Copyright
©The Author(s) 2021.
World J Clin Cases. Jan 6, 2021; 9(1): 267-273
Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.267
Published online Jan 6, 2021. doi: 10.12998/wjcc.v9.i1.267
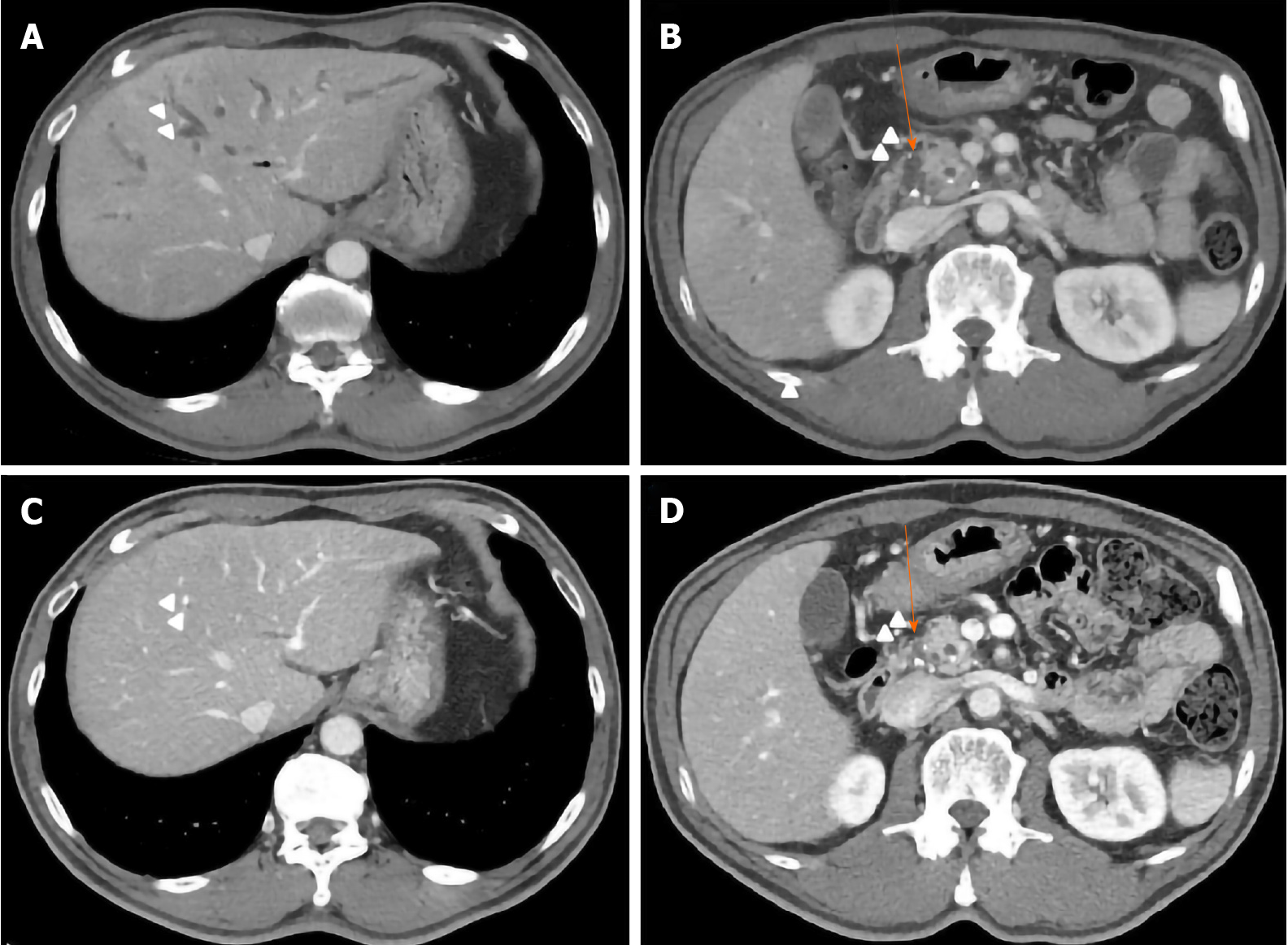
Figure 1 Computed tomography results.
A: Intrahepatic duct (IHD, arrows); B: Common bile duct (CBD) dilatation without a definite obstructive lesion (arrows). After 3 mo of high-dose glucocorticoid therapy; C: IHD dilatation with intraductal soft tissue attenuation had disappeared; D: CBD dilatation with mild luminal narrowing was reduced.
