Copyright
©The Author(s) 2021.
World J Clin Cases. May 6, 2021; 9(13): 3147-3156
Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3147
Published online May 6, 2021. doi: 10.12998/wjcc.v9.i13.3147
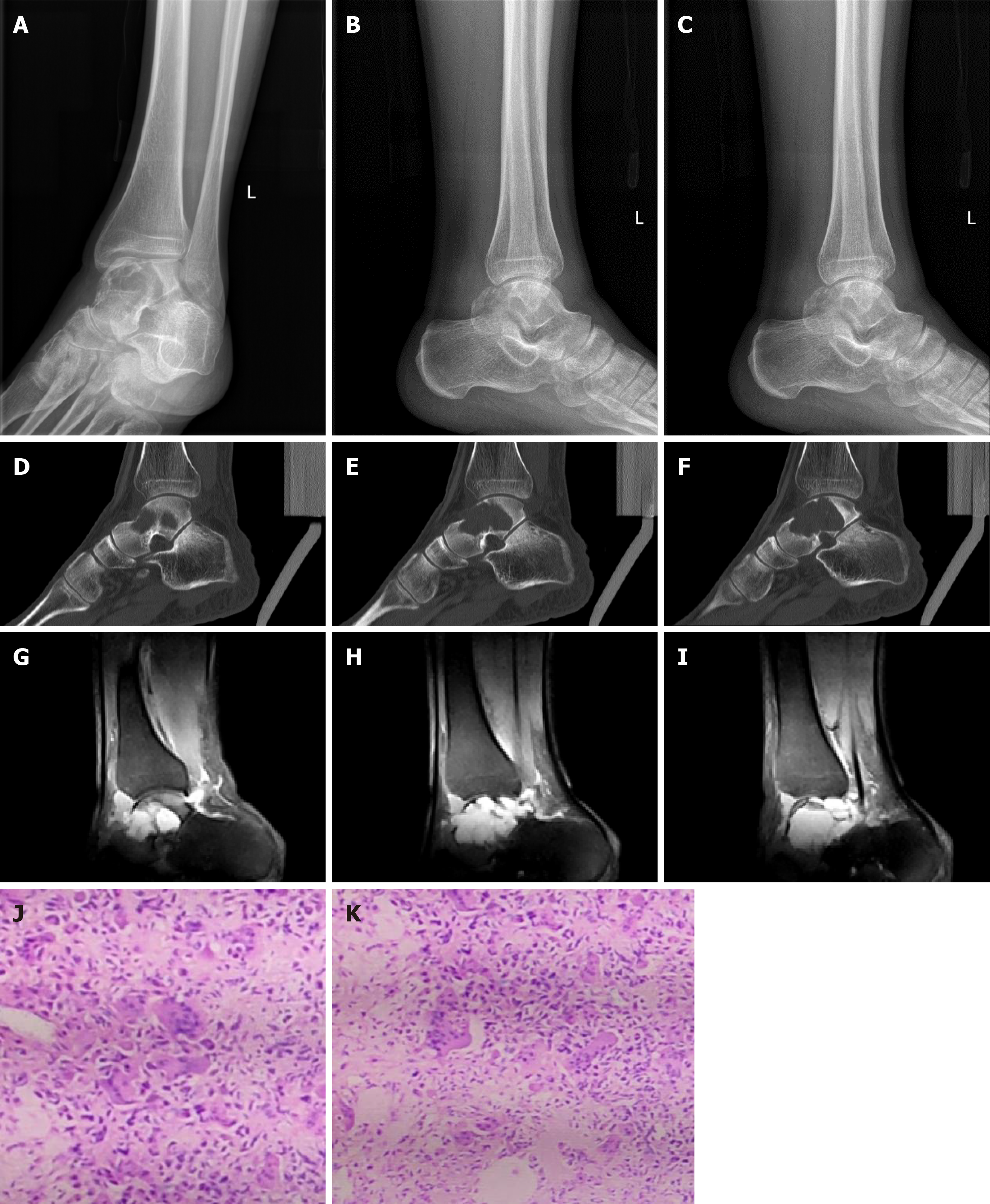
Figure 1 Preoperative imaging results.
A-C: Preoperative radiographs; D-F: Preoperative computerized tomography images; G-I: Preoperative magnetic resonance imaging suggested a giant cell tumor of the talus; J and K: Pathological images.
