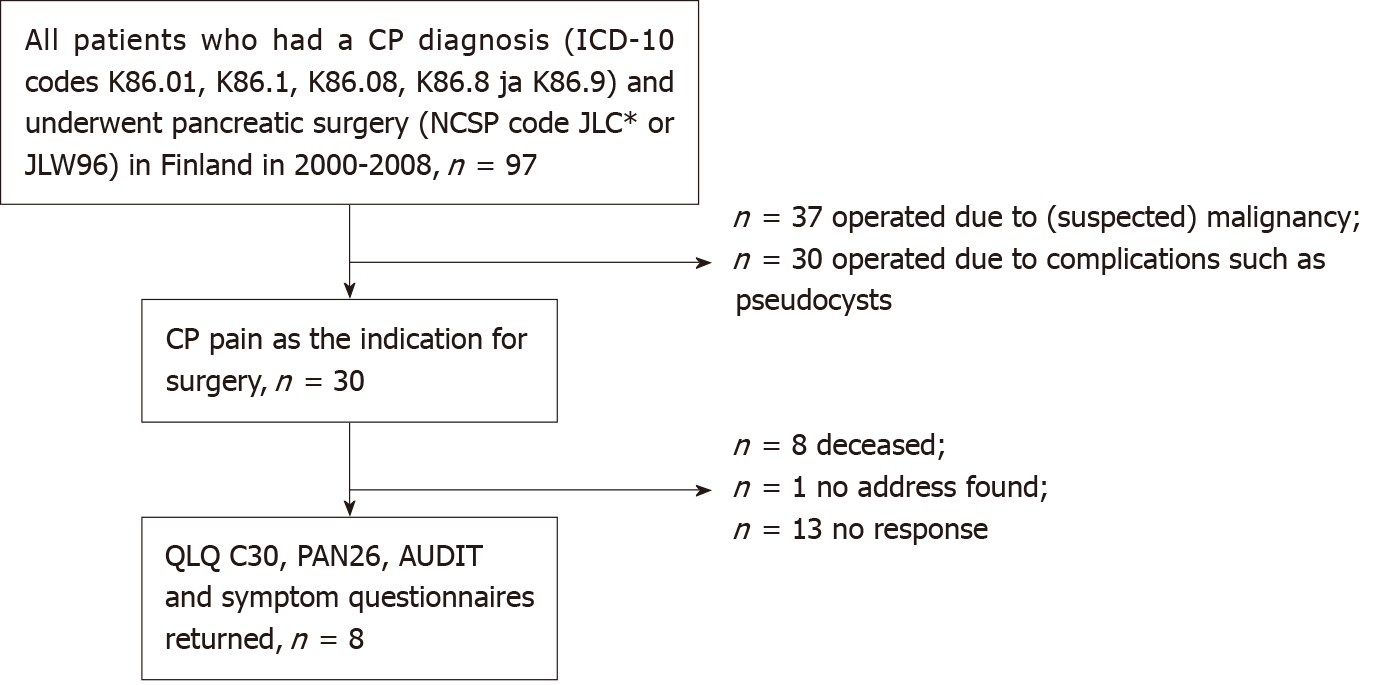
Figure 1 Flowchart of patients.
The study included all patients who underwent pancreatic surgery for chronic pancreatitis in the whole of Finland in 2000-2008. CP: Chronic pancreatitis.
