Copyright
©The Author(s) 2021.
World J Clin Cases. May 26, 2021; 9(15): 3631-3636
Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3631
Published online May 26, 2021. doi: 10.12998/wjcc.v9.i15.3631
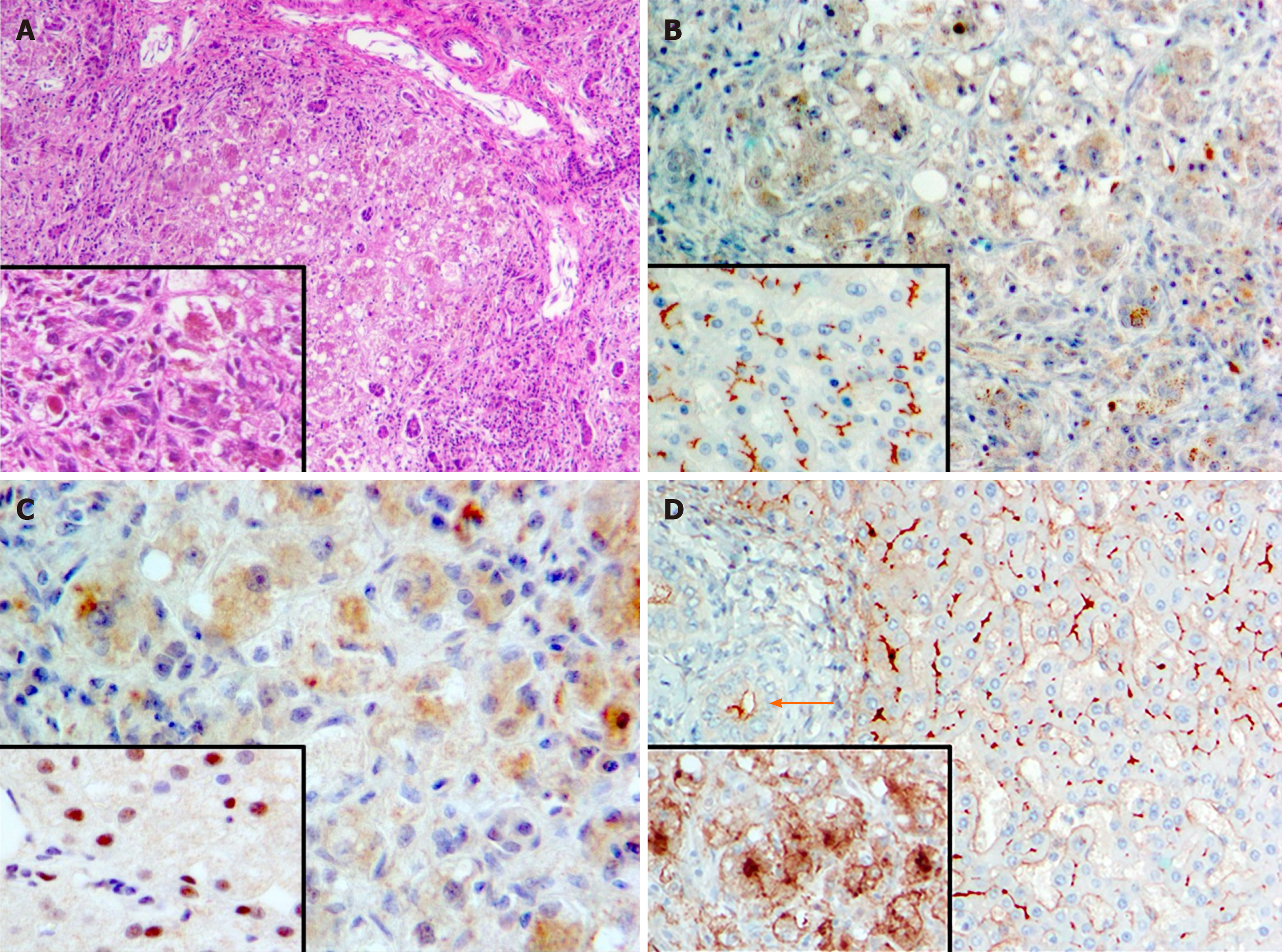
Figure 1 Histopathologic findings, explanted liver and controls.
A: Fibrosis and nodularity with steatosis and substantial lobular disarray, explanted liver. Pronounced cholestasis spares portal tracts. Hematoxylin & eosin; main image 100 ×, inset 200 × original magnifications; B: Bile salt export pump expression in normal liver (“control”) and explanted liver. No expression in explanted liver (main image); the pigment seen is bile. Control (inset), crisp expression along an unremarkable bile-canaliculus network. Anti-bile salt export pump antibody (Santa Cruz Biotechnology, Dallas, TX, United States; sc-74500)/hematoxylin; both main image and inset 200 × original magnifications; C: Farnesoid X receptor expression in normal liver (“control”) and explanted liver. No expression in explanted liver (main image); the pigment seen is bile. Control (inset), nuclear expression evident in most hepatocytes. Anti-farnesoid X receptor antibody (Santa Cruz Biotechnology; sc-25309)/hematoxylin; both main image and inset 400 × original magnifications; D: Gamma-glutamyl transpeptidase expression in normal liver (“control”) and explanted liver. Control (main image), crisp expression at apices of cholangiocytes (arrow) and along an unremarkable bile-canaliculus network, with faint perisinusoidal staining. Explanted liver (inset), blurred marking at severely distorted canalicular network with pronounced cytoplasmic and basolateral staining, abnormalities that reflect the extent of hepatocellular injury and disarray. Anti-gamma-glutamyl transpeptidase 1 (Abnova, Taipei, Taiwan; H00002678-M01)/hematoxylin; both main image and inset 200 × original magnifications.
- Citation: Czubkowski P, Thompson RJ, Jankowska I, Knisely AS, Finegold M, Parsons P, Cielecka-Kuszyk J, Strautnieks S, Pawłowska J, Bull LN. Progressive familial intrahepatic cholestasis — farnesoid X receptor deficiency due to NR1H4 mutation: A case report. World J Clin Cases 2021; 9(15): 3631-3636
- URL: https://www.wjgnet.com/2307-8960/full/v9/i15/3631.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i15.3631