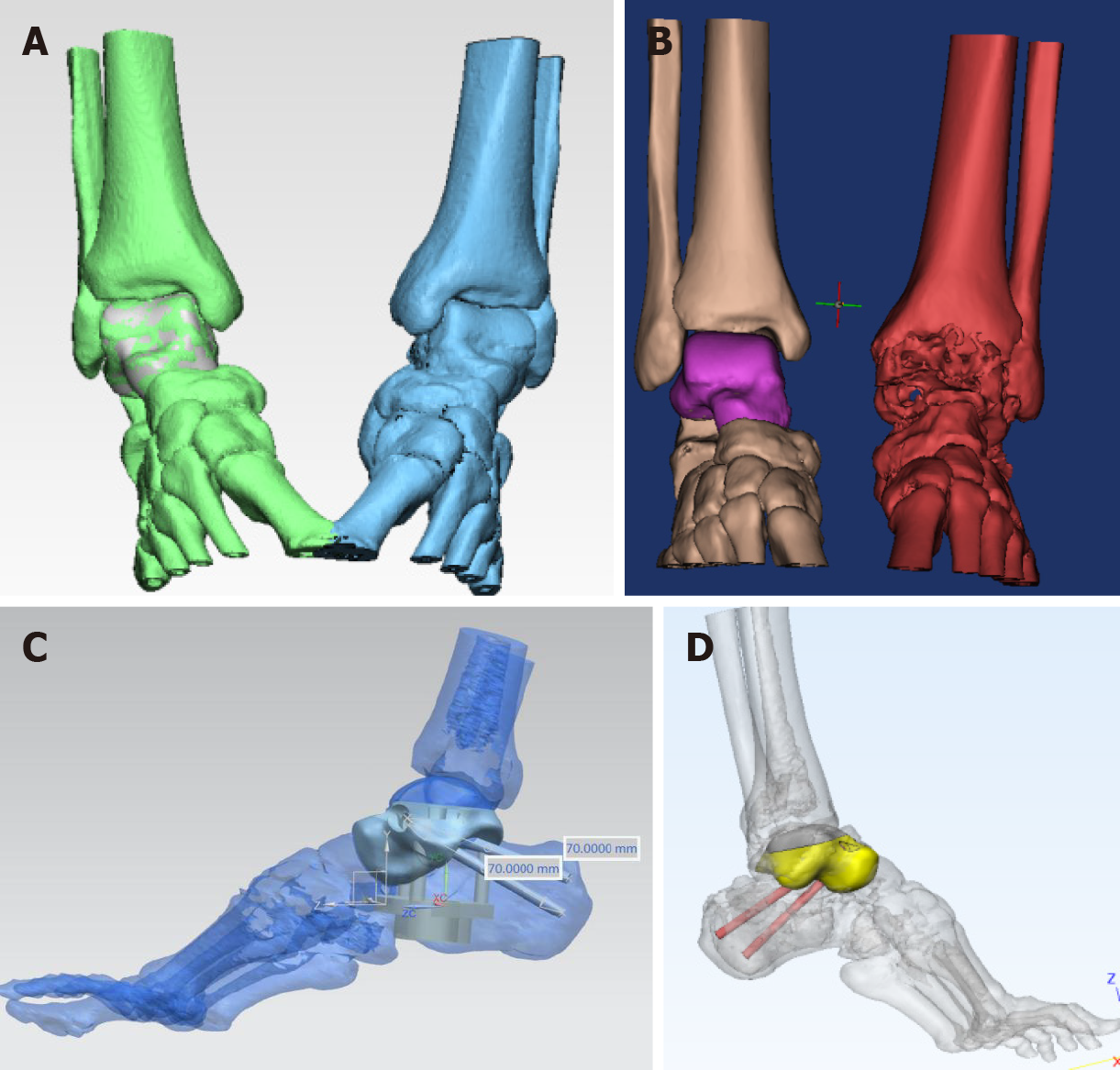
Figure 2 Casting process for the three-dimensional printed personalized prosthesis.