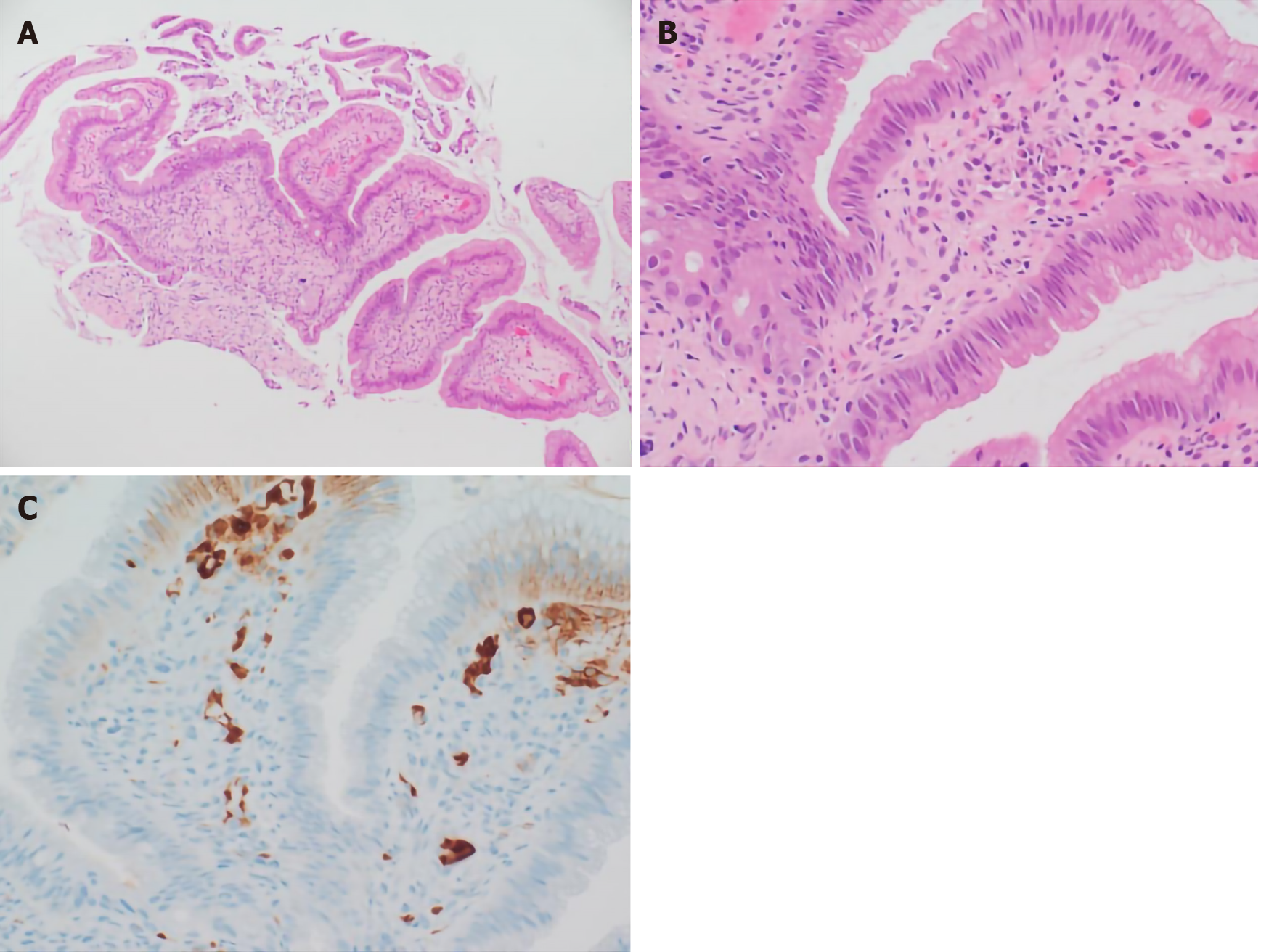
Figure 2 Histological assessment of biopsy specimen.
A: Biopsy of the ampulla of Vater showed inflammatory cell infiltration and granulation tissue [hematoxylin and eosin (H&E) stain, × 100 magnification]; B: Many plasma cells were observed in the subepithelial stroma (H&E stain, × 400 magnification); C: Immunohistochemical staining showed a large number of IgG4 positive cells (brown, × 400 magnification).