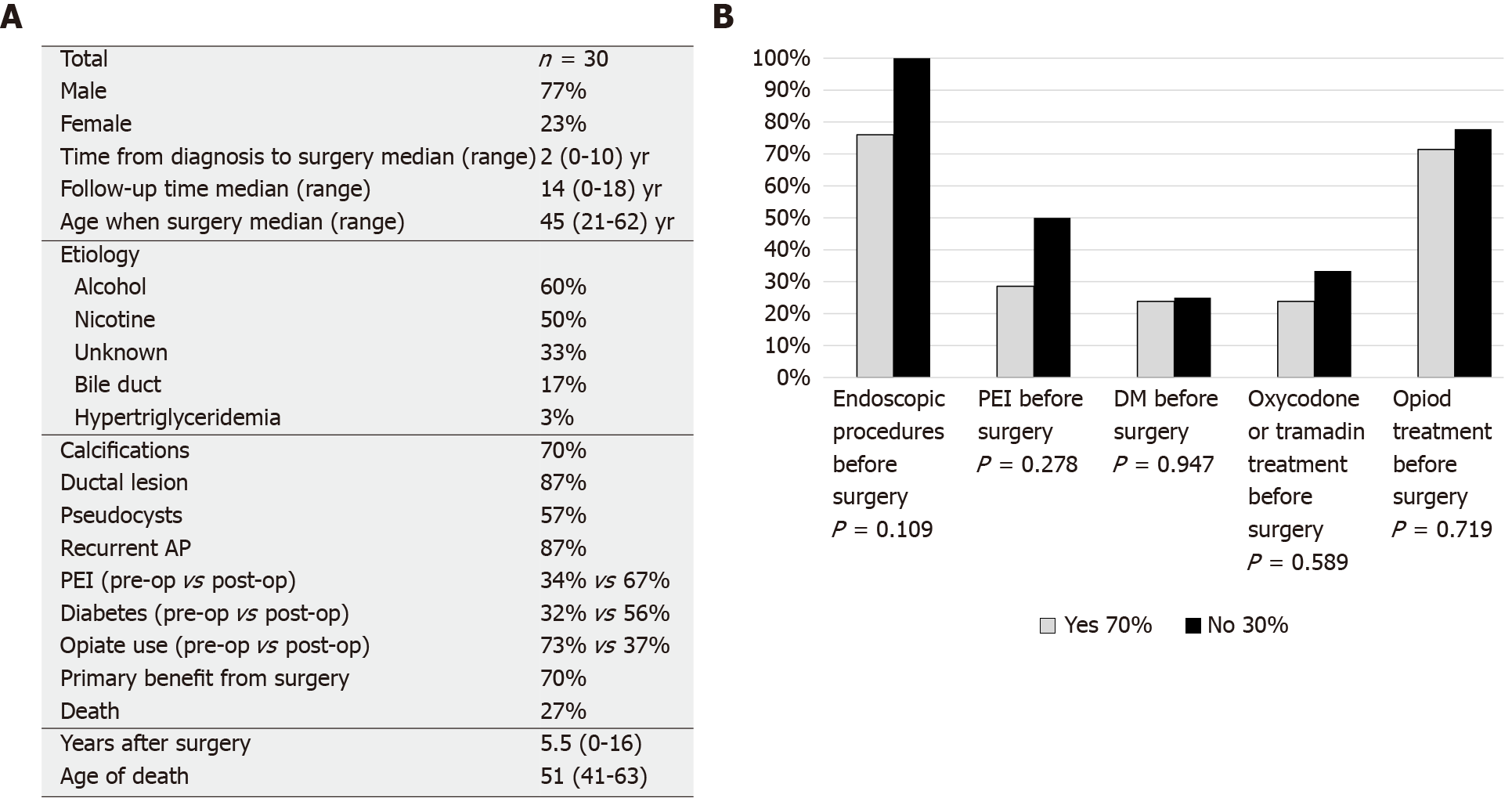
Figure 2 Demographics and outcome of chronic pancreatitis surgery.
A: Demographics of the surgical chronic pancreatitis patients; B: Surgical chronic pancreatitis patients grouped based on pain relief approximately one year after surgery. AP: Acute pancreatitis; PEI: Pancreatic exocrine insufficiency; DM: Diabetes mellitus.