Through three-dimensional (3D) computerized tomography and magnetic resonance imaging post-processing technology, the tomographic image processing and segmentation were carried out to obtain the complete data of the patient area, and the image technology and data registration technology were used to reconstruct and match the intact three-dimensional original data of the patient side. The serious data defects of necrotic talus on the affected side were repaired by reverse repair technology, the original data of defect-free talus reconstruction were obtained, and the tibial distance, distance boat, and subtalar joint surface were analyzed and smoothed to complete the personalized three-dimensional reconstruction of talus prosthesis. Reconstruction and manufacture of complex anatomical structure of soft and hard tissues were performed by three-dimensional printing technology. A: Complete data of the affected area were acquired by computerized tomography image processing and segmentation using 3D computerized tomography postprocessing technology; B: The 3D raw data of the affected side were obtained by reconstruction and matching performed with mirror and data registration technology; C: The data of the tibiotalar and subtalar articular facets were analyzed and processed; D: Accurate 3D reconstruction of the talar prosthesis was completed.
Figure 3 The three-dimensional printed personalized prosthesis with biological function A: Whole view of three dimensional (3D) print personalized talus prostheses; B: Articular side of 3D print personalized talus prosthesis tibialis; C: Subtalar joint side of 3D print personalized talus prosthesis.
On the tibia side, cocrmo material was used, the subtalar joint and subtalar joint surface were treated with micropores, and hydroxyapatite coating and nano-treatment were used to promote bone growth.
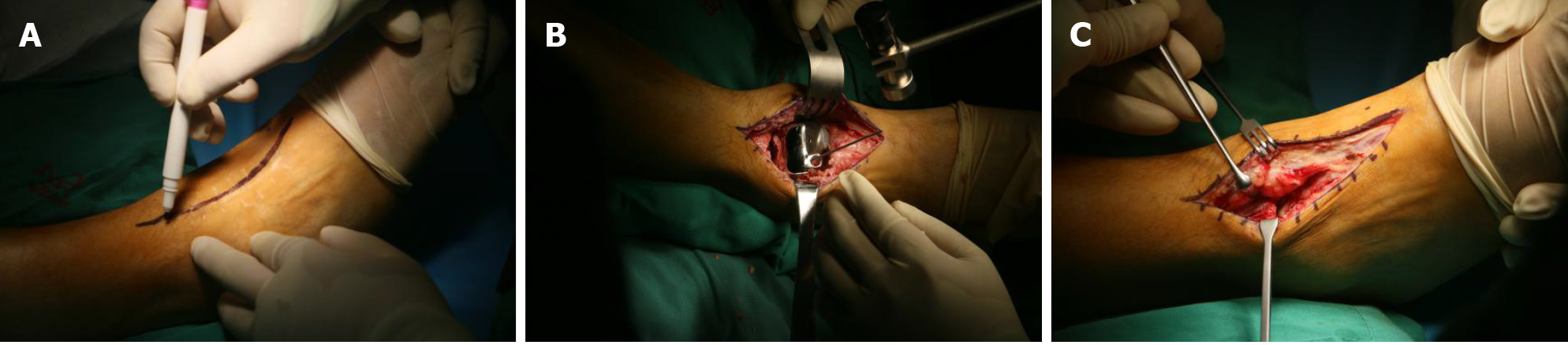
Figure 4 Surgical technique.
A: Preoperative anterior median approach marking; B: Resection of the talus and implantation of the prosthesis; C: Skin incision along anterior median approach.
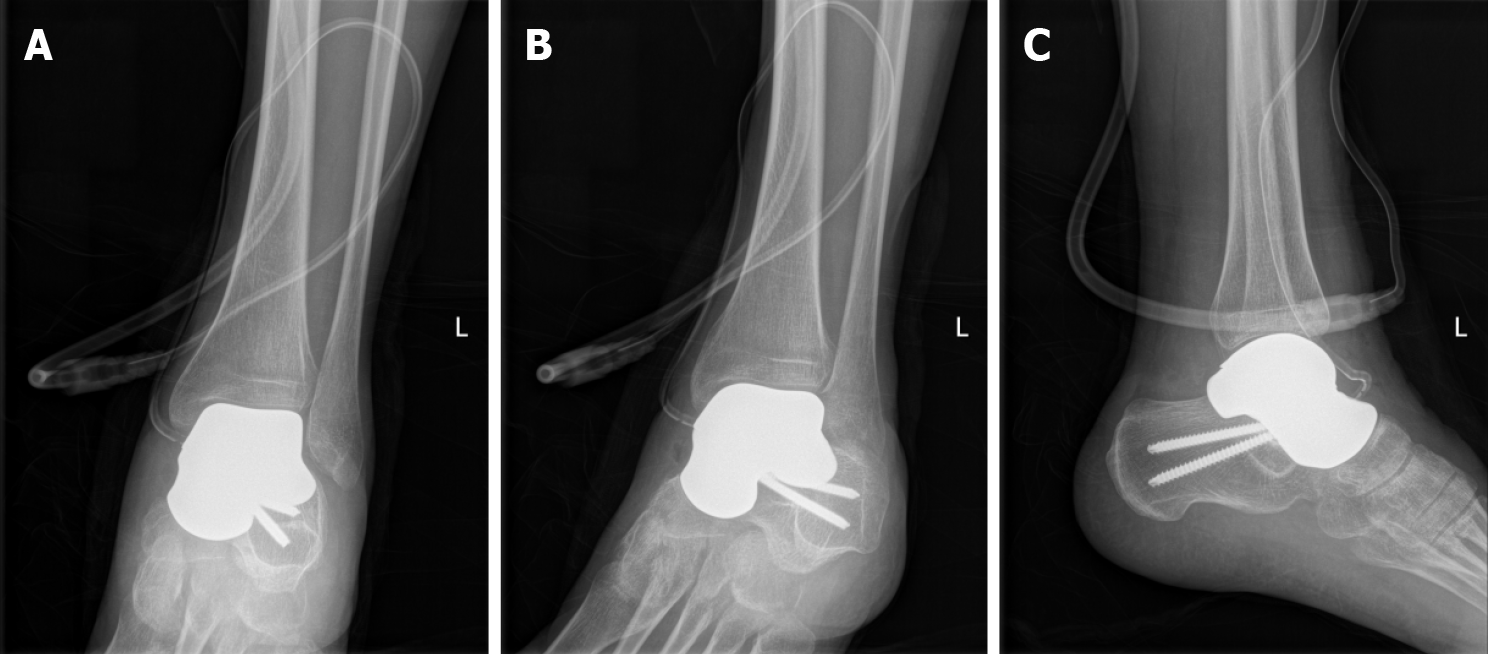
Figure 5 Radiographs on the day after surgery.
A and B: X-ray films of the ankle joint immediately after operation (front); C: X-ray film of the ankle joint immediately after operation (flank).
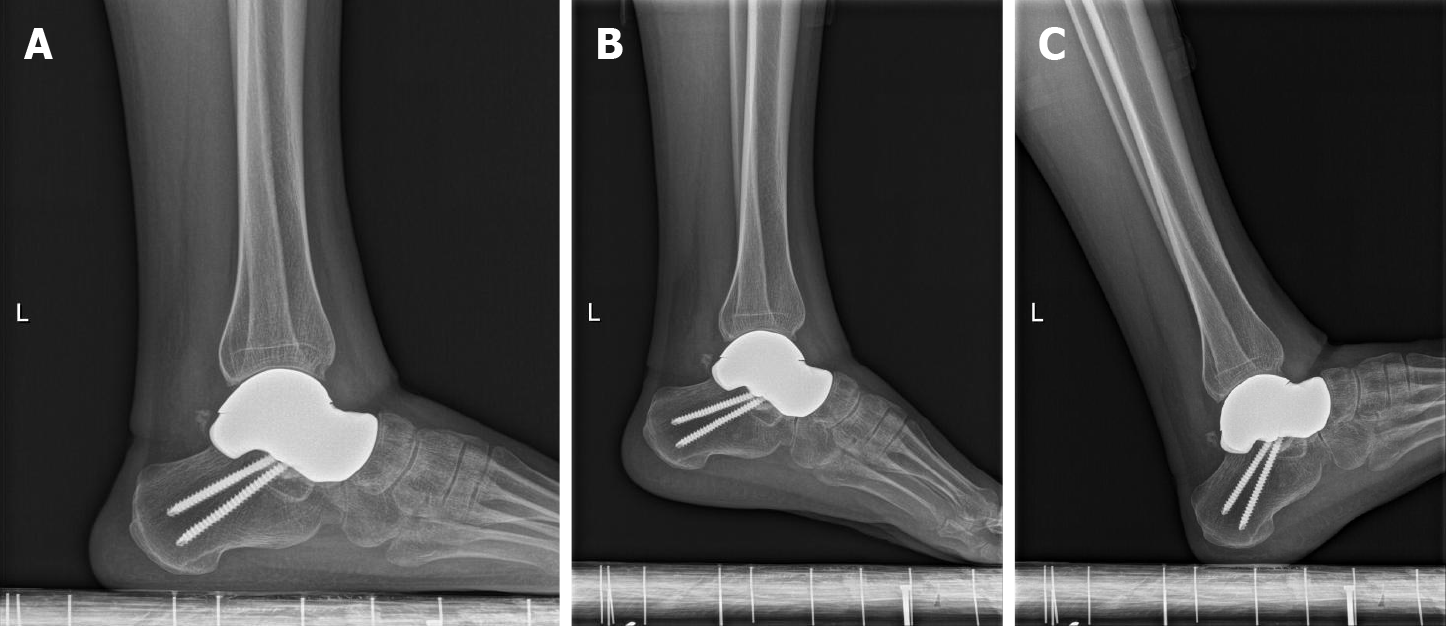
Figure 6 Postoperative radiographs (12 mo).