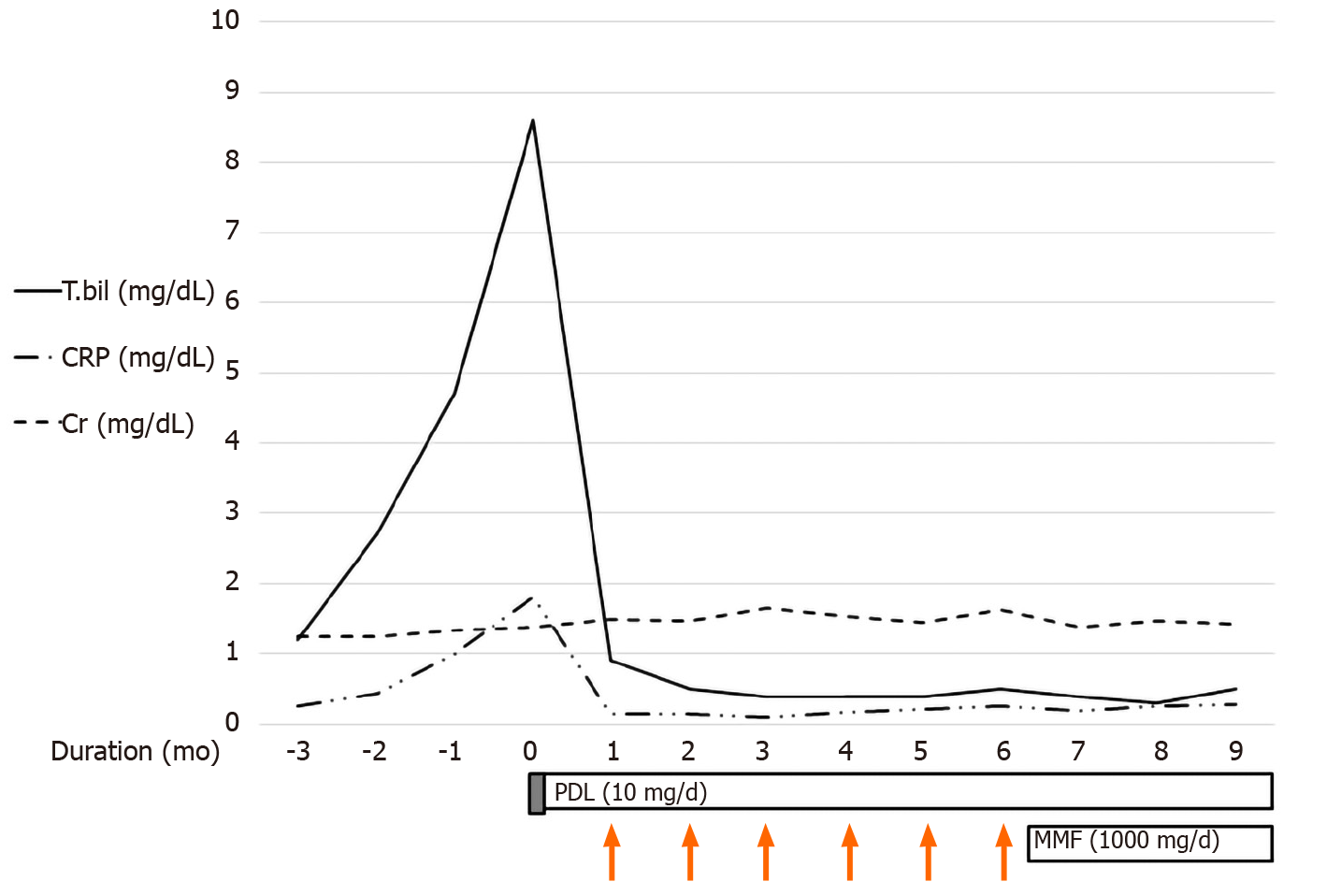
Figure 3 The initial laboratory findings indicated obstructive-pattern jaundice.
Bilirubinemia (8.6 mg/dL) and a high C reactive protein (CRP) level (1.81 mg/dL) were noted. We applied high-dose systemic glucocorticoid (GC) for 3 d (prednisolone 0.5 mg/kg/d). After GC pulse treatment, the bilirubinemia and elevated CRP level had improved so we decided to administer CYC pulse therapy (1000 mg/mo, 6 mo). The maintenance therapy was prednisolone (5 mg/d) and mycophenolate mofetil (1000 mg/d). CRP: C reactive protein; MMF: Mycophenolate mofetil.
- Citation: Kim JS, Choi WH, Lee KA, Kim HS. Immunosuppressant treatment for IgG4-related sclerosing cholangitis: A case report. World J Clin Cases 2021; 9(1): 267-273
- URL: https://www.wjgnet.com/2307-8960/full/v9/i1/267.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i1.267