Copyright
©The Author(s) 2021.
World J Clin Cases. Aug 26, 2021; 9(24): 7279-7284
Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7279
Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7279
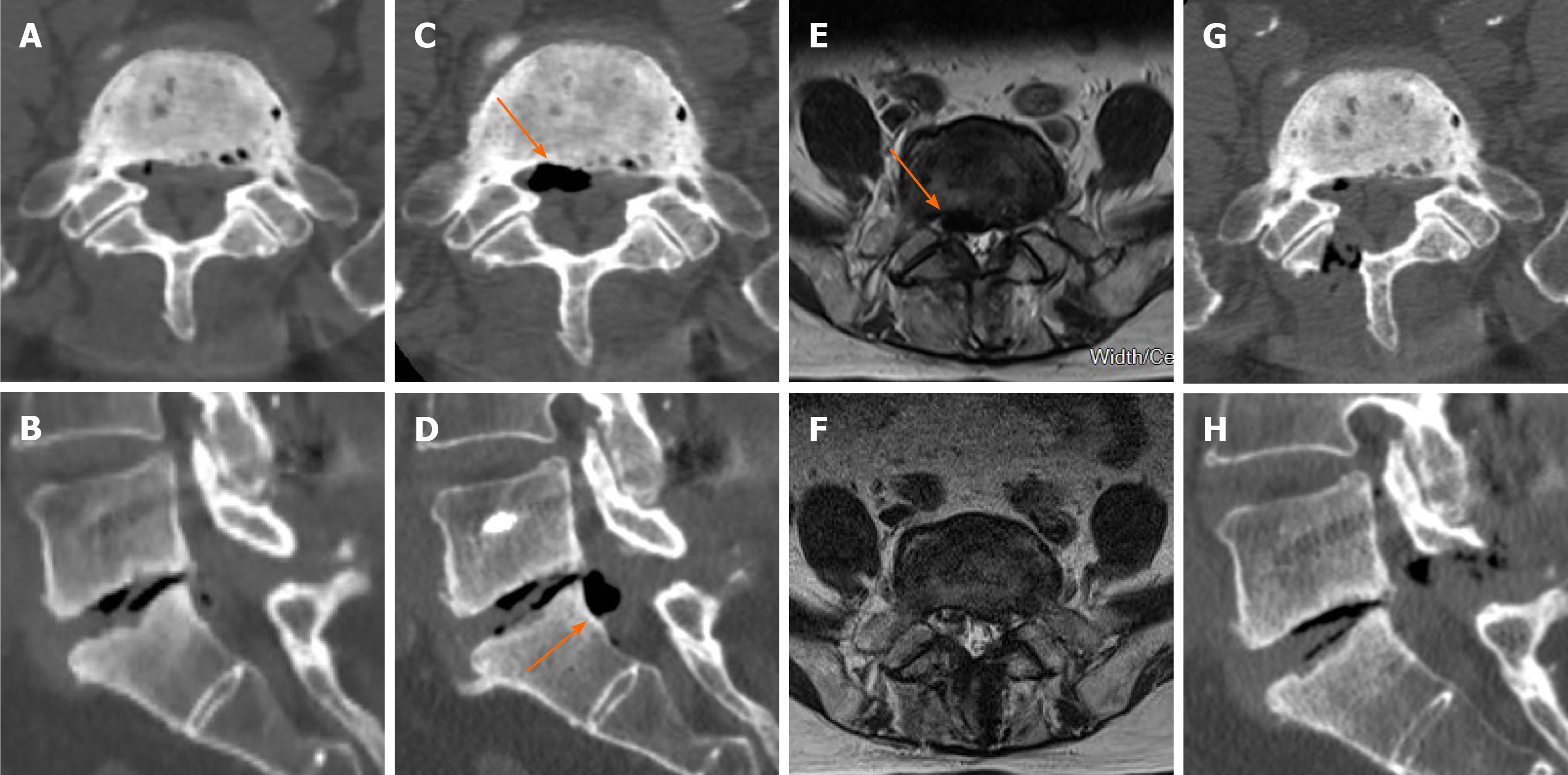
Figure 1 An 87-year-old man with right S1 radiculopathy.
A: Axial computed tomography (CT) image showing no gas accumulation in the spinal canal 40 d before radiculopathy onset; B: Sagittal CT image reconstruction shows no gas accumulation in the spinal canal and the vacuum phenomenon at the L5/S1 level 40 d before radiculopathy onset; C and D: Axial CT image and sagittal CT image reconstruction showing the vacuum phenomenon (orange arrows) in the spinal canal after radiculopathy onset; E: T2-weighted axial image showing an oval-shaped low signal intensity lesion (orange arrow) in the spinal canal after radiculopathy onset; F: T2-weighted axial image showing no low signal intensity lesion in the spinal canal after percutaneous endoscopic decompression; G and H: Axial CT image and sagittal CT image reconstruction showing the resolution of the vacuum phenomenon after percutaneous endoscopic decompression.
Figure 2 Digital pictures taken during percutaneous endoscopic decompression.
A: The blister-like membranous structure of the gas-containing cyst located in the posterolateral region of the spinal canal; B: A 20 G needle was used to puncture the gas-containing cyst before gas extraction; C: The gas was extracted into the syringe, and the scale shows that almost 1 mL of gas was extracted; D: Pathological examination showed that the picked gas-containing pseudocyst tissue is fibrous connective tissue (× 100); E: The wall of the gas-containing pseudocyst was fibrous connective tissue and lined with flat cells (× 200).
- Citation: Chen Y, Yu SD, Lu WZ, Ran JW, Yu KX. Epidural gas-containing pseudocyst leading to lumbar radiculopathy: A case report. World J Clin Cases 2021; 9(24): 7279-7284
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7279.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7279