A: Lateral X-ray film of the ankle joint at 12 mo after operation; B: Extreme plantar flexion position; C: Extreme dorsiflexion position. The talus prosthesis was in place without displacement or subsidence, the surrounding bone was in good condition, and there was no instability or fracture around the prosthesis.
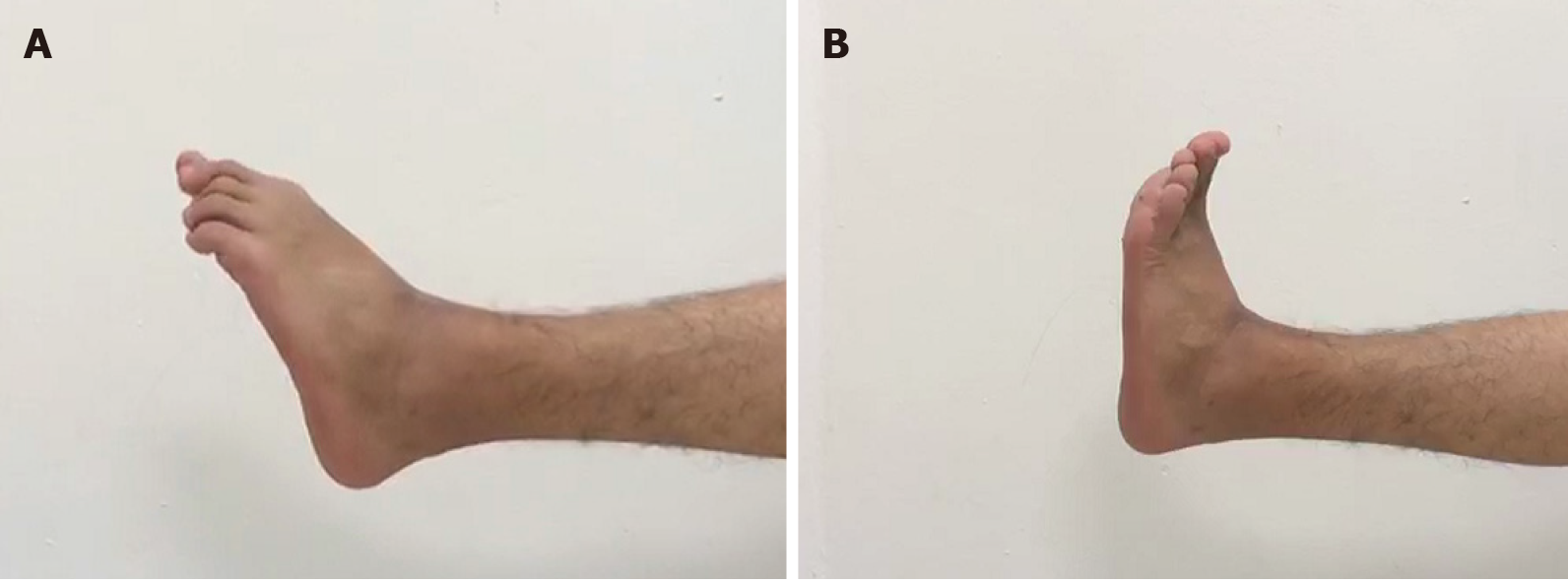
Figure 7 Postoperative range of motion (12 mo).
A: Extreme plantar flexion position; B: Extreme dorsiflexion position
- Citation: Yang QD, Mu MD, Tao X, Tang KL. Three-dimensional printed talar prosthesis with biological function for giant cell tumor of the talus: A case report and review of the literature. World J Clin Cases 2021; 9(13): 3147-3156
- URL: https://www.wjgnet.com/2307-8960/full/v9/i13/3147.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i13.3147