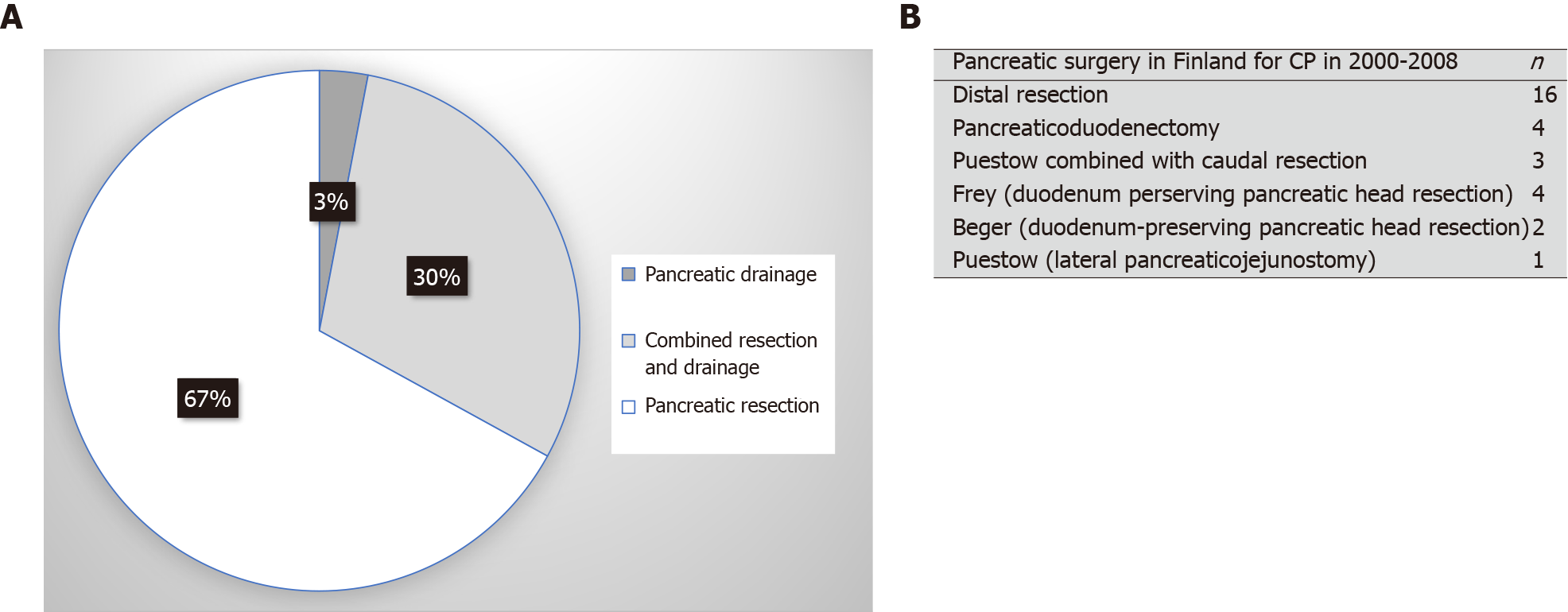
Figure 3 Distribution of chronic pancreatitis surgery in Finland.
A: Type of surgery for chronic pancreatitis. Most operations involved a pancreatic resection (pancreaticoduodenectomy or a distal resection); B: Type of surgical operations in detail. CP: Chronic pancreatitis.
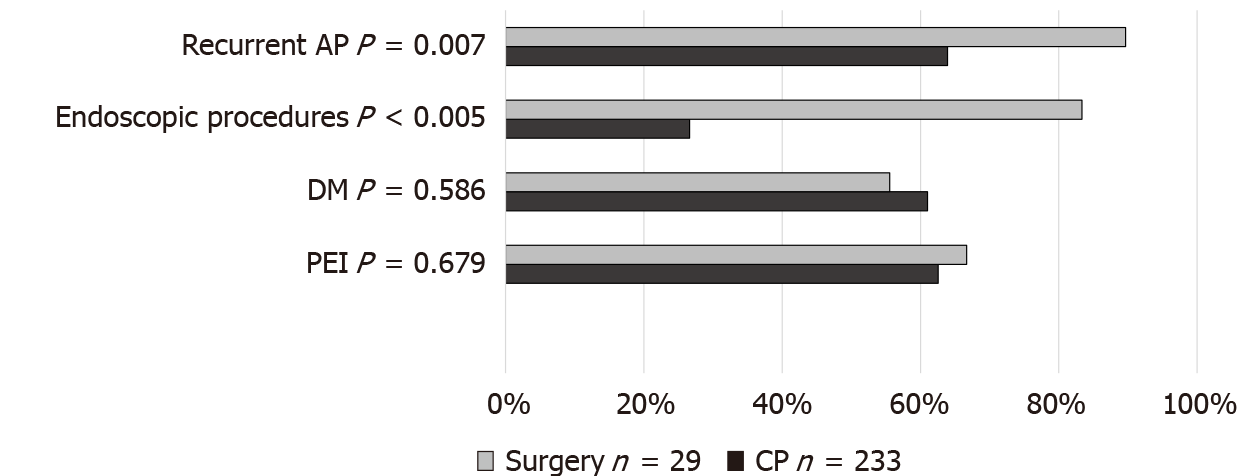
Figure 4 Surgical chronic pancreatitis patients compared to control population, which included nonsurgical chronic pancreatitis patients from the Finnish chronic pancreatitis cohort from 2014 to 2015 (n = 233).
There was more recurrent acute pancreatitis and prior endoscopic procedures in the chronic pancreatitis patients who underwent surgery. Pancreatic insufficiency and diabetes were similar between the groups. CP: Chronic pancreatitis; AP: Acute pancreatitis; PEI: Pancreatic exocrine insufficiency; DM: Diabetes mellitus.
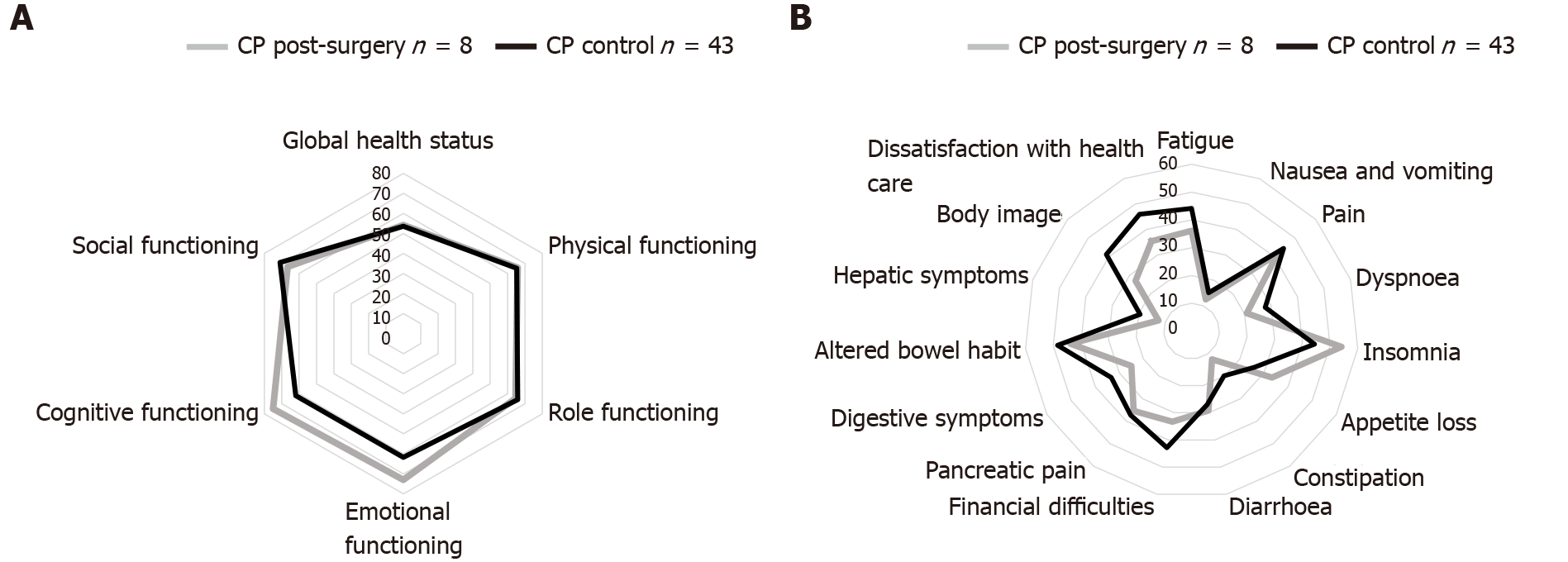
Figure 5 Quality of life in the chronic pancreatitis patients who underwent surgery, compared to control chronic pancreatitis patients.
All patients who answered the quality of life (QoL) questionnaire in the surgical group were smokers. The control group consisted of Finnish chronic pancreatitis patients who did not have surgery and smoking contributing to their disease. A and B: QoL functioning (A) and symptom scores (B) had a tendency to be better in most parameters in the surgical group, but without significance. A higher score was better in the functioning scores (A), and a lower score was better in the symptoms scores (B). CP: Chronic pancreatitis.
- Citation: Parhiala M, Sand J, Laukkarinen J. Surgery for chronic pancreatitis in Finland is rare but seems to produce good long-term results. World J Clin Cases 2021; 9(35): 10927-10936
- URL: https://www.wjgnet.com/2307-8960/full/v9/i35/10927.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i35.10927